general information
The trigeminal nerve consists of sensory and motor fibers. It originates in the structures of the brain and is divided into three branches:
- ophthalmic: responsible for the eye, forehead and upper eyelid;
- maxillary: innervates the area from the lower eyelid to the upper lip;
- mandibular: involves the chin, lower jaw, lips and gums.
With neuralgia, one or more branches of the trigeminal nerve are affected, which determines the main symptoms of the pathology. People over 45 years of age are most susceptible to the disease, and women get sick more often than men.
Make an appointment
Causes
The causes of trigeminal neuralgia can be of different nature:
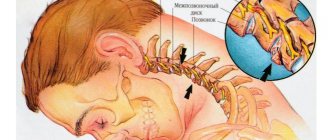
- compression of the entire trigeminal nerve or its branches against the background of: enlargement of the arteries or veins of the brain (aneurysms, atherosclerosis, strokes, increased intracranial pressure due to osteochondrosis, congenital developmental features);
- tumors of the brain or facial tissues in close proximity to nerve fibers;
- congenital anomalies of bone structure, narrowed openings through which nerve branches pass;
- injuries of the skull, facial area: bone fractures, post-traumatic scars of soft tissues;
- proliferation of scar tissue after injury, surgery, inflammation;
The risk of developing trigeminal neuralgia increases significantly:
- over the age of 50;
- against the background of mental disorders;
- with regular hypothermia;
- with insufficient intake of nutrients and vitamins into the body (anorexia, bulimia, malabsorption, etc.);
- with regular overwork, stress;
- for helminthic infestations and other helminthiases;
- for acute infections: malaria, syphilis, botulism, etc.;
- for chronic inflammation in the oral cavity (caries, gingivitis, abscesses, etc.);
- against the background of autoimmune lesions;
- with excessive exposure to allergies;
- for metabolic disorders.
What is facial neuritis
Under the influence of a number of negative factors - hypothermia, increased emotional stress, tumor processes in the brain - a narrowing of the arteries supplying the facial nerve occurs. Blood cannot move normally through the capillaries and stagnates in them.
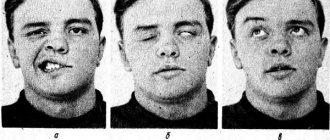
Neuritis of the facial nerve is a unilateral inflammatory lesion of the branches of the facial nerve, manifested by partial or complete disruption of facial expressions of half the face up to paralysis, as well as loss of speech, hearing and taste functions.
May be a consequence of exacerbation of herpes, hypertension, hypothermia, tumors and brain injuries, ENT pathology, multiple sclerosis, diabetes and pregnancy.
Treatment is prescribed after identifying the cause of inflammation.
As a result, significant tissue swelling occurs, which causes compression of the veins and lymphatic vessels.
The damaged nerve is deprived of normal blood supply and nutrition. Cells undergo negative changes in the absence of sufficient oxygen. The nerve trunk swells, and numerous hemorrhages appear in its structures.
According to medical statistics, in 94% of cases, damage to the facial nerve is unilateral, and only in 6% - bilateral. Sometimes pathology may indicate infectious processes in the human body.
Symptoms
The main characteristic symptom of trigeminal neuralgia is paroxysmal pain. It comes suddenly and in its intensity and speed of spread resembles an electric shock. Typically, intense pain forces the patient to freeze in place, waiting for relief. The attack can last from a few seconds to 2-3 minutes, after which there is a period of calm. The next wave of pain may come within hours, days, weeks or months.
Over time, the duration of each attack of neuralgia increases, and periods of calm are reduced until a continuous aching pain develops.
The provoking factor is irritation of trigger points:
- lips;
- wings of the nose;
- eyebrow area;
- middle part of the chin;
- cheeks;
- area of the external auditory canal;
- oral cavity;
- temporomandibular joint.
A person often provokes an attack when performing hygiene procedures (combing hair, caring for the oral cavity), chewing, laughing, talking, yawning, etc.
Depending on the location of the lesion, the pain takes over:
- the upper half of the head, temple, orbit or nose if the ophthalmic branch of the nerve is affected;
- cheeks, lips, upper jaw – if the maxillary branch is affected;
- chin, lower jaw, as well as the area in front of the ear - with neuralgia of the mandibular branch.
