Mental disorders in childhood are now not such a rare occurrence. Despite the development of medicine in general and psychiatry in particular, the number of patients with developmental features of the autism spectrum, schizophrenia and other diseases is constantly increasing.
Atypical autism is less common in children, but these statistics continue to grow. It was first identified as a separate disease in ICD-10. Previously, the concept of “autism” was used as a sign of schizophrenic disorders, psychoses, and mental retardation. This medical term has already thoroughly entered our lexicon, but not everyone knows how serious this disease is. However, the fact that a child suffering from it is considered disabled indicates the seriousness of the diagnosis.
Autism concept
Simply put, this is loneliness. The patient loses the ability to communicate with people and interact with the world around him in general. He withdraws into himself, into his own dimension, where there is no place for anyone else. From the outside it looks like a reluctance to communicate with anyone, but in fact, autistic people simply do not know how to do this.
From a physiological point of view, this is a violation of the perception of signals coming through auditory, visual, tactile and other receptors. They either do not completely reach the necessary think tanks, or do so incompletely. Accordingly, the reaction to current events changes.
Autism, or more accurately, autism spectrum disorder, is a complex developmental disorder that usually manifests itself at an early age. It is caused by pathology of the functioning of the nervous system.
High-quality restoration instead of meaningless procedures
Usually the diagnosis is made before entering school. But there is no need to rush to place your child in specialized institutions. ZPR is not a severe pathology, but a delay in the development of the nervous system. The task is to contact specialists in a timely manner. We have developed a program that is aimed at correcting and developing cognitive processes:
- Memory therapy allows you to quickly expand its volume, learn to remember new information, and operate with it.
- Thinking - building logical chains, analyzing the situation, spatial connections.
- Perception - the world around us, the training program, communication with people and peers.
- Emotional, motor, sensory areas - individual work depending on the severity of the disorders.
- Attention - the child learns to concentrate, perseverance appears, and the desire to follow generally accepted rules (school, kindergarten).
- Speech.
In case of mental retardation, the child learns to quickly adapt to new conditions. The level of isolation and aggression decreases. Close relationships are built with peers and adults. The priority is to choose a scheme that takes into account all the patient’s characteristics. Apply maximum developmental techniques, develop missing skills. Both outpatient and inpatient treatment is possible.
Symptoms
Atypical autism is more difficult to identify than its classic form, so the diagnosis is often delayed. Missed onset of the disease and late treatment has a negative impact on further results.
The most surprising and at the same time confusing factor is the huge variety and individuality of symptoms.
Common features of the disease are disturbances in social inclusion, communication and interaction with others.
At home, it is quite difficult to recognize atypical autism in children. Most often, relatives attribute certain oddities and unusual behavior to age-related changes or temperamental characteristics. They are in no hurry to contact a specialist with such problems, thereby missing the initial stage of the disease.
The distinctive factors of atypical childhood autism are:
- Age limits. This type of disorder has the peculiarity of developing not in early childhood, but at a later date - 3 years, 6–10 years, or adolescence. These are those periods of a child’s life when he experiences stress about adapting to a new team, the need to communicate with strangers, and building relationships.
- Socialization. Despite the fact that the patient is completely dependent on his parents, he reacts poorly to them. The baby may not worry about the absence of his mother or, on the contrary, show concern, and behave coldly and unkindly in front of her.
- Speech. It is either absent or reduced to the use of individual words, or, in extreme cases, phrases. Constructing sentences is too difficult a task.
- Emotional breakdown. During normal activity, absolute or selective non-contact may be observed. Intense external stimuli - bright lights, loud sounds - cause fear. Uncharacteristic, unpredictable reactions to events may occur.
- Behavior. There is a negative reaction to touch. Such children do not strive to copy adults or peers and prefer loneliness.
With normal physical development, mental retardation is most often observed.
Assessing the level of intellectual abilities can be difficult, since a diagnosis made at an early age can be corrected.
Diagnosis worsens due to disorders of the speech apparatus and communication skills. During tests, the child, as a rule, knows the solution to the problem, but does not say it.
Symptoms of logoneurosis in children
Logoneurosis is usually associated with a violation of the formation of verbal communication or speech motor skills. Often the child pronounces individual sounds incorrectly. It also happens that it is difficult for him to pronounce syllables or words. A very common symptom is stuttering in children, the treatment of which is quite amenable to correction. In advanced cases, a child with a speech disorder develops a vocabulary too slowly, it is difficult for him to remember what he has learned, and he is not able to pronounce long phrases. Severe logoneurosis in children is manifested by difficulties even with the perception and reproduction of speech.
