Progressive paralysis (paralytic dementia, Bayle's disease) is an organic pathology marked by progressive disturbances in psychological and neurological activity, up to the onset of dementia. All processes can be accompanied by somatic and neurological disorders.
The likelihood of a patient developing progressive paralysis varies from 1 to 5% of all people who have had syphilis. Among other things, the male part of patients suffers from the disease more often - according to statistics, 5 times than women. The incubation period of the pathology itself is 10-15 years from the moment of infection.
The cause of the development of this disease is syphilis. However, the risks may increase with the development of other sexually transmitted diseases, such as gonorrhea.
Stages of the pathology
In its course, Bayle's disease goes through 3 stages, namely:
- Initial – its duration varies from 2 months to six months. At this stage, patients will complain of loss of strength and poor sleep, lethargy and dementia, they manifest themselves with attacks of sentimentality and excessive sleepiness during the day and insomnia at night. In the process of examining and diagnosing this stage, doctors check the blood reaction according to the Wasserman method, which, if pathology is present, will be positive. A reaction is also carried out according to Lanta, and the level of protein in the blood is increased.
- Full development stage . At this stage, patients behave inappropriately, lose their sense of tact, giving way to a feeling of euphoria and complacency, and develop inherently delusional ideas, groundless joy or tears. The patient experiences disorders that affect speech and handwriting, some may rapidly lose weight, others may, on the contrary, develop one or another degree of obesity, the face swells, and the skin turgor changes. Abscesses and damage to the body by boils, excessive fragility of bones, and degenerative lesions of the heart and liver can develop negatively. The course of this stage is diagnosed using the Wasserman blood reaction - the results will be positive, like other reactions of serological studies.
- Dementia - at this stage of the disease, the patient has a decrease in self-criticism and a weakening of his own judgments, conclusions are absurd and delusional, sometimes replaced by a feeling and state of euphoria. As the pathology progresses, the patient will lose interest in the world around him, will not respond to external stimuli and answer questions, and urinary and fecal incontinence will develop. At this stage, the patient’s limbs may become covered with ulcers, strokes may lead to death, bone fragility increases significantly, and atypical paralysis, progressive in nature, may also develop.
Symptoms
As with tabes dorsalis, with progressive paralysis one finds reflex immobility of the pupils (Argyle-Robertson symptom): the pupils either do not react to light at all, or react sluggishly and insufficiently, while the reaction to accommodation lasts longer and better. The pupils are often uneven, abnormally wide or narrow, and often irregularly shaped. The mental reaction (to pain, mental stress) also suffers; however, this disorder is not in a natural connection with either the reflex immobility of the pupils or the stage of the disease. The remaining reflexes are not characteristically changed.
In simple forms of progressive paralysis, when the control of the cerebrum weakens, the reflexes naturally increase; in forms complicated by tabes dorsalis, i.e. interruption of the peripheral-spinal reflex arc, there are no reflexes, at least on the lower extremities.
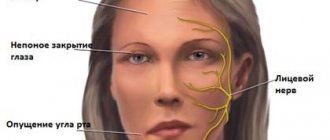
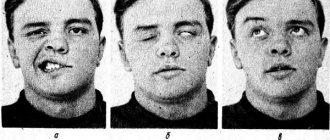
The most noticeable disorder is the coordination of muscle play, which is most noticeable in the subtle movements necessary for speech. Individual sounds are poorly formed, a number of sounds following each other are “blurred” together, the patient gets stuck on semivowels, misses some sounds and syllables, repeats or rearranges (“stumbles on syllables”), and often completely changes the sounds that make up a given word. Mental disorders are also added to this: inattention, weakness of receptivity, amnestic phenomena make it difficult to speak freely and repeat someone else’s words. The voice (especially in the last stages) becomes trembling and monotonous; Towards the end of the illness, speech becomes very slow and difficult to understand. In many cases, a decrease in the tone of the facial muscles is noticed, the nasolabial folds are smoothed out (on one side often more than on the other), more subtle facial movements disappear.
