Parkinsonism or Parkinson's syndrome is a pathological condition that is manifested by stiffness in movements, involuntary trembling of the limbs and head, and constant muscle hypertonicity. As a rule, parkinsonism is associated with various organic pathologies of the brain.
Parkinson's syndrome should not be confused with Parkinson's disease - the disease is considered an independent disease with similar symptoms. And parkinsonism is a syndrome that can develop secondary (for example, after exposure to toxins, traumatic brain injuries).
Diagnosis and treatment of early stage Parkinson's disease
O.S. Levin1,2, A.V. Rosinskaya3
1Russian Medical Academy of Postgraduate Education; 2Center for Extrapyramidal Diseases (Moscow); 3Room of extrapyramidal disorders of Primorsky Regional Clinical Hospital No. 1 (Vladivostok)
Parkinson's disease (PD) is a progressive neurodegenerative disease characterized by the combination of hypokinesia with muscle rigidity and/or resting tremor, as well as later developing postural instability and a wide range of non-motor disorders, including autonomic, mental, dyssomnic and sensory symptoms. The formation of neurotoxic aggregates of the small presynaptic protein alpha-synuclein (the main component of Lewy bodies), accompanied by the death of pigmented neurons in the ventrolateral parts of the substantia nigra pars compacta, is considered to be the main link in the pathogenesis of PD. However, in recent years it has been established that only the main motor symptoms of parkinsonism correlate with damage to the substantia nigra; at the same time, the degenerative process in PD also involves other groups of neurons in various areas of the brain, as well as in the peripheral nervous system, which underlies numerous non-motor manifestations of the disease [1, 3].
Modern vision
Parkinson's disease, together with various pathological disorders of the central nervous system: Alzheimer's disease and multiple sclerosis, can be combined into a group of technocratic diseases. The causes of Parkinson's disease have not yet been fully studied, but today we can say with confidence that the disease occurs against the background of a decrease in the body's resistance, increased exposure to environmental factors, the intensity of the rhythm of life, constant stress, illiterate therapy, which creates a favorable environment for the emergence of corresponding pathological processes. Research also shows the significant role of exposure to harmful factors (toxic substances), long-term treatment with medications that affect the central nervous system: antipsychotics, barbiturates, reserpine, cinnarizine, etc., poisoning with substances: manganese, carbon dioxide, mercury. A number of episodes of severe parkinsonism have been identified in drug abusers, especially synthetic heroin. In addition to the above, viral diseases, vascular pathology of the brain, and severe and repeated brain injuries can cause the development of parkinsonism.
Epidemiology
According to a continuous population study, the prevalence of PD in Russia is 139 cases per 100,000 population, the incidence of PD is 16 cases per 100,000 population per year. With increasing age, the risk of PD increases, and the detection rate of PD among people over 65 years of age is already about 1%. Most cases of the disease occur between the ages of 60 and 70 years. However, in 15% of cases, PD debuts before the age of 45 years.
Based on the available data and the age-sex structure of the Russian population, we can roughly estimate the total number of patients with PD in our country at 210 thousand, with the disease occurring in approximately 20 thousand patients each year. Approximate calculations show that at least a quarter of patients (that is, more than 50 thousand) end up outside the scope of medical care, and most of these are patients with an early stage of the disease [3].
Symptoms of the disease
Obvious signs of a pathological condition are:
Bradykinesia. This condition is characterized by a gradual slowdown and reduction in the number of movements produced by the patient. The person looks extremely slow, the number of accompanying gestures is reduced, facial expressions become poorer, the gait becomes shuffling and is not accompanied by rhythmic movements of the upper limbs.- Muscle stiffness. Lack of relaxation of muscle fibers, leading to constant tension in the limbs. This condition manifests itself in a natural posture for the patient - any actions are performed with the limbs constantly bent at the elbow and knee joints.
- Constant trembling in the arms and legs, head vibrations. This symptom appears only if the patient is at rest; when movements are resumed, the tremor stops.