Features of the course of the disease
Children with autism have a very difficult time mastering everyday skills that everyone takes for granted. Eating normally is difficult. They are extremely selective and picky when it comes to food. For example, a child eats only semolina porridge, and no variety of dishes will convince him to try something else. If there is no porridge, he will starve. In the end, his mother will cook it and feed him.
The toilet is another problem. Children do not see the point of going to the potty, and cannot understand why adults persistently strive for this. This happens because from early childhood they have a very weak (or no) reaction to such stimuli as:
- cold;
- wet diapers
- hunger;
- unpleasant odors;
- touch.
In play activities, toys are most often completely ignored. Instead, the child prefers to use household items. There is usually no plot of the game; only stereotypical movements are observed, such as spinning in the hands or moving from place to place. An autistic person may sniff, touch, lick a new object for a long time, move it in front of his eyes, or crawl on his knees around it.
Due to speech impairment, it is almost impossible to conduct a dialogue with the patient; he simply will not support it. However, the baby can remember fairly long phrases from films and television shows and reproduce them accurately. When you contact him with a question, he may repeat it or not respond at all.
Alalia.ru
We returned from another course of dolphin therapy. We were in Odessa, lived there in Nemo. I’ll say right away that the political situation was calm, there were no revolutionaries observed, so, a couple of times, weak rallies gathered at Duke’s.
The hotel itself is almost completed and decorated. Another building is being completed nearby, but this construction does not interfere in any way. Our therapy took place in the lower pool, where it always is. We also swam a couple of times in the new pool (in the new building), but it was a little cooler there. The therapists have all changed, Misha was not there, Sasha only got massages, Lesha doesn’t swim anymore either. The new therapists are also good and smart. We also paid for a course of speech stimulation. IMHO, the same microcurrent reflexology as in Reacentres only stimulates purely “speech” points on the hands, head, and face. Costs 100 hryvnia for 1 procedure (about 400 rubles). They also now do micropolarization. We trained and purchased equipment in St. Petersburg. We also bought a magnet for magnetic therapy. They also gave Dashka taping. Girls, if anyone doesn’t know what this is and decides to do it anyway (recommended for blood flow problems in the SHOP), then it’s better to sign up for Friday (before the weekend). I didn’t know the details, but it turned out that it was just fixing the muscles in a special way and with special patches. That is, a massage can’t be helped. And so, the patches are glued for 2-3 days. You can swim with them, they dry quickly. Well, classes with speech therapist Svetlana Alexandrovna are, as always, excellent. But I understand that she practically doesn’t work there anymore. There is a new speech therapist, she is also praised. By the way, she took training in Tomatis from Jeannot, purchased equipment and conducts classes somewhere outside of Nemo. We also went for CMT therapy to a physiotherapist in one of the hospitals. The hotel itself opened a children's room with a labyrinth and a teacher. Babysitting services are available upon prior request. We have built a gym in the new building, and the sauna should be operational soon. I understand that there will be a Finnish sauna, a steam room, and some kind of barrel still standing. They also made a cinema there, every evening they showed first some cartoon, and then films. First we ate there at the hotel. For two adults and a child we paid for 2 set meals, but this was also a lot, the portions were large. The food is delicious, no complaints. But in the second week we still abandoned these complexes (somehow we got tired of them, although the dishes were different every day) and went to Puzata Khata on Deribasovskaya. There was also an opportunity to do an EEG and Doppler. The equipment is new. We didn’t get an EEG, but we did a Doppler test (350 hryvnia), the doctor looked at everything for an hour, very carefully.
Reasons for development
The main factor in the development of early autism is considered to be a deficiency of the central nervous system. The reasons why it occurs are as follows:
- genetic predisposition;
- chromosomal abnormalities;
- organic lesions of the central nervous system in pathologies of pregnancy and childbirth;
- premature schizophrenic process;
- some congenital diseases.
Modern medicine already knows about thirty similar nuances. Therefore, pathologies such as mental retardation and autism spectrum disorders are becoming more common.
The likelihood of having a child with special psychological needs exists in every family.
The actions of various factors or their combination introduce individual characteristics into each patient. The character and type of personality also leaves an imprint on the course of the disease. Even with similar symptoms in the same situations, different children may behave differently.
Etiology of speech disorders
Our Center in St. Petersburg successfully treats logoneurosis in children. Most often, these speech disorders manifest themselves in the form of stuttering. It also happens that a child hears well, but does not begin to pronounce words clearly for a long time or has great difficulty learning to speak.