If the lesion affects all three branches or the nerve itself before it is divided, the pain spreads to the entire corresponding half of the face.
Painful sensations are accompanied by other sensory disturbances: numbness, tingling or crawling sensations. Hyperacusis (increased hearing sensitivity) may be observed on the affected side.
Since the trigeminal nerve contains not only sensory, but also motor pathways for the transmission of impulses, with neuralgia the corresponding symptoms are observed:
- twitching of facial muscles;
- spasms of the muscles of the eyelids, masticatory muscles;
The third group of manifestations of neuralgia are trophic disorders. They are associated with a sharp deterioration in blood circulation and lymph outflow. The skin becomes dry, begins to peel, and wrinkles appear. Local graying and even hair loss in the affected area is observed. Not only the scalp suffers, but also the eyebrows and eyelashes. Impaired blood supply to the gums leads to the development of periodontal disease. At the time of the attack, the patient notes lacrimation and drooling, swelling of the facial tissues.
Constant spasms of muscle fibers on the diseased side lead to facial asymmetry: narrowing of the palpebral fissure, drooping of the upper eyelid and eyebrow, upward movement of the corner of the mouth on the healthy side or drooping on the diseased side.
The patient himself gradually becomes nervous and irritable, and often limits himself to food, since chewing can cause another attack.
General conclusions regarding treatment algorithms
- The mechanism of nerve injury and the timing of physician response/intervention are of paramount importance in making treatment decisions for trigeminal nerve injuries. There is only 24 hours from the time the nerve injury occurs before the condition is identified to maximize the chances of recovery.
- Surgical treatment may be indicated immediately after surgery in specific cases.
- Persistent central and peripheral changes occur in the nervous system 3 months after injury that are unlikely to respond to surgical treatment.
- Based on knowledge of cellular and biochemical mechanisms, the ideal time for nerve repair is the first 2–3 weeks after injury. It is during this period that maximum restoration of sensory functions occurs.
- Long-term treatment of patients mainly includes drug and psychological algorithms.
- Counseling and support is the most useful tool for treating patients with persistent sensory problems related to nerve damage.
- Drug symptomatic therapy is indicated for patients with chronic pain or discomfort, as well as for patients with anxiety and/or depression due to chronic pain. However, due to severe side effects from groups of drugs that are aimed at treating chronic pain, less than 8% of patients remain on medications.
- Painkillers for topical use - Versatis Lidocaine patch 5% - 12 hours after 12 hours.
- Systemic painkillers - Tricyclic antidepressants (Amitriptyline and Nortriptyline), Antiepileptic drugs (Pregabalin-Lyrica or Gabapentin) - blockers of neuropathic pain, but sometimes the patient has to pay for such relief with depression and even obsessive suicidal thoughts.
- Surgical interventions: - if the intersection of the nerve is reliably known - immediate microsurgery of the nerve fiber (application of a microsurgical suture) with subsequent monitoring of early signs of regeneration of the peripheral branches of the nerves; — removal of the implant within the first 24 hours (ideally); - revision of the damaged lower alveolar nerve no later than 4 weeks after the damage, for example, with fragments of the root of the third molar or endodontic mass removed to the nerve canal; — revision surgery of the damaged lingual nerve during the first 3 months after the injury.
Diagnostics
A neurologist diagnoses trigeminal neuralgia. During the first visit, he carefully interviews the patient to find out:
- complaints: nature of pain, its intensity and localization, conditions and frequency of attacks, their duration;
- medical history: when pain attacks first appeared, how they changed over time, etc.;
- life history: the presence of chronic diseases, previous injuries and operations is clarified, special attention is paid to dental diseases and interventions.
A basic examination includes assessing the condition of the skin and muscles, identifying asymmetry and other characteristic signs, checking the quality of reflexes and skin sensitivity.
To confirm the diagnosis, the following is carried out:
- MRI of the brain and spinal cord with or without contrast: allows you to identify tumors, consequences of injuries, vascular disorders; sometimes the study is replaced by computed tomography (CT), but it is not as informative;
- electroneurography: study of the speed of nerve impulse transmission through fibers; allows you to identify the fact of nerve damage, assess the level of the defect and its features;
- electroneuromyography: not only the speed of impulse passage along the nerve bundle is studied, but also the reaction of muscle fibers to it; allows you to assess nerve damage, as well as determine the sensitivity threshold of trigger zones;
- electroencephalography (EEG): assessment of the bioelectrical activity of the brain.