As the disease progresses, a person loses the ability to perform coordinated actions, loses control over the body, and cannot maintain a certain position for a long time. Over time, these disorders lead to complete immobility and loss of the ability to self-care. Personal and intellectual qualities also undergo changes towards degeneration.
In contrast to the primary form, after the first symptoms of the disease appear, the disease develops rapidly, followed by active progression. Disturbances in the brain occur in a bilateral, symmetrical version, while the primary type is characterized by unilateral symptoms, smoothly flowing to the second hemisphere, covering larger areas.
Parkinsonism syndrome is accompanied by signs of other brain disorders: pyramidal phenomenon, ataxia of the cerebellar zone, increasing intellectual impairment, etc. The medical history of most patients indicates the initial impact of one or another factor that provoked the disease being studied: brain injury, stroke, taking antipsychotic medications, encephalitis, etc. Often there is a significant “rollback” of the disease in the opposite direction if the root cause is identified and eliminated in time , harmful effects.
If the source of the pathology is difficult to determine, you can turn to the differentiation of symptoms. Thus, with infectious parkinsonism, the main symptoms are extreme muscle tension and autonomic disorders. In this case, the tremor may not appear at all. The anomaly, which developed as a result of oxygen starvation, is accompanied by strong vibrations of the limbs and head. With vascular disease, impairments in memory, attention, and intelligence are pronounced. Trembling in the limbs is present, but it has a small amplitude and is insignificantly expressed. The hydrocephalic phenomenon has complex, numerous symptoms: dementia, lack of control over urination, impaired sensory perception, numbness of the hands, loss of emotional stability, hallucinations.
Diagnostics
The diagnosis of PD is carried out in 2 stages. At the first (syndromic) stage, parkinsonism syndrome must be distinguished from other conditions that mimic it (Table 1).
Table 1. Conditions requiring differential diagnosis with parkinsonism.
| If there is tremor | In the absence of tremor |
| Increased physiological tremor Essential tremor Dystonic tremor Hepatolenticular degeneration | Apathetic-abulic syndrome Depression Frontal dysbasia Humeral periarthropathy Hypothyroidism Cervical osteochondrosis Dementia with the phenomenon of paratonia (continuity) Catatonia |
Identifying signs of hypokinesia is key in differential diagnosis. Initial symptoms of hypokinesia may be characterized by difficulty writing, pressing buttons on a remote control, brushing teeth, typing on a keyboard, removing small objects such as coins from a bag or pocket, putting on slippers, etc. Sometimes, already at an early stage, weakness and lag of one of the legs when walking appears with a change in the usual gait pattern. Characterized by a weakening of friendly arm movements when walking (acheirokinesis), impaired recharging of the watch (“Rolex symptom”). A weakened voice, slowness, weakening of intonation, or unclear speech may be noticed (especially when pronouncing morphologically complex words quickly). When examined to identify hypokinesia, the patient is asked to perform certain movements for about 20 seconds at the fastest pace and with maximum amplitude. In this case, the doctor should pay attention to the slow initiation of movement, asymmetry of movements, but most importantly - to a special form of exhaustion of movements (decrement), which, as they are repeated, become increasingly slower, decrease in amplitude, and require more and more effort from the patient. The phenomenon of exhaustion can be detected in all movements assessed, but is sometimes noted only in one of the tests. It should be borne in mind that the slowness and awkwardness of movements characteristic of patients with parkinsonism at an early stage can be confused with manifestations of pyramidal and cerebellar insufficiency, as well as severe depression, however, these conditions are not characterized by a decrement of movements as they are repeated. It should be borne in mind that hypokinesia can be difficult to detect against the background of severe tremor in a limb, however, even in this case it is important not to miss a diagnostically significant phenomenon: with parkinsonism, after performing a test for hypokinesia, the patient often holds his hand in a fixed, tense position and is not able to quickly relax.
Muscle rigidity is manifested by stable (as opposed to spasticity) resistance to passive movements in the wrist, elbow, shoulder, knee joints, as well as in the neck, and subjectively by stiffness and unpleasant painful sensations in the limbs. In some patients, when checking their tone, the “gear wheel” phenomenon is revealed. Rigidity should be distinguished from the phenomenon of resistance (gegenhalten), characteristic of patients with dementia and damage to the frontal lobes. Counter-containment changes rapidly depending on the direction and speed of passive movement.
