1.General information
First of all, let’s define, as always, the terminology. Paralysis is complete and unconditional immobility of an organ or system for which motor activity is the main natural function. This is the inability of the patient to cause such activity "from within" - neither by conscious nor unconscious effort of will, while from the outside, for example, a paralyzed leg can be rotated at the hip joint or bent at the knee with the help of one's own hands or the hands of another person. This is the difference between paralysis, say, muscle spasm or joint contracture, when such movement is impossible in principle; The term “paralysis” emphasizes precisely the inability of the affected organ to carry out the command of the central nervous system.
Paresis translated from Greek means “weakening, loss of strength”; this term refers to incomplete paralysis (which, by the way, is also translated as “relaxation”), when the available muscle effort or the original range of possible movements is partially preserved; the degree of this preservation can vary widely.
As a synonym for the concept of “paralysis”, the term “plegia” (“stroke”) is often used, which is semantically close to the concepts of “apoplexy” and “stroke” - which apparently formed the etymological basis of the outdated Russian phraseological units “suffered a blow” ", "paralysis after a blow", "apoplexy", etc. However, in modern medical terminology, the word "plegia" is usually used with qualifying prefixes: hemiplegia (one-sided paralysis), mono-, para- or tetraplegia (respectively, paralysis of one , both same-level or all four limbs).
A must read! Help with treatment and hospitalization!
Causes and risk factors
Hemiparesis can have a primary or secondary origin - develop as an independent disease or be a consequence of another disease, or be one of its symptoms. It can also be diagnosed during the recovery period after hemiplegia. It is easier to determine the cause by the location of the problem, specifying which side is affected - left or right.
The most likely causes of hemiparesis are:
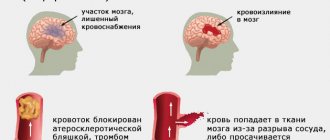
- stroke - blockage or rupture of blood vessels in the brain followed by hemorrhage;
- benign or malignant tumors – during the growth process they compress nearby tissues and damage healthy cells;
- traumatic brain injuries - bruises, concussions are accompanied by the death of tissue areas;
- encephalitis is a large group of infectious diseases accompanied by inflammation of the brain and neurological disorders;
- epileptic conditions - especially dangerous when the next attack ends with a spasm of skeletal muscles, which inevitably leads to paralysis;
- migraine is a severe headache of unknown etiology that can cause hemiparesis only in particularly severe cases;
- multiple sclerosis – contributes to the destruction of the protective membranes of the nerves, causing their damage;
- atrophy of brain tissue - this process causes the death of neurons, which inevitably leads to disturbances in the sensitivity of parts of the body;
- diabetes mellitus – its severe course causes convulsive contraction of cerebral vessels;
- cerebral palsy - in this case, hemiparesis is considered congenital, acquired in utero or during childbirth.
2. Reasons
In the most general form, the cause of paralysis and paresis can be formulated as a violation of the interaction between the central nervous system (brain and spinal cord) and the peripheral executive system (skeletal, intestinal, bladder, sphincter and other muscle systems).
In turn, such a violation can be caused by three global factors:
- failure of the central nervous system itself (for example, in dystrophic-degenerative diseases, various atrophic, oncological, inflammatory processes, ischemic and hemorrhagic strokes, mechanical lesions of the motor areas of the cerebral cortex and/or motor neurons of the spinal cord);
- end organ failure (for example, with muscle atrophy, severe ruptures of muscle-ligamentous structures or poisoning with certain poisons, mainly plant ones, which are notorious for their ability to cause total muscle paralysis and painful death from suffocation and/or cardiac arrest);
- failure of the communication system is, in fact, a breakdown of the connection between the central nervous and muscular systems: in this case, the fully functional final “performer” simply does not receive activating nerve impulses (traumatic, atrophic, etc. damage or damage to neuronal conduction channels).