In order to successfully treat speech delay and logoneurosis in children, it is necessary to accurately establish its causes. Most often they become:
- genetic predisposition;
- brain hypoxia;
- side effects of pharmacological agents;
- birth injuries, etc.
At risk are children who have a history of:
- Organic brain damage.
- Complicated pregnancy in the mother.
- Birth during difficult childbirth.
- Skull trauma.
- Severe infectious disease, etc.
Therefore, it must be taken into account that under certain circumstances a child may develop a speech delay, then an osteopath will quickly and effectively speed up the solution to the problem.
Childhood catatonic autism
A severe form of the disorder is expressed by catatonic agitation. It manifests itself most often by the following actions:
- monotonous walking, turning into running;
- scream;
- laughter, crying;
- prolonged stereotypic movements;
- impulsiveness expressed in unexpected actions.
Motor excitation suppresses instinctive activity and is expressed by negativism, attacks of numbness or waxy flexibility. Attempts at physical influence provoke resistance, hypertonicity and a persistent desire to avoid touching.
The attack may be accompanied by the pronunciation of individual words, syllables, and sounds. At the same time, the timbre of the voice and volume are constantly changing: the child either whispers something unintelligible, then suddenly suddenly starts screaming. There is a stereotypical repetition of phrases, either clear or drawn out and blurred.
Establishing diagnosis
The sooner a disorder is identified, the faster the correct approach to it will be found, and an algorithm of actions will be built that will lead to rapprochement and establishment of contact. First of all, this is the task of parents.
Children a priori cannot be the same, but even with a discount for personality traits or upbringing, they must fit into generally accepted norms of development.
By the end of the first year of life, a child without autistic disorders should master the following basic skills:
- know your name and respond to it;
- communicate with others;
- react emotionally to various situations.
Modern diagnostic methods allow parents, even before the birth of a child, to examine a panel of genes responsible for mental retardation and the development of autistic disorders. The genetic panel makes it possible to both accurately confirm the diagnosis and further detailed examination of the patient.
If parents have not done such tests, but begin to notice autistic manifestations, medical help is clearly needed. The first authority they should contact is a child psychologist. If a negative trend is confirmed, he gives a referral to a neurologist or psychiatrist.
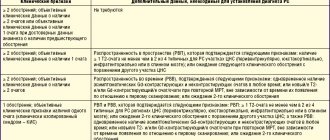
General detailed diagnostics are carried out in the following ways:
- conversation, observation of the child;
- tests, questionnaires;
- game, construction;
- MRI, CT scan of the brain;
- study of the autonomic and cardiovascular systems.
Children with autism may not respond to sound stimuli for a long time. For this reason, parents begin to suspect hearing problems. At the initial stage of diagnosis, it is important to make sure that there are no problems with auditory perception of information or to confirm them.
Program that guarantees results
Rehabilitation of children with mental retardation begins with an examination. The doctor studies documents, prescribes a set of tests, and conducts diagnostic examinations. This approach will allow us to identify the clinical picture, choose a technique, and avoid possible risks.
In our center, the child is helped to restore body functions that are impaired or completely lost. Specialists of a narrow profile work.
Procedures:
- Powerful physiotherapy - selected individually. Exercises allow you to activate hidden reserves, stimulate growth zones, and improve performance.
- Hydrotherapy is a complex of manipulations that relieves excessive stress and allows you to create a positive emotional background. Relieves spasticity and develops motor functions.
- Logotherapy - the doctor corrects problems and offers fun exercises in a playful way.
- Sensory integration gives the child a chance to learn how to build communication connections and get rid of fears and tension.
- Virtual reality stimulates thought processes, develops logical thinking, memory, and perception.
- Reflexology is a great way to activate the frontal lobe, speech and learning areas of the brain.
- Ergotherapy is a unique technique that allows a child to feel confident in everyday life. Useful skills are acquired and the correct model of behavior for a specific situation is formed.
Fine motor skills are actively developing, without which it is difficult to achieve good speech performance. The main thing is that the child does not feel pressure and does not close himself off from the doctor. We use game techniques, interesting educational materials, and modern gadgets that stimulate the treatment of mental disorders in children of different ages.
Behavior correction
A child's adaptation reserves also directly depend on the causes of autism. This should be facilitated by external factors:
- the right approach is organized;
- correctional work;
- treatment if necessary.