Slow (3–4 Hz) resting tremor in one arm or leg is one of the common initial manifestations of parkinsonism. The presence of a classic resting tremor of the “rolling pills” or “counting coins” type is most characteristic of PD. To identify latent tremor, the patient is asked to make movements with the other hand, walk around, and perform a distraction task (for example, subtracting from 100 by 7). To identify tremors in the leg, you need to examine the patient in a sitting or lying position. However, in the absence of hypokinesia, rest tremor does not allow diagnosing either parkinsonism or PD. It should be taken into account that, on the one hand, essential and dystonic tremor can be observed at rest, on the other hand, postural and kinetic tremor is often observed in PD.
The initial manifestation of PD, especially in young people, may be foot dystonia, which appears or worsens when walking, and much less often - dystonia of other localization.
Early non-motor disorders. Starting from the earliest (prodromal) stage of the disease, the patient may be bothered by emotional depression, increased irritability, fatigue or a feeling of constant fatigue, as well as autonomic disorders such as sweating disorders (“defective thermostat”), for example, profuse sweating in cold weather, and also a tendency to constipation, frequent and/or imperative urination, increased drooling at night (the “wet pillow” symptom), erectile dysfunction. Hypoosmia often occurs already in the premotor stage of PD, but rarely attracts the attention of the patient himself, and a formalized study is necessary to identify it (using special techniques, for example, the University of Pennsylvania Olfactory Test - UPSIT). Identifying signs of rapid eye movement sleep behavior disorder syndrome (anxious dreams, vocalizations, sleep-talking, movements reflecting the content of dreams), which may precede other manifestations of the disease for many years, may be of important diagnostic importance. These non-motor manifestations may improve the accuracy of diagnosis based on early motor symptoms of the disease.
The debut manifestations of PD are also chronic pain syndromes, most often in the back and scapulohumeral region, associated with increased muscle tone, limited mobility and postural disorders.
Already at an early stage, signs of mild cognitive impairment may be detected, in particular instability of attention and slowness of thinking, difficulty finding words (the “tip of the tongue” phenomenon).
"Red flags". The second stage - the stage of nosological diagnosis - comes down to the differential diagnosis of PD with other nosological forms of parkinsonism. It requires a clinical assessment of the history and neurological examination findings. It is important to clarify the drug history. Drugs such as metoclopramide, sodium valproate, cinnarizine, amiodarone can cause drug-induced parkinsonism. Discontinuation of the drug that triggered the development of parkinsonism may not lead to immediate regression of symptoms. Sometimes, after taking the drug and a short-term improvement, the condition worsens again, which indicates a latently developing degenerative process that was “unmasked” by the side effects of the drugs.
A neurological examination may reveal symptoms that are atypical for PD, requiring the exclusion of other diseases that cause parkinsonism. Among them are: symmetry, rapid progression of symptoms with early loss of the ability to move within 5 years, early development of postural instability with falls, lack of a persistent positive effect of adequate doses of levodopa, early development of autonomic failure, rapid onset of dementia (within 1- year), limited mobility of the eyeballs (especially paresis of downward gaze), early development of severe pseudobulbar syndromes, axial dystonia, pyramidal and cerebellar signs, the presence of focal disorders of cortical functions.
Diagnosis and treatment of parkinsonism at the Yusupov Hospital
Only after finding out the nature of the disease, neurologists at the Yusupov Hospital prescribe treatment to patients depending on its cause and severity of symptoms. Is there a cure for Parkinson's syndrome? Some types of secondary parkinsonism are potentially reversible: neuroleptic parkinsonism (treated with medication), parkinsonism with hydrocephalus, or a space-occupying lesion is treated surgically, parkinsonism due to Wilson's disease with the modern administration of drugs that promote the formation of chelating complexes. Difficult to control parkinsonism are diseases of the parkinsonism+ group, in which, along with a lack of synthesis and transport of dopamine, postsynaptic structures carrying dopamine receptors often suffer.