Laboratory diagnostics includes only general studies to exclude other causes of painful attacks, as well as to assess the condition of the body as a whole (usually a general blood and urine test is prescribed, as well as a standard set of biochemical blood tests). If the infectious nature of the disease is suspected, tests are carried out to identify specific pathogens or antibodies to them.
Additionally, consultations with specialized specialists are prescribed: ENT specialist (if there are signs of nasopharynx pathology), a neurosurgeon (if there are signs of a tumor or injury), and a dentist.
Causes
Until now, no clear cause of the pathology has been identified. However, there are a number of factors that are associated with its possible appearance:
- virus infection . Typically, the pathogen, penetrating the human body, does not show itself with characteristic symptoms. But when the immune system malfunctions, the pathogenic element begins to actively progress and multiply.
- Hypothermia. The situation leads to a decrease in the body's resistance to the introduction of viruses and bacteria. If a person stays in a draft for a long time, this can cause vasospasm, and subsequently a disruption of the blood supply to the nerve.
- Uncontrolled consumption of alcoholic beverages. Ethyl alcohol in large quantities poisons the human body. It negatively affects not only the functioning of the brain, but also the state of the nervous system as a whole.
- High blood pressure. The condition leads to increased pressure inside the skull and trauma to the nuclei of the facial nerve.
- The period of bearing a child. Most often, compression of the facial nerve occurs in pregnant women in the 1st trimester. Hormonal changes have a negative impact on the functioning of the nervous system.
- Brain tumors. A rare but common cause of the problem. The tumor compresses the nerve fibers and impairs the passage of impulses.
- injuries . Strong blows and bruises cause damage and rupture of nerve endings. Fluid accumulates in the area of the damaged area and swelling occurs, spreading to the entire face.
- Consequences of caries in the oral cavity. Facial neuritis develops as a consequence of an infection that has penetrated from the carious cavity into the blood.
- Untreated otitis and sinusitis.
- Diabetes . When the disease occurs, the metabolism in the body is disrupted, resulting in foci of inflammation.
- Multiple sclerosis. The pathology is accompanied by destruction of the nerve sheath and the formation of sclerotic plaques in their place.
The most common cause of facial neuritis is frequent stressful situations and severe emotional shocks. Nervous stress not only contributes to inflammation of the facial muscles, but also to the development of more serious pathologies.
Treatment of trigeminal neuralgia
Treatment is aimed at:
- to eliminate the cause of damage;
- to alleviate the patient's condition;
- to stimulate the restoration of nerve structures;
- to reduce the excitability of trigger zones.
Properly selected treatment can reduce the frequency, intensity and duration of pain waves, and ideally achieve stable remission.
Drug treatment
Trigeminal neuralgia requires complex treatment using drugs from several groups:
- anticonvulsants (carbamazepine and analogues): reduce the excitability of nerve fibers;
- muscle relaxants (baclofen, mydocalm): reduce muscle spasms, improve blood circulation, reduce pain;
- B vitamins (neuromultivit, milgamma): stimulate the restoration of nerve fibers, have an antidepressant effect;
- antihistamines (diphenhydramine): enhance the effect of anticonvulsants;
- sedatives and antidepressants (glycine, aminazine): stabilize the patient’s emotional state.
For severe pain, narcotic analgesics may be prescribed. Previously, drug blockades (injecting the problem area with anesthetics) were actively used, but today this method of treatment is almost never used. It contributes to additional damage to nerve fibers.
Treatment of the root cause of the disease is mandatory: elimination of dental problems, taking medications to improve cerebral circulation, etc.
Physiotherapy and other non-drug methods
Non-drug methods complement drug therapy well and help stabilize patients’ condition. Depending on the condition and concomitant diseases, the following may be prescribed:
- ultraviolet irradiation: inhibits the passage of impulses along nerve fibers, providing an analgesic effect;
- laser therapy: reduces pain;
- UHF therapy: improves microcirculation and prevents muscle atrophy;
- electrophoresis with analgesics or antispasmodics to relieve pain and relax muscles;
- diadynamic currents: reduce the conductivity of nerve fibers, significantly increase the intervals between attacks;
- massage of the face, head, cervical-collar area: improves blood circulation and lymph outflow, improving tissue nutrition; must be carried out with caution so as not to touch trigger zones and provoke an attack; the course is carried out only during the period of remission;
- acupuncture: helps relieve pain.