The best results in the fight against childhood atypical autism, the catatonic form of the disease and other autism spectrum disorders are achieved through teamwork. Positive dynamics can be achieved only with the coordinated actions of three components: all family members, medical workers, and teachers.
The patient needs to be taught social communication. Everyone who does not have such deviations sees this from early childhood in the example of parents and older children. An autistic person cannot do this; he needs a special approach and special corrective actions.
Signal therapy method in the treatment of children with enuresis
T.L. Bozhendaev ¹, ², N.B. Guseva ¹, ², N.S. Khlebutina ¹, A.I. Krapivkin ¹, V.V. Barakhta 3, A.A. Korsunsky¹
- 1 GBUZ Children's City Clinical Hospital No. 9 named after. G.N. Speransky DZM, Moscow, Russia
- 2 Department of Pediatric Surgery, Russian National Research Medical University named after. N.I. Pirogov, Moscow, Russia
- 3 Federal State Autonomous Educational Institution of Higher Education Southern Federal University, Rostov-on-Don, Russia
The presence of enuresis in children is due to various factors. This disease goes away on its own in only 5% of children; in other cases it leaves a negative imprint on the psychological and neurological state of the child. The development of this disease is due to various factors, in which one of the main roles belongs to delayed maturation of the nervous system and late development of behavioral skills. Many treatment methods have been proposed, which have their pros and cons. We offer an integrated approach using alarm therapy.
As the child grows, volitional control is formed, which is important in the formation of a conscious, mature act of urination without involuntary episodes of incontinence. Reflex urination against will occurs in newborns and infants, because... central regulation is not carried out, and the reflex arcs are closed at the level of the spinal cord.
By the age of 3–5 years, the influence of the cerebral cortex appears, which contributes to the formation of volitional control of the act of urination. The act of urination at this age becomes controlled, i.e. the child is able to regulate urination by actively contracting the sphincter and pelvic floor muscles.
Persistent involuntary urination during night sleep, inappropriate for the psychological age of the child, is called enuresis (International Classification of Diseases, 10th revision, 1995). This form of the disease, which is very common, is observed in 10–30% of cases among children aged 4 to 15 years. The largest number of children are aged 4–7 years, and only in 5% of children, with age, the manifestations of urinary disorders decrease independently. From 4–5 years of age, when a child should have developed a mature type of urination, the presence of enuresis should be detected [1, 2].
According to the Moscow Department of Health (2015), more than 20% of school-age children suffer from urinary disorders, incl. – enuresis, which helps to consider this problem extremely relevant in scientific and practical senses [3].
There are several main reasons for the development of enuresis, namely:
- Delayed maturation of the nervous system.
- Disruption of the rhythm of antidiuretic hormone secretion.
- Hereditary predisposition.
- Inflammatory diseases of the urinary organs.
- Dysfunction of the lower urinary tract.
Delayed maturation of the nervous system
Disturbances in the volitional act of urination and changes in sleep patterns are facilitated by delayed maturation of the nervous system. Pathological pregnancy and childbirth lead to early disorders of brain function, which contributes to a delay in the rate of maturation of the nervous system. Neurologists diagnose such children under the age of 1 year: the consequences of perinatal damage to the central nervous system. Disturbances in the activation and awakening reaction occur; the impulses emanating from the detrusor are insufficient to awaken the child, which causes enuresis.
A complex symptom complex of disorders of the autonomic nervous system (disorders of the hypothalamus, sympathetic trunk, mesenteric ganglion), caused by the immaturity of the nervous system, causes neurogenic dysfunction of the bladder - dysfunctional urination, characterized by a violation of the mechanisms of storage and emptying of the bladder [4].
Often, children with enuresis also have other psychological and behavioral disorders (attention deficit hyperactivity disorder). The lack of neatness skills and the anxious and suspicious personality background of children determine the high frequency of cases of enuresis in orphanages (up to 33%).
Disturbance of the rhythm of antidiuretic hormone secretion
The secretion of the hormone vasopressin (antidiuretic hormone) occurs in the hypothalamus, then it moves to the posterior lobe of the pituitary gland, where it accumulates. Its release into the blood occurs rhythmically, which contributes to less urine output at night than during the day. Overfilling of the bladder at night and, accordingly, involuntary urination is caused by a disturbance in the rhythm of the production of this hormone or its insufficiency [5].
The high effectiveness of desmopressin, a synthetic analogue of vasopressin, in enuresis proves the influence of antidiuretic hormone on the pathogenesis of this disease. Many authors explain impaired vasopressin secretion by a delay in the rate of maturation of the central nervous system in children [6].