After therapy, patients’ quality of life improves, the severity of symptoms decreases, and their ability to work is partially restored. You can get a consultation with a neurologist by making an appointment in advance by calling the Yusupov Hospital.
Additional research methods
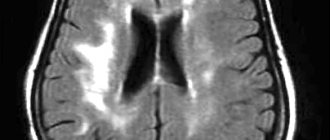
At the moment, there are no laboratory or instrumental research methods that would be mandatory for every patient with suspected PD. In recent years, patients with PD have often undergone CT or MRI of the brain, but most often this is not necessary, and in most cases the diagnosis can be made based on clinical findings. However, if the clinical picture in a patient with parkinsonism syndrome deviates from the classic variant characteristic of PD, in particular, there is no typical response to dopaminergic drugs, then neuroimaging is necessary.
When the onset of the disease is before 50 years of age, it is important to exclude hepatolenticular degeneration, which may be indicated by a corneal Kayser-Fleischer ring, low ceruloplasmin levels, increased signal intensity from the basal ganglia and cerebellum on T2-weighted MRI images, and increased urinary copper excretion.
Transcranial sonography of the deep structures of the brain may also have diagnostic significance, revealing in PD hyperechoic changes in the projection of the substantia nigra, associated with the accumulation of iron and established in 92% of cases of clinically probable PD, but its results can only be interpreted in a clinical context.
Of the practically important, but not yet available in our country, diagnostic methods include positron emission tomography (PET) and single-photon emission computed tomography (SPECT), which make it possible to study synaptic transmission at all levels, as well as monitor the pathological process. When detecting a decrease in the accumulation of F18-fluorodopa with PET and β-CIT with SPECT in the striatum, we can talk about the involvement of presynaptic nigrostriatal terminals in the pathological process (primary parkinsonism). Determination of decreased accumulation of 11C-raclopride (D2 receptor ligand) in PET will indicate a decrease in the number of dopamine receptors in the striatum (parkinsonism “plus”).
Causes of parkinsonism
With parkinsonism, changes occur in the structures of the brain: in particular, degeneration of cells in the substantia nigra of the brain. It is this structure that is responsible for muscle tone, regulates motor function, with its participation the processes of breathing and cardiac activity occur, and vascular tone is maintained.
Many factors can provoke these changes: infectious diseases, atherosclerosis, poisoning with various substances, including carbon monoxide, lead, mercury. The hereditary factor also plays a certain role, but in this case parkinsonism begins earlier, including in adolescence.
General principles for starting treatment
Since at the moment the ability to slow down the process of degeneration due to the neuroprotective effect (the ability to protect intact cells from damage) or the neuroreparative effect (the ability to restore the activity of partially damaged cells) has not been convincingly proven in any of the drugs used, treatment is still based on symptomatic action. However, the potential for a neuroprotective effect, supported by experimental or clinical data, should be taken into account when prescribing treatment.
Currently, a widely accepted concept emphasizes the importance of early administration of dopaminergic therapy - immediately after diagnosis - in order to more quickly correct neurochemical imbalances in the brain and support compensation processes.
If previously the need for maintaining monotherapy as long as possible was emphasized, at present the advantages of this approach do not seem obvious - compared with an early transition to a combination of drugs with different mechanisms of action. The need for monotherapy or combination therapy should be decided individually. In any case, when choosing drugs and their dosage, one should strive not for complete elimination of symptoms, but for a significant improvement in function, allowing one to maintain everyday and professional activity. At the same time, you should avoid making several changes to the treatment regimen at once (for example, increasing the dose of several drugs at once or adding several drugs at once), this allows you to separately evaluate the effectiveness and safety of each of the prescribed drugs.
Principles for choosing an antiparkinsonian drug
The choice of drug at the initial stage of treatment is carried out taking into account age, severity of the motor defect, labor status, state of neuropsychological functions, the presence of concomitant somatic diseases, and the individual sensitivity of the patient. In addition to achieving optimal symptom control, the choice of drug is determined by the need to delay the development of motor fluctuations and dyskinesias (Table 2).