The so-called is sometimes considered as a relatively independent form. “sleeping” or hypnopompic (“on awakening”) paralysis. This state, caused by a disruption or failure of sleep phases, can last up to several minutes and is usually accompanied by panic vital horror (sudden awareness in reality of one’s absolute immobility, defenselessness and helplessness), as well as vivid, frightening hallucinations (“aliens”, “intruders”, “rapists”) ", "killers", etc.), sometimes with a complete tactile illusion of actions performed in relation to the paralyzed person. Mainly from here, we note, comes a small but steady flow of quite sincere statements about “alien abductions”, “contacts with demons”, as well as absurd (but sometimes causing very real and serious troubles) accusations of robbery and rape. The mechanism for the development of this condition is due to the fact that in the REM sleep phase, motor activity should be turned off automatically; this is a normal, physiologically justified, protective paralysis (otherwise, somnambulism develops, orally “sleepwalking,” i.e., sleepwalking in various variants and forms). However, under unfavorable conditions (situations of chronic stress combined with sleep deficiency, some mental disorders, narcolepsy, i.e. pathological drowsiness, etc.), the reverse activation of motor functions is delayed, and awakening occurs earlier, in the “fast” phase.
Visit our Neurology page
Symptoms of manifestation
Paralysis is manifested by a change in muscle tone, with central genesis towards spasm, a decrease in muscle strength and normal reflexes and the appearance of things that are not characteristic of humans. The sensitivity of the legs changes, they do not feel pain and there is no sensation of the ground, the placement of the legs when stepping has to be controlled by vision. Afterwards, atrophic changes in muscles and skin occur. Often, lack of movement is accompanied by dysfunction of the pelvic organs: lack of independent urination and defecation.
- Rate of development of paralysis
Acute paralysis develops with injury and stroke; in all other cases, symptoms appear over time and gradually increase. If after the injury there are no signs of functional recovery within two days, then there is every reason to suspect a violation of the integrity of the spinal cord.
- Differences between central and peripheral paralysis
Lower paraparesis or paraplegia is more often caused by damage to the spinal cord, less often by the brain, and very rarely by peripheral neuropathy. If the entire leg is disabled from movement, then the paresis is of a central nature.
If paresis of the leg involves its lower part, it is associated with damage to the nerve trunk innervating individual muscle groups of the lower leg, and not with brain pathology.
Alcoholics develop paresis of both legs with impaired movement of the feet, this is a consequence of damage to large nerves.
We will call you back
Message sent!
expect a call, we will contact you shortly
3. Symptoms and diagnosis
The main symptoms of paralysis and paresis, in fact, have already been described in the introductory part. However, there are a lot of clinical nuances and significant typological features that have given rise to a number of classifications. Thus, diagnostically important indicators are the degree of immobility (from mild to deep paresis and complete paralysis), localization of lesions of the nervous system (central, peripheral) or muscle groups (for example, only extensors, only smooth muscles, etc.), the degree of preservation of sensitivity ( complete absence, paresthesia, pain, numbness), preservation and nature of reflexes, etc. However, the essence remains the same: there are no movements either in a dream, or in reality, or under the influence of sedatives, or in any specific, so-called. conditionally desirable situations (which distinguishes true paralysis or paresis, say, from hysterical astasia-abasia, which develops according to a completely different etiopathogenetic “algorithm”).
The diagnosis of “paralysis” or “paresis” itself, even in the mildest form of the latter, can be established and reliably confirmed by an experienced neurologist during a standard clinical examination: for this purpose, a number of diagnostic criteria have been developed and applied, as well as dynamic, static, reflexological tests. Establishing the causes of paralysis sometimes takes quite a long time and requires the use of one or another combination of methods that exist in the extensive diagnostic arsenal of modern medicine - from high-tech imaging and laboratory analytical equipment to experimental psychological, medical genetic and other types of special research.
About our clinic Chistye Prudy metro station Medintercom page!
Forms of hemiparesis
Based on their origin, there are two forms of hemiparesis:
- congenital;
- acquired.
Based on location, the disease is divided into:
- central hemiparesis - caused by pathology of the pyramidal tract in the area from the CGM to the anterior horns of the spinal cord;
- peripheral hemiparesis - occurs as a result of damage to the nuclei of the cranial nerves, cells of the anterior horns of the spinal cord.
The side opposite to the injury is predominantly affected by hemiparesis, which is explained by the crossing of nerves in the area where the medulla oblongata passes into the spinal cord. But there are cases of paresis on the side of the injury.
Based on the location of the lesion, the disease is classified into:
- right-sided hemiparesis is the most common variant diagnosed in adults and is accompanied by speech impairment; disorders manifest themselves in mild or severe severity;
- left-sided hemiparesis - mainly occurs in childhood, as it is one of the symptoms of cerebral palsy; this form is characterized by mental disorders.
Separately, the classification distinguishes spastic hemiparesis, which affects only the limbs on one side of the body.