Surgery
The help of surgeons is indispensable when it is necessary to eliminate nerve compression. If indicated, the following is carried out:
- removal of tumors;
- displacement or removal of dilated vessels pressing on the nerve (microvascular decompression);
- expansion of the bone canals in which the branches of the nerve pass.
A number of operations are aimed at reducing nerve fiber conductivity:
- exposure to a gamma knife or cyber knife;
- balloon compression of the trigeminal node: compression of the node using an air-filled balloon installed in close proximity to it, followed by death of the nerve fibers; surgery often leads to partial loss of sensation and decreased muscle movement;
- resection of the trigeminal node: rarely performed due to the complexity and large number of complications.
Make an appointment
Treatment
The method of treating pathology depends on its type. The primary type of disease, which arose as a result of hypothermia, is treated according to one scheme, and the secondary type, which developed due to traumatic brain injuries, according to another.
Self-medication is dangerous with complications!
Attention
Despite the fact that our articles are based on trusted sources and have been tested by practicing doctors, the same symptoms can be signs of different diseases, and the disease may not proceed according to the textbook.
Pros of seeing a doctor:
- Only a specialist will prescribe suitable medications.
- Recovery will be easier and faster.
- The doctor will monitor the course of the disease and help avoid complications.
find a doctor
Do not try to treat yourself - consult a specialist.
In general, the fight against the disease includes the use of the following groups of drugs:
- Glucocorticosteroids - relieve inflammation in the affected areas.
- Anti-inflammatory medications. Discharged only in case of severe pain symptoms.
- Diuretics . Prescribed for severe swelling of the face.
- B vitamins
In combination with taking medications, physical therapy, acupuncture, and massage are recommended. The patient is offered surgery only if the disease manifests itself in an acute form and is accompanied by intense pain.
Why can our articles be trusted?
We make health information clear, accessible and relevant.
- All articles are checked by practicing doctors.
- We take scientific literature and the latest research as a basis.
- We publish detailed articles that answer all questions.
Massage procedures to get rid of neuritis can be performed both at home and in a clinic. Gymnastic exercises are performed daily for at least 30 minutes.
The patient sits in front of a mirror and observes the movements of the inflamed part of the face, holding the healthy one. This is necessary so that most of the load falls on the affected departments.
Physiotherapeutic methods for treating facial neuritis include:
- Thermal procedures. They are used only in the initial stages of the problem.
- Paraffin applications (on the 5th-6th day of the disease).
- Ultrasound using hydrocortisone.
The minimum number of procedures is 8 sessions. After this, the neurologist makes a decision to extend the sessions or terminate them.
Acupuncture is prescribed to quickly restore damaged muscle fibers. If drug therapy, acupuncture and physiotherapeutic procedures do not bring a positive result, then the patient is offered surgery.
Complications
Without treatment, trigeminal neuralgia gradually progresses. Over time, a pathological pain focus forms in one of the parts of the brain. As a result, the pain covers the entire face, is provoked by any minor irritant and even the memory of an attack, and subsequently becomes permanent. Vegetative-trophic disorders progress:
- irreversible atrophy of the facial muscles is formed;
- teeth become loose and begin to fall out due to advanced periodontal disease;
- baldness is increasing.
Due to constant pain, the patient's sleep is disturbed and severe depression develops. In severe cases, patients may commit suicide.
Prevention
Prevention of trigeminal neuralgia is a set of simple measures that significantly reduce the risk of developing pathology. Doctors recommend:
- undergo regular preventive examinations;
- at the first signs of the disease, seek help (the sooner treatment is started, the greater its effect will be);
- eat right, get the required amount of vitamins, minerals, unsaturated fatty acids;
- regularly engage in light sports and gymnastics;
- get enough sleep and rest;
- minimize stress and physical overload;
- avoid hypothermia and harden yourself;
- to refuse from bad habits.