Table 2. Choice of drug for initial treatment of Parkinson's disease.
| Drugs | Can be used as first choice | Degree of symptomatic improvement | Neuroprotective potential | Risk of side effects | |
| Fluctuations and dyskinesias | Other side effects | ||||
| Levodopa | + | +++ | +? | ↑ | ↑ |
| Dopamine receptor agonists | + | ++ | +? | ↓ | ↑ |
| MAO B inhibitor | + | + | +? | ↓ | ↑ |
| Amantadine | + | + | +? | ↓ | ↑ |
| Anticholinergics | — | + | — | ? | ↑ |
In persons under 50 years of age with mild or moderate motor impairment in the absence of severe cognitive impairment, one of the following drugs is prescribed: dopamine receptor agonist, monoamine oxidase type B inhibitor, amantadine. For a milder motor defect, an MAO B inhibitor may be prescribed; for a more severe defect, it is preferable to start with treatment with one of the dopamine receptor agonists. Non-ergoline agonists (eg, pramipexole, ropinirole, rotigotine or pronoran) are preferred over ergoline agonists (bromocriptine, cabergoline) due to their more favorable side effect profile. If one of the dopamine receptor agonists is insufficiently effective or poorly tolerated, another dopamine receptor agonist or a drug from a different pharmacological group can be tried. A combination of a dopamine receptor agonist, MAO type B inhibitor and amantadine is rational, which should be switched to gradually, adding a drug of a new group if the previously prescribed drug did not provide the expected effect.
Anticholinergic drugs (for example, biperiden) are indicated in the presence of severe resting tremor or painful dystonia, provided that neuropsychological functions are preserved. It is advisable to add them to the combination of a dopamine receptor agonist with an MAO B inhibitor and/or amantadine, if in a relatively young patient it did not suppress tremor to the extent necessary to maintain his ability to work.
If these drugs in maximum tolerated doses and their combination do not provide an adequate state of motor functions and social adaptation of patients, levodopa is prescribed in the minimum effective dose [4].
In persons aged 50–70 years with a moderate motor defect and relative preservation of cognitive functions, treatment begins with an MAO type B inhibitor (for mild symptoms of parkinsonism) or one of the dopamine receptor agonists. In the future, it is advisable to gradually switch to a combination of a dopamine receptor agonist, an MAO type B inhibitor and amantadine (provided that it is well tolerated). Anticholinergics should generally not be prescribed to patients over 60 years of age due to the risk of cognitive decline and other side effects. If the combination of the above drugs is insufficiently effective, levodopa is added in the minimum effective dose (200–400 mg per day).
In persons aged 50–70 years with a pronounced motor defect that limits the ability to work and/or the ability to self-care, as well as in the presence of severe cognitive impairment and the need to obtain a quick effect, treatment begins with drugs containing levodopa. If small to moderate doses of levodopa (300–500 mg levodopa per day) do not provide the necessary improvement, a dopamine receptor agonist, amantadine, and an MAO B inhibitor may be added sequentially.
In elderly people (over 70 years of age), especially in the presence of severe cognitive decline and somatic burden, treatment should begin with levodopa. The age limits indicated are relative, and the general principle is rather that the younger the patient, the later levodopa should be administered. In addition, it is not so much the chronological, but the biological age of the patients that plays a decisive role.
Symptoms of Parkinsonism
Parkinsonism has a number of characteristic symptoms that make it possible to clearly differentiate this disease:
- Trembling of the limbs and head. The peculiarity is that the tremor occurs at rest and subsides when attempting to move.
- Muscle stiffness, tension, hypertonicity. It intensifies with repeated monotonous movements; it is difficult for the patient to perform them for a long time.
- A characteristic posture for parkinsonism: the back is hunched, the limbs are tucked towards the body, the head is always tilted forward.
- Unsteady, shuffling gait – the patient moves in small steps and does not lift the foot off the floor well.