All this gives the patient’s face a sluggish and meaningless expression, by which one can recognize a paralytic from a distance. Quite early you can see twitching of individual muscle bundles on the face. The tongue sticks out hesitantly, and twitching of individual muscle bundles is noticeable.
In the same way as speech, handwriting becomes deranged. In addition to the large and uneven trembling characteristic of organic brain lesions, in the handwriting of paralytics it is also observed that the lines do not go where they should, the letters are of unequal size; instead of arcs, angles, etc. are obtained; The pen pressure is uneven. Added to this are mental difficulties: omissions, repetitions, movements of letters, syllables and words, blurring, incorrect corrections, syntactic errors, the end of the sentence does not correspond to the beginning; in the end, the result is completely illegible scribbles.
The gait disorder becomes noticeable a little later, unless the development of psychosis was preceded by tabes dorsalis with its symptoms. The foot is placed incorrectly, sometimes in front, sometimes behind, sometimes to the side of the desired place. The gait becomes irregular and unsteady; the legs are spread wide and to some extent spastically. It is often noticed that the whole body “sags” to the left and then to the right. In the final stages, patients can no longer walk at all.
Gradually, the entire musculature of the body comes into a state of spastic paralysis, the patient becomes completely helpless. Smooth muscles are also affected; swallowing becomes difficult and impossible, the intestines cannot empty their contents; fecal and urinary incontinence is observed, the latter often in conjunction with paralysis of the bladder.
Blood gives a mostly positive Wassermann reaction, cerebrospinal fluid almost always. Fluid pressure is often increased; when mixed with an equal amount of a saturated solution of ammonium sulfate, it produces a cloudiness from the presence of globulins, also contains an abnormally large amount of albumin, and in all cases without exception contains an increased number of cellular elements (hyperlymphocytosis). In this case, the presence of plasma cells is considered especially characteristic of the diagnosis of progressive paralysis.
The listed somatic symptoms should be considered the main symptoms of progressive paralysis, however, in some, albeit very rare cases, they can be very mildly expressed. Neither in the sense of time, nor in the sense of intensity do they have any definite relationship with mental disorders and can appear both before and after them. It is often possible to detect coordination disorders in the patient’s letter that preceded the disease. Pupillary disorders can be detected many years before the onset of the disease, but they may also be absent.
Of the additional somatic symptoms, paralytic seizures are the most common. They are similar to those usually observed with gross lesions of the brain: for the most part, but not always, they come suddenly, consciousness is lost, and after this there appear convulsions, partly general, partly localized, sometimes of the Jacksonian type.
The duration of the seizures varies between a few seconds and several days, and consciousness often returns before the seizures stop.
Along with these seizures, which are generally characteristic of severe brain damage, simple fainting, epileptiform and apoplectiform seizures are observed. The latter leave behind hemi- and monoplegia, mostly of a spastic nature.
Disorder of the thermal centers leads to sudden increases in temperature, sometimes lasting for days.
In addition to bone decalcification, other trophic disorders are observed. In the final stages, it is difficult to avoid bedsores; the reason for this lies not only in paralysis and untidiness, but also in impaired trophism.
Body weight is closely related to the disease: euphoric patients are well nourished until death.
At the last stage of the disease, marasmus develops.
Appetite is either excessive or decreased, depending on the patient’s basic mood. Senseless gluttony often occurs, especially in manic forms in the stage of dementia.
Sleep in a state of excitement is poor, in the calm stages before the onset of deep dementia it is mostly normal, in the last stage patients spend restless nights. Drowsiness is observed less frequently.
The sexual feeling is often affected: at the beginning, with manic forms, libido increases, then first potency disappears, and then attraction.