Treatment at the Energy of Health clinic
If you or your relative are bothered by severe pain in one or another part of the face, the neurologists of the Health Energy clinic will come to the rescue. We will conduct a full diagnosis to identify the causes of the pathology and prescribe comprehensive treatment. At your service:
- modern drug regimens to reduce the frequency and intensity of attacks;
- physiotherapeutic procedures: magnetotherapy, laser therapy, electrophoresis, phonophoresis, etc.;
- delicate therapeutic massage;
- acupuncture;
- help from a psychologist if necessary.
Advantages of the Health Energy Clinic
The Health Energy Clinic is a multidisciplinary medical center where every patient has access to:
- screening diagnostic programs aimed at early detection of diseases and pathologies;
- targeted diagnostics using modern equipment and laboratory tests;
- consultations with experienced specialists, including foreign ones;
- modern and effective comprehensive treatment;
- necessary certificates and extracts;
- documents and appointments for spa treatment.
Trigeminal neuralgia is a serious pathology that can seriously disrupt a person’s normal lifestyle. Don't let pain and fear take over your thoughts, get treatment at Health Energy.
Facial neuritis (facial nerve neuropathy)
Paralysis of the facial muscles on one side of the face (prosopoplegia) as a result of damage to the facial nerve is a common disease that requires urgent treatment.
In a large number of cases, damage to the facial nerve (FN) occurs in the bony canal (pyramid of the temporal bone), before exiting the skull through the stylomastoid foramen. Bone canal L.N. is quite narrow, which contributes to compression of the nerve in it during the formation of edema. Edema is usually caused by impaired blood supply to the nerve as a result of hypothermia or a viral infection. In the first hours after the onset of paresis of the facial muscles, therapeutic measures should be aimed at relieving swelling of the facial nerve. Otherwise, irreversible death of nerve fibers may occur. On the first day of the disease, it is important to establish the location, nature and extent of nerve damage. In the following days, the diagnosis aims to accurately establish the etiological factor - infection, ischemia, etc.
In accordance with these standards, our clinic primarily performs brain tomography (MRI, CT) and electromyographic study of L.N.
Localization of facial nerve damage
First of all, it is important to differentiate between the intracranial localization of the lesion, the lesion in the bony canal of the temporal bone and after the exit of the nerve on the face.
1. If paralysis of the facial muscles occurs simultaneously with the appearance of hemiplegia (weakness) in the limbs of the ipsilateral (same) half of the body, then we are talking about a focal lesion of the opposite hemisphere of the brain. The most likely cause is a stroke. Brain tomography in this case makes it possible to clarify the cause of hemisphere damage (tumor, multiple sclerosis?). In mild cases, tomography does not reveal lesions. In this case, EEG (electroencephalographic study) allows one to differentiate between damage to the cerebral cortex and subcortical (lacunar) strokes. We do not perform EMG in cases of hemispheric lesions.
In rare cases, limited central damage (damage to the cerebral hemispheres) appears only on the face. In this case, a simple forehead wrinkling test can exclude a central lesion. The forehead muscles receive innervation from both hemispheres. Therefore, if one of the hemispheres is damaged, the forehead muscles do not suffer. At the same time, when the facial nerve itself or its nuclei are damaged, paresis of the facial muscles of the entire half of the face, including the muscles of the forehead, is observed.
*It must be remembered that the masticatory muscles receive innervation from the trigeminal nerve system. Therefore, their function is preserved. The oculomotor muscles, innervated by the 3rd, 4th and 6th pairs of cranial nerves, are also preserved. Ptosis (drooping eyelid) is not a symptom of facial nerve damage. On the contrary, damage to the facial nerve is characterized by the inability to close the eye.
2. Damage to the nuclei of L.N. in the brainstem is usually accompanied by paralysis or paresis of the limbs of the opposite side (Millard-Hubler syndrome) and/or paresis of the abducens nerve on the same side, due to the involvement of the nucleus n. Abducens (Fauville syndrome). The latter is manifested by convergent strabismus: the inability to move the eye of the affected side to the side.
*The upward movement of the eyeball when the eyes are closed (Bell's phenomenon) is not a symptom of damage to the oculomotor nerves.
We definitely do an MRI, since MRI is better at visualizing the deep structures of the brain than CT. Brain tomography visualizes structural abnormalities. We obtain additional information about the localization of functional disorders by conducting EMG studies of the blink reflex (R1 and R2 components of the blink reflex are generated in different parts of the brainstem) and acoustic brainstem evoked potentials (Components IV are generated in different parts of the brainstem).