- With Parkinsonism, patients often fall and lose their balance.
- Motor poverty - it is difficult to start moving, they are slow.
- Facial activity decreases.
- Speech becomes quiet and monotonous.
- The patient's memory is noticeably poorer and there are disturbances in thinking.
- Psychological disorders – low mood, tendency to criticize.
- The skin becomes greasy.
- Salivation increases, and in some patients severe drooling may be observed.
- There is another characteristic feature - a tendency to constipation, rare stools, and impaired peristalsis.
Even characteristic symptoms do not guarantee a reliable diagnosis. Therefore, it is necessary to undergo a full examination.
At CELT you can get advice from a neurologist.
- Initial consultation – 4,000
- Repeated consultation – 2,500
Make an appointment
Use of extended-release pramipexole in early PD
The development of new dosage forms of antiparkinsonian drugs that provide them with a prolonged release and allow a single dose during the day not only makes treatment more convenient, but also, by improving patient adherence to treatment, increases the long-term effectiveness of therapy. In addition, with a slow release of the drug throughout the day, a more stable concentration in the blood is achieved, which can ensure better tolerability and effective control of disease symptoms throughout the day (both during the day and at night).
A new dosage form of pramipexole with prolonged (controlled) release, which involves a single dose during the day, has been used in European countries and the USA since 2009, and in our country - since 2012. It is a matrix tablet in which the active substance is evenly distributed in a polymer matrix. In the gastrointestinal tract, the matrix absorbs liquid and turns into a gel, which uniformly releases pramipexole over 24 hours. Since pramipexole is highly soluble in a liquid medium, regardless of its pH, the active substance is released from the matrix and absorbed throughout the intestine. The rate of gastric emptying and intestinal motility do not significantly affect the effect of the drug. Absorption parameters also do not depend on whether the drug is taken on an empty stomach or after a meal [2].
When developing a new dosage form, the possibility of a simple, immediate transition from the traditional form of the drug to the new one was taken into account. The condition for this is that equal daily doses of immediate release (taken 3 times a day) and extended release (taken once a day) have the same antiparkinsonian effect. The difference between the new and traditional dosage forms of pramipexole lies only in the rate of release of the active substance. The half-life of pramipexole is the same when using both forms, but controlled release ensures longer maintenance of therapeutic drug concentrations in the blood [5].
The equivalence of equal daily doses of immediate- and extended-release pramipexole has been demonstrated in a number of clinical trials.
It is worth emphasizing the particular convenience of the new dosage form of pramipexole, which can be taken once a day, for patients with early stage PD who continue to work. To avoid side effects, the drug is prescribed by slow titration - according to the same scheme as the immediate-release drug. For this purpose, extended-release pramipexole tablets are available in several strengths: 0.375, 0.75, 1.5, 3 and 4.5 mg. Treatment begins with a dose of 0.375 mg once a day, then, subject to good tolerance, every 7 days they move to the next dose level until the optimal effect is achieved, up to a maximum of 4.5 mg/day (Table 3). After reaching a dose of 1.5 mg/day, it is sometimes advisable to titrate more slowly, since the development of the full therapeutic effect may require several weeks. The recommended dose for maintenance therapy (both in early and in advanced or late stages of the disease) can range from 0.375 to 4.5 mg/day. The most commonly used dose is 3 mg/day.
Table 3. Titration schedule for extended-release pramipexole.
| A week | Dose |
| 1st | 0.375 mg 1 time per day |
| 2nd | 0.75 mg 1 time per day |
| 3rd | 1.5 mg 1 time per day |
| 4th | 2.25 mg 1 time per day |
| 5th | 3 mg 1 time per day |
| 6th | 3.75 mg 1 time per day |
| 7th | 4.5 mg 1 time per day |
Parkinson's disease (parkinsonism)
General information
The central nervous system, including the brain and spinal cord, controls everything you do, including movement.