With progressive paralysis, like tabes dorsalis, sometimes atrophy of the optic nerve is observed, which, however, is functionally subject to large fluctuations, that is, vision becomes worse or better over the course of months; Complete blindness is observed in exceptional cases. Paralysis (mostly transient) of individual eye muscles is also not so rare, mainly in the initial stage.
Sensory symptoms in the form of headaches, ordinary and “eye” migraines, and paresthesias of all kinds are also often observed. Especially in the initial stage, they often fill out the picture of the disease, and they are interpreted as neuritis and rheumatism. Important for diagnosis is a common pain sensitivity disorder (hypalgesia or analgesia) limited to the skin.
Among the additional mental symptoms, endogenous mood swings of the manic and melancholic type should be noted; they often dominate the picture of the disease.
Hallucinations (almost exclusively auditory and visual) do not play a big role, most cases proceed without them, and only very rarely are deceptions of the senses in the foreground.
But delusional ideas are very common; usually they are closely related to changes in the affective sphere. In contrast to paranoid states, these ideas are not so fixed; especially in manic forms they are subject to great fluctuations depending on the mood and the degree of dementia; the more the patient deals with them, the more they intensify: the patient has 20 horses, as soon as he imagines this, this is not enough for him, he already has a hundred, two hundred, etc. It is also easy to instill in a paralytic a delusional idea, or to modify the ones he has : it’s worth asking him if he really didn’t have any rank in military service, and he immediately becomes a general. The delusions of paralytics are absurd both qualitatively and quantitatively (incredible exaggerations).
In some cases, severe focal symptoms, all kinds of cerebral palsy are observed (especially often there is unequal innervation in the face, especially the lower branches), aphasic and apractical disorders, etc. In later stages, symptoms of irritation appear: smacking, grinding teeth, and other convulsive, more or less coordinated movements.
Clinical forms of progressive paralysis
Each of the presented forms of the disease is marked by its own special, clinical form of the pathology, and it is on this issue that it is worth dwelling in more detail:
- Simple form - at this stage, the pathology is marked by a characteristic increase in such a symptom as dementia, accompanied by a certain carelessness, inappropriate actions, loss of a sense of tact, indifference to the environment and situation, a decrease in the ability to remember, and a weakening of memory is observed.
- Expansive - this form is characterized by the fact that the patient has an elevated mood and ideas that are absurd in their manifestation, verbosity and delusions of grandeur.
- Depressive-hypochondriacal manifestation of pathology - this stage is marked by depression and bouts of tearfulness, complaints of a hypochondriac and Cotard's syndrome.
- Agitated manifestation of the syndrome - in this case, there is pronounced motor excitability and the patient’s tendency to destruction, manifestations of attacks of aggression. But the most important thing is hallucinations that affect hearing and vision.
- Circular manifestation of pathology - when diagnosing this form of the disease, the patient exhibits manic attacks and depression, alternating attacks of lethargy and euphoria, inactivity, which is replaced by a gloomy and gloomy mood, which is replaced by a feeling of dysphoria.
- Hallucinatory-paranoid manifestation of pathology - at this stage, true manifestations of hallucination are noted, little and insignificantly systematized, quite a lot of delusional ideas in such a relationship as idea and influence, catatonic disorder itself.
- The catatonic type of the pathological course of the disease is marked in its manifestation with the so-called catatonic stupor, a certain degree of inhibition or excitement. They are, according to some psychologists, very unfavorable signs.
- Galloping and slow-onset forms of the disease . If we talk about the galloping form, it is marked by a very rapid course, when the patient expresses active motor agitation, delusions and epileptic seizures, vegetative, as well as trophic disorders, severe exhaustion and, in some cases, death. The pathological stage can last from 1-2 weeks to several months. If we talk about a slowly ongoing stage, we are talking about an atypical form of progressive paralysis. This pathological change is very rare and manifests itself as aphasic disorders and manifestations of apraxia.
- Senile paralysis - this symptom and form of pathology is most often diagnosed in patients aged 60 years or more and is characterized by a very long course, about 35-40 years, and as a result, death. This phase is very similar to the manifestations of senile psychosis.