According to the nature of the disease, the following are distinguished:
- acute form - developing in a short time;
- subacute – slowly progressive.
According to severity, hemiparesis is divided into:
- easy;
- moderate;
- deep.
Hemiparesis is diagnosed based on the degree of damage, taking into account the points scored:
- 5 points – motor activity is fully preserved, muscle strength is normal;
- 4 points – range of motion is completely preserved, muscle strength is slightly lost;
- 3 points – motor activity is significantly impaired, but the muscles have difficulty overcoming the force of friction, that is, the limb can come off the surface;
- 2 points – movements are minimally preserved, limbs can move along the plane without leaving it;
- 1 point – muscle activity is slightly noticeable, movements in the limbs are practically absent;
- 0 points – no motor activity, complete paralysis is observed.
4.Treatment
Ready-made recipes, protocols, treatment regimens for paresis and paralysis, universal for all possible cases and clinical situations, are, of course, impossible. The therapeutic strategy is always determined by diagnostic results and many individual indicators; it is always, if possible, etiopathogenetic (aimed at eliminating the cause) and, if possible, minimally invasive. But even with this, the only correct, approach, the result can not always be confidently predicted. Sometimes mobility is gradually restored with virtually no treatment, but the other way around also happens: the most intensive and seemingly 100% justified treatment, which has long proven its effectiveness, does not bring the desired result: paralysis remains completely or partially until the end of life, and sometimes progresses, involving everything new structures and systems (as observed, for example, with amyotrophic lateral sclerosis and other atrophic processes). In some cases, the method of choice is conservative therapy, in others the simplest, most effective and, oddly enough, safe treatment is neurosurgical intervention. Particular mention should be made of the group of physiotherapeutic and “non-traditional” methods. It is in this area, i.e. In the rehabilitation of patients with paralysis and paresis, the role of massage, exercise therapy, physiotherapy, acupuncture and other similar procedures is extremely important. However, their capabilities should be assessed sensibly, without elevating them to the rank of miracles and without forcing their use: the result may turn out to be insignificant or directly opposite to the desired one. It is equally important to be critical of the countless healers, healers, geniuses, enthusiasts and simply outright charlatans who strive under the slogans of miraculous healing.
But the main thing: at the first signs of unusual muscle weakness, numbness, decreased sensitivity, any limitation in mobility and/or range of usual movements, consult a doctor immediately. It’s really not worth waiting until a mild and possibly transient (at least curable) “paresis” turns into full-blown and irreversible paralysis.
Prevention
Right-sided and left-sided hemiparesis is always easier to prevent than to treat, so it is important to know what disease prevention involves.
Effective preventive measures are:
- timely detection and full treatment of all emerging pathologies in the body;
- mandatory screenings for expectant mothers prescribed by a gynecologist;
- giving up bad habits in order to prevent cardiovascular and endocrine diseases;
- preventing all kinds of stress and anxiety;
- normalization of the diet, enrichment with vitamins;
- moderate physical activity, according to age and health status.
And most importantly, at the first signs of hemiparesis, you should consult a doctor and not self-medicate, so as not to provoke serious complications.
Return to list
Peripheral paresis
Peripheral paresis develops when the nerve is directly damaged. In this case, disorders develop in one group of muscles that this nerve innervates. Muscle weakness may be present in only one leg or arm. The larger the nerve is damaged, the larger part of the body is affected by paresis or plegia (paralysis).
Peripheral paresis develops due to the following reasons:
- degenerative diseases of the spine, radiculitis;
- demyelinating diseases;
- nerve damage due to connective tissue diseases and vasculitis;
- compression of nerves (“tunnel syndromes”);
- nerve injuries;
- poisoning with alcohol and other toxic substances.
In the presence of peripheral paresis, muscle weakness, weakened reflexes, and decreased tone occur. Involuntary muscle twitching is noted. Over time, muscle atrophy develops (muscles decrease in volume) and contractures occur.
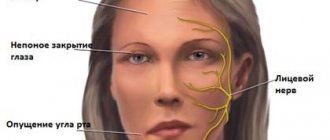
Facial paresis develops when the facial nerve is damaged. It is characterized by impaired functioning of facial muscles. Most patients have unilateral lesions, but total paresis also occurs. The main symptom indicating the progression of facial nerve paresis is facial asymmetry or the complete absence of motor activity of muscle structures on the side of the lesion.