A person with Parkinson's disease gradually loses the ability to fully control body movements. Parkinsonism is a syndrome of progressive damage to the nervous system, manifested by a decrease in general motor activity, slowness of movements (bradykinesia), tremors, and increased muscle tone. There are Parkinson's disease - primary, or idiopathic, parkinsonism; secondary parkinsonism (vascular, drug-induced, post-traumatic, postencephalitic, etc.) and parkinsonism syndrome in degenerative and hereditary diseases of the central nervous system. The concept of "parkinsonism" applies to any syndrome in which neurological disorders characteristic of Parkinson's disease are observed. The average age of onset of PD is 55 years. At the same time, in 10% of patients the disease debuts at a young age, before 40 years. In this case, the disease is called juvenile parkinsonism. The disease occurs in children and adolescents, in this case doctors talk about juvenile Hunt's parkinsonism, which is characterized by a slow progression and classic symptoms of parkinsonism. The incidence of parkinsonism does not depend on gender (the disease occurs with equal frequency in both women and men) and race, social status and place of residence. In the later stages of the disease, the quality of life of patients is significantly reduced. With severe swallowing disorders, patients quickly lose weight. In cases of prolonged immobility, the death of patients is caused by associated respiratory disorders and bedsores. Causes of the disease
The origin of Parkinson's disease remains not fully understood, however, a combination of several factors is considered as the cause of the disease: • aging; • heredity (genetic predisposition); • some toxins and substances. Other causes of Parkinson's disease include: - viral infections leading to postencephalitic parkinsonism; - atherosclerosis of cerebral vessels; - severe and repeated traumatic brain injuries. Manifestations of Parkinson's disease Parkinson's disease, despite its relatively slow development, is a progressive disease, and pronounced manifestations may indicate later stages, since in the initial forms a latent course is likely.
In total, there are up to 8 stages of development of Parkinson's disease with progressive clinical manifestations: from the absence of obvious symptoms to complete immobilization of the patient - a specially developed scale is used to assess the condition of a particular organism. Among the symptoms of the disease are: - slow movements of the limbs; - difficulty or disappearance of facial activity; - increased muscle tone; - stoop; - pain of varying intensity; - specific tremor (shaking), decreasing or completely disappearing with action; - difficulty or loss of control over posture (frequent falls, changes in gait, etc.); - speech changes; - bladder dysfunction; - chronic depression. A patient suffering from even the initial form of the disease needs a professional examination and recommendations for an individual course of treatment, since otherwise serious consequences may arise. A peculiar flexion posture appears: the head and torso are tilted forward, the arms are half-bent, often tightly pressed to the body, the legs are half-bent at the knee joints. The gait is characterized by small shuffling steps. Sometimes complete immobility can occur quite early. There is often a tendency to involuntary run forward: if you push the patient forward, he runs so as not to fall, as if “catching up with his center of gravity.” Speech becomes quiet, monotonous, without modulation, with a tendency to fade at the end of the phrase. Many patients complain of difficulties getting out of bed and turning in bed during night sleep, which significantly disrupts not only the quality of night sleep, but also, as a consequence, the usefulness of daytime wakefulness. What you can do
The first thing you should remember is that timely and correctly selected treatment, as a rule, preserves your professional and everyday activity for many years, reducing all manifestations of the disease.
What a doctor can do
Diagnosis of Parkinson's disease is entirely based on clinical observations, because... There are no specific diagnostic tests for this disease. Drugs prescribed for Parkinson's disease do not provide a cure for Parkinson's disease, but they can relieve its symptoms. As a rule, the prescribed treatment should be continued for the rest of the patient's life to avoid recurrence of symptoms. The choice of drug and selection of dosage for each specific patient is carried out only by a specialist - a neurologist or psychiatrist! The patient and his relatives should be aware that antiparkinsonian drugs have contraindications and side effects, and only a doctor can determine the necessary treatment.
Medicines that have not been proven to be effective in PD
In clinical practice, medications are widely used whose effectiveness in PD has not been proven and which, therefore, cannot be recommended for use in this disease. First of all, these include the so-called nootropic, neurometabolic and vasoactive drugs. It is possible that some of these drugs have some therapeutic effect, but before recommending a specific drug, an adequate assessment of its effectiveness should be carried out. Specialists involved in the treatment of PD are well aware that a certain proportion of patients respond well to placebo, and this effect is not durable. Accordingly, the costs of such treatment turn out to be meaningless.