Most often, disorders at this level are caused by demyelinating disease, tumors, vascular malformations, syringomyelia, etc. With the sudden appearance and development of symptoms (within hours) of damage to the hemispheres or brain stem, an acute cerebrovascular accident is assumed. The patient is admitted to the intensive care unit.
3. The third variant of intracranial lesion is the lesion of L.N. along the path from the brain stem to the entrance to the bony canal of the temporal bone (porus acusticus internus) in the so-called cerebellopontine angle. Here the facial nerve follows next to the auditory nerve and the intermediate (regulates tear and salivation, carries taste fibers from the anterior two-thirds of the tongue) nerve. Therefore, with pathology in the area of the cerebellopontine angle, in addition to paresis of the facial muscles, there is deafness on the same side, loss of taste on the same side of the tongue, dry mouth and decreased tear production may be felt.
The most common causes are acoustic neuroma, vascular malformations, basal gliomas, etc. MRI is performed to verify the diagnosis. If necessary, contrast-enhanced MR angiography is performed. Throughout the entire length from the cerebellopontine angle to the exit of the facial nerve to the face, the symptoms of its damage may indicate the presence of a serious ENT pathology: purulent otitis, with the formation of a fistula, mastoiditis (inflammation of the mastoid process), etc. Therefore, in case of the specified localization of the lesion, a consultation with an ENT specialist is required in our clinic.
4. Upon entering the bony canal, the facial and intermediate nerves diverge from the auditory nerve. Therefore, with damage to the canal, deafness (if it is not associated with ENT pathology) is not observed. On the contrary, so-called hyperacusis is detected - increased sensitivity of the ear to sounds, especially high tones. This phenomenon is associated with dysfunction of the nerve fibers that run as part of the L.N. to muscle m. Stapedius of the inner ear, which regulates the adjustment of the mechanical part of the sound-receiving apparatus.
5. Symptoms of damage to the facial nerve in the bone canal of the temporal bone. As the facial nerve moves from inside to outside in the canal, the following nerve branches are successively separated from it: n. Petrosus major (lacrimation), n. Stapedius (to the muscle m. Stapedius), Chorda timpani (salivation and taste fibers). Therefore, when the nerve lesion is localized before the origin of n. Petrosus major, no lacrimation observed. Hyperacusis can be observed only when the nerve is damaged before the n. Stapedius. Dry mouth and taste disturbances occur if the nerve is affected before the Chorda timpani leaves. The latter departs from the facial nerve close to its exit from the bone canal to the outside.
Bell's palsy - paralysis of the facial muscles of half the face with the addition of these symptoms, resulting from swelling and compression of the nerve in the bone canal - the most typical case of L.N. neuropathy.
Hunt's neuralgia (Ramsey Hunt syndrome) is Bell's palsy + pain and the presence of characteristic bubbles in the area of the external auditory canal, pinna and behind the ear. Hunt's neuralgia is a sign of herpetic nerve damage. In this case, we carry out a serological blood test for Herpes Zoster.
6. After the release of L.N. outward from the stylomastoid foramen, it branches on the face. Here it is available for direct study using electromyographic methods. Typically, M-responses of the nasal muscles, orbicularis oculi and oris muscles are studied when the nerve at the exit from the stylomastoid foramen is stimulated. Identification of signs of neuropathy in the peripheral part of the facial nerve on both sides indicates the presence of polyneuropathy. In this case, an EMG study of the nerves of the limbs is performed to verify the presence of polyneuropathy.
After branching, some branches pass through the parotid gland. Tumors of the parotid gland can cause their damage.
If an EMG study is performed in the first 4 days (preferably in the first two days) after the onset of paralysis of the facial muscles, then these studies allow for differential diagnosis of lesions on the face and inside the bone canal (when topical diagnosis based on the clinical symptom complex is impossible). After 4-7 days, Wallerian degeneration of distal nerve fibers (on the face) may occur if they are damaged proximally (in the canal).
NB: Intracranial lesion indicates the presence of serious diseases that threaten to lead to damage to other parts of the brain if not diagnosed and treated in a timely manner. The first examination of the patient is brain tomography.
Neuritis of the facial nerve in the classic form, i.e. in case of damage in the bone canal and in the facial area, it also requires urgent hospitalization of the patient in a neurological hospital with immediate anti-edematous therapy, the basis of which is corticosteroids. It is important to carry out timely measures to restore nutrition and blood supply to the nerve.