- Infantile and juvenile paralysis is most often diagnosed in children and adolescents in the age group from 6 to 16 years. The reason for the development of this form of pathology is infection of the fetus through the placenta of the fetus from the mother with syphilis - the so-called congenital pathology. Most often, the disease manifests itself as a delay in the mental development of the child, as well as damage to the inner ear and deformation of the front teeth, and epileptic seizures.
- Taboparalysis – in this case we are talking about a combination of a progressive form of paralysis and tabes dorsalis. Symptoms of this pathology manifest themselves in the form of absence of the knee and Achilles reflexes, loss of sensitivity, depression and nihilistic delirium are somewhat less common. Symptoms can manifest themselves as a sharp loss of weight or a sharp gain in weight, the appearance of puffiness on the face, changes in facial turgor, the appearance of abscesses and boils, and excessive bone fragility.
Differential diagnosis
Differential diagnosis of manic progressive paralysis and a manic attack of manic-depressive psychosis is based on the presence of somatic symptoms, on the discrepancy between the degree of arousal and colossal nonsense, and most importantly on the absurdity of delusional ideas. A manic patient rather seems to be playing around, calling people by names other than theirs; the paralytic believes in his own fictions.
The first attack of the disease in adulthood requires great care in evaluation, even when there are no paralytic symptoms; Today they are not there, tomorrow they will be. In any case, delusional ideas are almost always clearly expressed in the manic form of progressive paralysis.
The same principles should be followed in the differential diagnosis of melancholic attacks.
It is not always easy to distinguish progressive paralysis from schizophrenia, especially if there is only a vague state of excitement with a meaningless change of ideas, a state resembling confusion, but without any specific coloring. The catatonic signs observed in this case (they can be difficult to accurately analyze in this state of the patient) do not in themselves prove the presence of catatonia; inhibition of affect and the absence of mental and affective connection with the outside world are more evident. History can often confuse matters further, since many paralytics are psychopaths even in a healthy state. In these cases, the decisive role will be played by whether it will be possible to prove (or categorically refute) that the patient has noticed a paralytic change in character from a certain moment.
To distinguish it from epilepsy, you only need to keep in mind the characteristic features of both diseases; however, when epileptic seizures first appear in middle age, they do not have a definite character in either direction; in such cases, the diagnosis remains unclear for some time.
Due to the tendency of paralytics to excesses, it is sometimes very difficult to distinguish progressive paralysis from alcoholic forms. Korsakoff's disease, being an organic psychosis, has a number of mental symptoms in common with progressive paralysis, but the difficulty is eliminated by neuritis, the absence of specific paralytic symptoms (sometimes pupillary symptoms are observed), and at times the onset of the disease. It should also be noted that neuritis is not always clearly expressed.
The distinction from brain tumors is easy for obvious reasons; however, it should be noted that slow-growing, infiltrating gliomas are encountered, which clinically present a picture of a simple form of progressive paralysis with barely noticeable local symptoms.
Progressive paralysis differs from other organic psychoses in the presence of somatic symptoms (including the composition of the cerebrospinal fluid); however, even when they are not present, a diagnosis of progressive paralysis can be made without great risk on the basis of paralytic delusions of grandeur alone.
An important task is to establish the exact boundary between progressive paralysis and neurasthenia.
All doubts about the diagnosis are dispelled by special reactions of the blood and cerebrospinal fluid to syphilis. The most famous of these is the Wassermann reaction (RW).
Symptoms of pathology
Symptoms of progressive paralysis will manifest themselves as follows:
- speech impairment and failure in the ability to connect complex words;
- a patient diagnosed with progressive paralysis loses the ability to do basic math, and his motivation decreases significantly;
- the patient's consciousness is clouded;
- memory is lost - both short-term and long-term;
- muscle atrophy and weakness are observed in the upper and lower extremities, as well as weakness in other parts of the body;
- attacks of delirium and hallucinations, increased attacks of irritability and irascibility, which are followed by attacks of depression and moodiness;
- muscle cramp.