Genetic factors
The enuresis gene is identified on chromosome 12. If one or both of a child's parents suffered from enuresis during childhood, the child's risk of the disease increases significantly. Boys suffer from enuresis more often than girls in a ratio of 4:1.
Predisposition to enuresis is not considered fatal in terms of treatment. Any patient with enuresis, according to ICCS standards, needs a comprehensive examination to identify the root cause of the disease: antidiuretic hormone deficiency, urinary tract infection, etc. With a family history of enuresis, more than 70% of children are cured with a combination of drugs and methods: desmopressin, alarm therapy , solifenacin [7].
Inflammatory diseases of the genitourinary organs
Impaired urination leads to constant dampness of underwear, which leads to infection in the urinary tract (especially in girls) [8]. Often, as a result of vulvovaginitis, girls experience urgency and frequent urination. Urge incontinence (failure to keep urine) is caused by an increase in the level of salt excretion in the urine, equally in girls and boys. Violations of the threshold of sensory activity during sleep cause daytime urinary disorders, as a result of these factors, enuresis occurs [9].
Lower urinary tract dysfunction
Overactive bladder (OAB) is a common form of lower urinary tract dysfunction. Symptoms of OAB include urinary urgency with and without urinary incontinence, accompanied by daytime pollakiuria and nocturia [10]. In most patients, the causes of urgent and frequent urination are autonomic dysfunction syndrome, residual encephalopathy and detrusor overactivity.
Neurotic complications, a negative impact on character and behavior, and the formation of future character traits initiate this disease. A very wide range of complications determines many ways to treat enuresis, but to date the problem is considered unsolved.
There are various methods of treating enuresis, each of them is aimed at one of the causes and does not take into account the entire symptom complex of the disease [11]. One of the treatment methods is based on the correction of dysfunction of the nervous system and consists of examining the internal organs to identify an imbalance of energy flows, followed by painful stimulation to obtain a response from muscle tension (RF patent No. 2123836). The disadvantage is the complexity of implementation and low efficiency.
Another method is based on developing the skill of waking up the patient when he urges to urinate, in the daytime while awake using a conditioned reflex therapy device, after reflex urination the device is turned off and the patient completes it as usual (RF patent No. 2216361). The disadvantage of this method of treatment is its low effectiveness in children with immature urination.
To consolidate the volitional control reflex at night, it is necessary for children to have a mature type of urination during wakefulness. According to our observations, immature type of urination occurs in more than half of the cases of all examined 5-year-old children with enuresis. This delay is associated both with a violation of the formation of cortical rhythms and with a delay in the consolidation of the stereotype by parents (E.L. Vishnevsky, O.B. Laurent, 2001). The treatment method we have presented and the claimed invention increase the effectiveness of treatment for children suffering from enuresis. The solution to this problem is to normalize the process of miction in the daytime, taking into account the physiological norm and to consolidate a mature urination stereotype, which, when combined with signal therapy at night, helps to strengthen the control of involuntary urination during sleep. An important condition of the task is the selection of a group of patients with immature urination and a delay in the formation of the cortical rhythm according to electroencephalography (EEG) and with treatment control using EEG
This method is as follows: during the initial visit, children with an immature type of urination are identified on the basis of urination diaries, then an EEG is performed to identify a delay in the formation of the cortical rhythm: the alpha rhythm frequency is 7 Hz, the presence of beta rhythm.
Treatment begins with behavioral therapy: individual modes of urination and fluid consumption (physiological calculation of fluid consumption of 50 ml per kg of body weight per day, taking into account daytime temperature and physical activity). The urination regime is formed in accordance with the mature type of urination with an interval of 2–3 hours between micturitions, with double forced urination before bedtime with a difference of 30 minutes
Before going to bed, the Enuflex alarm device is attached to the child’s underwear.
The bedwetting alarm clock belongs to the group of durable medical equipment (Durable Medical Equipment). It is intended for use at home.
There are three types of alarms:
- Sensor attached to panties.
- Wireless alarm.
- Signaling mat.
Type of signal: sound, light and vibration. Two components of the alarm clock: a humidity sensor and a sound analyzer. The alarm clock stimulates the patient to wake up and perform miction in response to the filling of the bladder. The moment the first drop of urine hits the laundry with the sensor attached, an alarm sounds. This type of treatment has a particularly good effect in families with stable motivation not only in the child, but also in the parents. Parental control must be maintained for 30 days. If within 7 days the child wakes up independently to a signal without parental control, it is suggested to stop monitoring night awakenings.