*Facial nerve neuritis is a common but outdated name. More correctly, neuropathy of the facial nerve, since this concept includes not only inflammatory (neuritis) diseases, but also nerve lesions of other etiologies.
Objective criteria for the severity of facial nerve damage.
Nature of the lesion and prognosis.
Please note that slight facial asymmetry without facial muscle weakness is not a consequence of facial neuritis. Close your eyes, stretch your lips in a wide smile, whistle, wrinkle your forehead and frown - make sure that the muscles are really paralyzed.
1. The first EMG study for neuropathy of the facial nerve is recommended to be carried out in the first 4 days after paralysis. The study consists of two parts: EMG of the facial nerve and study of the blink reflex on both sides. With EMG L.N. recording is made from the facial muscles innervated by direct stimulation of the nerve in the area where it exits the bone canal. The blink reflex is recorded from both orbicularis oculi muscles when the trigeminal nerve is stimulated. The impulse along the trigeminal nerve enters the brain stem, where it switches and enters the nuclei of the L.N. on both sides. After which, from the core of L.N. the impulse travels along the entire nerve (including the bone canal) to the facial muscles.
Three typical types of lesions with neuritis of the facial nerve and their interpretation:
— deviation from the norm in EMG L.N.: lesion on the face
- normal EMG results of L.N., but the amplitude of the R1 component of the blink reflex is reduced: lesion in the bone canal - complete destruction of axons or axonotmesis (incomplete damage to the axon with the formation of a persistent block of conduction along it). Complete absence of the reflex is an unfavorable prognosis.
- normal EMG results of L.N., but the latency of the R1 component of the blink reflex is increased: demyelination of the nerve (damage to the myelin sheath). Favorable prognosis.
2. The second EMG study is recommended to be carried out 10-15 days after paralysis. The following EMG signs allow you to verify the diagnosis:
— decrease in amplitude (%) of the M-response of the facial muscles during EMG L.N. compared with the first study in proportion to (%) irreversible degeneration of nerve fibers. If the amplitude has not decreased, the prognosis for complete recovery is favorable.
— the amplitude of the M-response is preserved, but the amplitude of the reflex response is significantly reduced with normal latency: axonotmesis, restoration of nerve function may take several months (with adequate therapy).
— the amplitude of the M-response remains at the same level, but the latency of the first component of the blink reflex is significantly increased. Compared to the first study, a clear correction of the deviation of the reflex component from the norm is noted. Recovery occurs due to remyelination (restoration of the myelin sheath of the nerve). The prognosis is favorable. Recovery within several weeks with adequate therapy.
— The M-response of the facial muscles has disappeared: an extremely unfavorable prognosis. Formation of facial muscle contractures.
- The M-response has sharply decreased, the reflex response is absent in the first and second studies of the blink reflex. The prognosis is unfavorable. Recovery is possible by the sprouting of new fibers into denervated muscles with the formation of aberrant conduction (hemifacial spasm, tics).
If it is not possible to compare with the first study (late hospitalization), from 2-3 weeks from the onset of the disease, it is possible to conduct needle EMG of the facial muscles to verify axonal damage.
3. The third study is recommended to be carried out 1.5-2 months from the onset of paralysis. In addition, during the treatment process there is often a need to evaluate the effectiveness of the therapy. Then additional research is carried out on an individual basis. In addition, if the restoration of the nerve as a result of axonotmesis lasts for several months, we repeat the neurophysiological study after 3-4 and after 5-6 months.
There is no need to dramatize the situation if you notice sudden paralysis of the muscles of half the face. As a result of systematic tactics of therapeutic and diagnostic measures, timely therapy aimed at limiting the spread of the pathological process, and a pathogenetically determined approach to identifying the etiology of the disease, it is possible to achieve complete restoration of facial muscle function in the vast majority of patients. But remember: if you have neuritis of the facial nerve, you must immediately consult a doctor. Treatment and examination should be started within the first hours of the onset of the disease.
For information about making an appointment with specialists, please contact us by phone: 8;, or by email. The email address is being protected from spambots. Javascript must be enabled in your browser to view the address. / The email address is protected from spambots. Javascript must be enabled in your browser to view the address.