Neurosyphilis - damage to the central nervous system by Treponema pallidum
.
It can occur at any stage of infection [8, 10]. According to temporal characteristics, early and late neurosyphilis is distinguished (before and after 5 years from the moment of infection), and its clinical forms are divided into meningeal, vascular, parenchymal and gummous [7]. Meningeal and vascular forms often occur simultaneously (“meningovascular neurosyphilis”) and are based on an inflammatory process, while the parenchymal form is currently considered as a predominantly neurodegenerative process [14]. Parenchymal forms of late neurosyphilis include tabes dorsalis
,
progressive paralysis
[]; or a combination of them [7].
Progressive paralysis appears 20-40 years after infection in individuals who have received insufficient or no treatment for syphilis. Its development is based on predominant damage to the brain substance, most often in the area of the frontal cortex; clinical manifestations include cognitive and mental disorders [16].
In recent decades, predominantly meningovascular forms have been recorded, while parenchymal forms are rare, in less than 10% of cases of untreated syphilis; in addition, the “classical” manifestations of progressive paralysis have been replaced by blurred and often monosymptomatic manifestations [2, 4-6, 9, 12]. Taking into account the fact that the last epidemic of syphilis was observed in our country in the late 90s [2, 3], an increase in the number of cases of its later forms should now be expected. Nevertheless, doctors' alertness to late neurosyphilis remains low.
In the literature of recent years there are only a few descriptions of paralytic dementia [1, 3, 6, 13, 15, 16]. This article presents a related observation.
Patient N.
, born in 1955, first turned to a neurologist in November 2011 with complaints of memory impairment, increased drowsiness, fatigue, impaired speech fluency, irritability, short-term attacks of loss of consciousness that occurred when driving a car (while driving she “blacked out” for a few seconds , then “came to her senses” and continued moving).
From the anamnesis it became known that after graduating from pharmaceutical school in 1973, the patient worked in city pharmacies as a pharmacist and analytical chemist until 2011. Until 2010, I considered myself healthy and did not see a doctor. Denies any cases of hereditary diseases in the family. Married, has two adult children.
Since November 2010, she began to notice increased irritability and short temper, attacks of jealousy, fatigue, and memory impairment; I began to cope worse with my usual work. She contacted a neurologist at a territorial clinic, was diagnosed with dyscirculatory encephalopathy and treated with vascular drugs. However, memory and behavior disorders gradually progressed, and in April 2011 she was forced to leave her job due to frequent conflicts with management who was dissatisfied with her. She did not notice any difficulties in everyday life (self-care, housekeeping, shopping), but she terminated the contract with the telephone company because she could not deal with her telephone bills and believed that she was being deceived.
In August 2011, while driving a car, short-term attacks of impaired consciousness began to occur (in the patient’s words, “blackouts”), which lasted several seconds and were not accompanied by changes in body position and convulsive phenomena. The clinic doctor ordered magnetic resonance imaging of the brain (MRI), which revealed focal lesions of the white matter with predominantly involvement of the frontal and temporal regions; The patient was referred for consultation to a multiple sclerosis specialist. After studying the anamnesis and clinical examination, the differential diagnosis was planned to be made between a primary neurodegenerative process (frontotemporal dementia was not excluded) and vascular pathology. However, during further examination, a positive Wasserman reaction was revealed, and the patient was hospitalized in the venereology department of the Nizhny Novgorod Dermatovenerological Institute.