Literature
- Golubev V.L., Levin Ya.I., Vein A.M. Parkinson's disease and parkinsonism syndrome. M.: MEDpress-inform, 1999.
- Levin O.S., Fedorova N.V., Smolentseva I.G. Dopamine receptor agonists in the treatment of Parkinson's disease. Rus. honey. magazine 2000; 15–16: 643–646.
- Levin O.S., Fedorova N.V. Parkinson's disease. M.: MEDpress-inform, 2011.
- Patient management protocol. Parkinson's disease. Problem standardization in healthcare. 2005; 3: 74–166.
- Chwieduk CM, Curran MP Pramipexole extended release in Parkinson's disease. CNS Drugs 2010; 24: 327–336.
- Grosset KA, Bone, Grosset DG Suboptimal medication adherence in Parkinson's disease. Mov. Discord. 2005; 20: 1502–1507.
- Hauser R., Salin L., Koester J. Double-blind evaluation of pramipexole extended-release (ER) in early Parkinson's disease. Neurology 2009; 72(11 Suppl. 3):A412–413.
- Kvernmo T., Härtter S., Bürger E. A review of the receptor-binding and pharmacokinetic properties of dopamine agonists. Clin. Therap. 2006; 28:1065–1078.
- Mizuno Y., Yamamoto M., Kuno S. et al. Efficacy of Pramipexole Extended Release (ER) and switching from Pramipexole Immediate Release (IR) to ER in Japanese advanced Parkinson's disease (PD) patients. In: XVIII WFN World Congress on Parkinson's Disease and Related Disorders: Miami Beach, 2009: Poster 2.192.
- Möller JC, Oertel WH Pramipexole in the treatment of Parkinson's disease: new developments. Expert Rev. Neurother. 2005; 5:581–586.
- Poewe W., Rascol O., Barone P. et al. Pramipexole extended-release in early Parkinson's disease. Neurology 2011; 77:759–766.
Description and reasons for the development of pathology
The concept of secondary parkinsonism includes all cases of the syndrome of the same name, caused by various factors affecting the central nervous system, as well as developing against the background of a previously diagnosed primary disease. The secondary anomaly differs from the primary manifestations of the disease in a more acute form of manifestation of signs, accompanied by other symptoms of central nervous system degeneration. Classic Parkinson's disease is characterized by the destruction of neurons, not associated with external influencing factors, on its own. The secondary anomaly has a root cause in the form of internal and external damage, leading to the development of symptoms of parkinsonism.
About a third of patients who complain of symptoms of Parkinson's disease actually develop a secondary form. It is important for medical specialists to differentiate the two different forms, since the approaches to the treatment and recovery of patients in the two cases have significant differences. Depending on the root cause of neuronal disorders, several types of disease are distinguished:
- drug;
- post-traumatic;
- intoxication;
- posthypoxic (as a result of prolonged oxygen starvation);
- infectious;
- vascular.
The most common type of pathological condition is drug-induced parkinsonism, which develops against the background of long-term or high-dose use of antipsychotic drugs.
Also common causes of disorders in the central nervous system are:
- traumatic brain injuries of varying severity, including repeated concussions;
- viral and bacteriological infections, encephalitis, immunodeficiency virus, herpes, measles, etc.;
- intoxication with substances and gases of a chemical nature with subsequent refusal to detoxify;
- long-term use of antipsychotics, antidepressants, anticonvulsants and antiemetics;
- post-ischemic and post-stroke condition, repeated focal infarctions, chronic ischemic disease;
- suffered oxygen starvation of various etiologies;
- excessive accumulation of liquid substance inside the skull with constant compression of brain structures;
- tumor processes of benign and malignant nature, compressing the intracranial organ;
- other degenerative diseases of the central nervous system that provoke the occurrence of parkinsonism syndrome.