Treatment is carried out until the alpha rhythm is normalized to 8 Hz and the beta rhythm is stopped for at least 3 months. The formation of a mature type of urination is also monitored using diaries also after 3 months of treatment [12].
Clinical observation
Alexander B., 8 years old. Body weight 25 kg, child from the first pregnancy, which occurred with intrauterine hypoxia.
Complains of enuresis, decreased activity of the urge to urinate while awake, incontinence of urine from overflowing 1–3 times a day, decreased urge to urinate.
Parents say that the child plays around, leaks urine during martial arts training, if he does not make a gesture before training,
Diary of urination: upon urge 1-2-3 times, upon reminder 3-4 times, a total of 5-6 urinations per day. Morning portion – 170–180 ml, daily portion 100–120–180 ml. Enuresis every night. Under ultrasound control, no pathological changes in the kidneys and bladder were noted.
According to uroflowmetry: he urinates with an active stream and can accumulate up to 180 ml of urine. Uroflowmetry shows a bell-shaped curve, no residual urine.
EEG: rhythm does not correspond to age, alpha rhythm is irregular, frequency – 7 Hz.
A drinking regimen has been formed: 1300 ml/day (6 times a day, 220 ml), on training days (2 times a week) 1600 ml (6 times a day, 250 ml)
The regime of urination every 2 hours, 2 micturitions before bed with an interval of 30 minutes.
By following the urination and drinking schedule (every 2–3 hours), he began to retain urine during the day 5 weeks after the start of behavioral therapy. Along with behavioral therapy, the use of an Enuflex alarm clock device was started every night. Control of the child's awakening to the alarm by parents for 3 weeks. In the fourth week of treatment, he began to wake up on his own, steadily, when he received a signal.
After 3 months, enuresis decreased to 3 times a week. During the day, the number of sensory urinations increased to 5, and by reminder - to 2. The morning portion of urine increased to 220, but during the day it was less than the age norm of 160–180 ml, which was regarded as the persistence of an immature type of urination.
The EEG showed relief of the beta rhythm, but the alpha rhythm was within 7 Hz, which did not fully correspond to the mature cortical rhythm. Treatment was continued for another 3 months.
Control after 6 months of general treatment: the number of urinations upon urge is 6–7 out of 8. Episodes of enuresis have been reduced to 2 times a month if the drinking and urination regime is not observed. The EEG shows an alpha rhythm without bursts of pathological beta activity, frequency – 10–11 Hz. The treatment effect was regarded as positive.
Conclusion
Decreased self-esteem, emotional disorders, impact on the psychological climate in the family - this is a negative reaction to urinary incontinence in any form. A big psychological problem for a child is the formation of certain complexes that affect future adult life.
The causes of enuresis and methods of overcoming this disease should be understood by the whole family. There must be mutual understanding between the child’s parents, the doctor and the child himself.
If a child is under 5 years old and has enuresis and/or other urinary disorders (frequent urination, daytime incontinence or urine leakage, etc.), then it is important to consult a doctor (pediatrician, nephrologist and urologist). In the absence of organic pathological changes in the urinary system, educational appointments are carried out under the supervision of a doctor.
After the age of 5 years, a late onset (or secondary enuresis) is observed, which can occur either in isolation (monosymptomatic course) or with other symptoms. Various methods for correcting urinary incontinence have been proposed for several decades. There are more than 150 methods of medicinal, instrumental and physiotherapeutic treatment. Based on the immaturity of the nervous control centers, it is important to begin treatment of urinary disorders with general measures, taking into account the quality of life of the patient with urinary incontinence.
Late and irregular training of a child to conscious urination (to the potty), untimely refusal of absorbent underwear contributes to the appearance of enuresis, imperative syndrome along with genetic and pathophysiological reasons, which helps to slow down the formation of a dynamic stereotype of mature urination. Knowledge of the mechanism of urination is important for understanding the development of enuresis. The development of volitional control of urination depends on parental efforts and is one of the stages in the mental development of children, according to S. Freud.
Specialized treatment methods are required to activate the reflex arc, strengthening the behavioral response: bladder - signal - awakening - controlled urination. Thus, signal therapy is an absolute indication at the initial stage of correction of enuresis in children with immature urination and residual encephalopathy.
Topics and tags
Pediatric urology
Magazine
Newspaper "Moscow Urologist" No. 2-2020
Comments
To post comments you must log in or register