From the anamnesis it was additionally revealed that the patient had been married for more than 30 years. Over the past 7 years, she had regular sexual contact with another man, in whom syphilis was not detected based on the results of a clinical and laboratory examination. The patient's husband indicated that he had had casual sexual contact in the past (more than 10 years ago). Over the past 10 years, the patient and her husband have not had a blood test for syphilis. An examination of the husband revealed positive blood results for syphilis. Based on the results of the examination, the husband was diagnosed with late latent syphilis; the husband refused hospitalization and received treatment on an outpatient basis at his place of residence. Given these data, it was assumed that the patient was infected with syphilis more than 10 years ago.
During a somatic examination on November 22, 2011, no clinically significant deviations from the norm were identified. No manifestations of syphilis on the skin and mucous membranes were detected. A neurological examination on November 22, 2011 revealed mild dysarthria; No pathology of the cranial nerves, reflex disorders, sensory or autonomic disorders were noted. There were mildly expressed emotional-volitional and behavioral disorders: a complacent mood, a decrease in the ability to critically assess her condition (she considered herself healthy), some motor disinhibition.
When examining cognitive functions, it was found that the patient was clearly conscious. Understanding of speech is completely preserved, expressive speech is also preserved, but there is a violation of fluency, speech is “stumbled”, it is difficult to find the right words. Speech activity is somewhat reduced: when testing for literal verbal associations, in 1 minute he names only 8 words starting with the letter “L”; in a test for semantic speech activity, she named 16 animals in 1 minute. The handwriting is uneven, the patient misses letters in words that are difficult to write. Memory for distant events is preserved; there is moderate amnesia for recent events (I remembered the last name, but could not remember the name of the President of Russia, periodically confuses the names of doctors). When performing a 5-word memory test, immediate recall is not affected; during delayed recall, she initially remembered 4 words out of 5; after a semantic hint, instead of the correct word “truck,” she stubbornly continued to call the word “tractor.” The ability for serial counting is preserved. Analyzes plot pictures and interprets proverbs correctly and without difficulty; the ability to abstract (conceptualization test) is preserved. Performs the “fist-rib-palm” test without perseverations and errors. The clock drawing test runs without errors. Constructive and graphomotor praxis are not impaired. On trials with conflicting instructions and on a choice reaction, he makes two errors each.
Mini-Mental State Examination (MMSE) score: 28 points (wrongly named the day of the week, recalled only two during delayed recall of three words). The Frontal Battery (FAB) score was 15 points.
A general blood test revealed an increase in ESR to 54 mm/h; biochemical tests revealed no significant deviations from the norm. Blood serodiagnosis and liquor diagnostics gave positive results when conducting both non-treponemal (precipitation microreaction and complement fixation reaction with cardiolipin antigen) and specific treponemal tests (complement fixation reaction with treponemal antigen, immunofluorescence reaction with whole cerebrospinal fluid, passive hemagglutination reaction, enzyme-linked immunosorbent assay) .
Results of the CSF study dated November 24, 2011: protein 1.1 g/l; cytosis 2 cells/µl; microprecipitation reaction with cardiolipin antigen 1/8 (positive); complement fixation reaction with cardiolipin antigen 1/10 (positive); complement fixation reaction with treponemal antigen 1/10 (positive); positivity rate of enzyme immunoassay (ELISAIgG) 16.6 (positive); passive hemagglutination reaction (RPHA) - 4+, immunofluorescence reaction with whole cerebrospinal fluid (WIFc) - 4+. Duplex scanning of the brachiocephalic arteries and duplex transcranial scanning (11/30/11) did not reveal any pathology.
An ultrasound examination of the internal organs (including the kidneys and thyroid gland) on November 30, 2011 revealed no pathology. On the EEG dated November 27, 2011, her epileptiform type was noted; gross diffuse changes in the bioelectrical activity of the brain, a focus of epileptiform activity in the frontotemporal region on the right. MRI of the brain on October 29, 2011 revealed diffuse atrophic changes and demyelination (Fig. 1)
;
in T1 mode with contrast (gadolinium), no pathological accumulation of contrast agent in the affected areas was registered. Figure 1. MRI of the brain of patient N. without contrast, dated 10.29.11.
FLAIR pulse sequence in the axial plane (a-d). Diffuse atrophic changes in the cerebral cortex and both hemispheres of the cerebellum are detected; multiple cortical, subcortical and paraventricular foci of hyperintense signal without clear contours, localized mainly in the frontal lobes (thin arrow); cortical symmetrical zones in the insular lobes and temporal lobes (oval); paraventricular areas of hyperintense signal near the anterior horn of the lateral ventricles and the posterior right horn of the lateral ventricle (thick arrow). Based on the results of a clinical examination and data from instrumental and laboratory studies, a diagnosis was made: late neurosyphilis, parenchymal form, progressive paralysis, mild cognitive impairment syndrome, symptomatic epileptic seizures.
The patient received two courses of specific antibacterial therapy for syphilis (penicillin 10 million units intravenously twice a day for 14 days per course).
An examination of the patient, carried out 6 months after completion of specific treatment for syphilis, made it possible to establish significant positive dynamics in her condition. According to the patient, her mood and memory improved significantly, asthenia disappeared, and attacks of “blackout” did not recur. Indicators of cognitive functions approached normal (06/01/12): when performing a test of memorizing 5 words, immediate reproduction did not suffer; during delayed recall, I immediately remembered all 5 words without prompting. She performed trials with conflicting instructions and for a choice reaction without errors. The score on the MMSE scale was 29 points, on the FAB scale - 18. When testing for literal verbal associations, she named 18 words starting with the letter “L” in 1 minute.
A serological study of blood and CSF (05.23.12) showed a decrease in the titers of a complex of specific serological reactions (a complex of specific serological reactions, or CSR, includes a microprecipitation reaction and a complement fixation reaction with cardiolipin antigen and a complement fixation reaction with treponemal antigen). Blood CSR titers decreased by more than 4 times. In the CSF, the protein content decreased to 0.7 g/l, the CSR titers decreased by more than 2 times: microprecipitation reaction with cardiolipin antigen 1/2 (positive); complement fixation reaction with cardiolipin antigen 1/5 (positive); the reaction of complement fixation with treponemal antigen is positive.
An MRI performed on May 22, 2012: compared with the previous study (10.2011), positive dynamics were determined in the form of a decrease in the size of some foci of hyperintense signal (Fig. 2)
.
Figure 2. MRI of the brain of patient N. dated May 22, 2012.
FLAIR pulse sequence in the axial plane (a-d). Positive dynamics are determined in the form of a decrease in the size of three foci of hyperintense signal in the left frontal lobe (circle), as well as a decrease in the zone of hyperintense signal near the posterior horn of the right lateral ventricle (arrows). Cortical symmetrical zones of hyperintense signal in the temporal and insular lobes of the zone - without dynamics. The EEG dated 06/01/12 showed obvious positive dynamics: typical epileptiform activity was not recorded, although signs of paroxysmal activity remained in the right frontal region. Thus, the patient, against the background of a significant decrease in blood and CSF titers of blood and CSF, experienced a significant reduction in cognitive impairment and a reverse development of some pathological changes on brain MRI.
A peculiarity of the presented case is the occurrence of clinical manifestations of late neurosyphilis in a socially prosperous married woman aged 56 years, who had no history of sexually transmitted diseases. Specific treatment for syphilis has had a significant positive effect. Our results are consistent with the data of a number of authors [11, 13] about the possibility of reducing cognitive impairment even with late manifestations of neurosyphilis, which is probably due to the reverse development of the inflammatory component of the pathological process in the brain.
The presented case highlights the importance of timely diagnosis and treatment of neurosyphilis. Neurologists should remember that late neurosyphilis can debut with isolated cognitive impairment, simulating primary neurodegenerative and other diseases of the central nervous system. Physicians are required to be wary of syphilis as a possible cause of subacutely progressive cognitive impairment.
[]Synonyms - general paralysis
,
paralytic dementia
,
general paralysis of insane
.