What is akathisia and how does it manifest itself?
Akathisia is a syndrome of chronic restlessness in adults combined with a feeling of severe internal anxiety. It manifests itself as a constant thirst for movement, in making aimless movements that can interfere with the person himself and those around him. The patient cannot sit still, he is burdened by being in a calm state, he constantly moves his legs, jumps up, walks from corner to corner along the same route. This can happen not only during the day, but even at night, when a person gets up during sleep to walk aimlessly. As a result, night sleep is disrupted, an inversion of day and night sleep occurs, and the rhythm of life and daily routine are disrupted. Gradually, this leads to the inability to live a normal life, increased anxiety, asocialization of the individual, and the development of various mental disorders.
Akathisia can occur as a side effect of taking certain medications (this will be discussed below). The syndrome is often associated with other pathologies. Initially, the term “akathisia” was introduced and described by the Czech psychiatrist L. Gaskovec as a phenomenon accompanying certain mental disorders in 1901. Later, French doctors fleshed out this theory, linking the development of akathisia with the disease of secondary parkinsonism. We were talking about a disease that occurs as a complication of encephalitis. Over time, thanks to the discoveries of scientists, the list of risks has been expanded. It turned out that people with Parkinson's disease, chronic alcoholics, drug addicts, as well as patients taking a number of psychotropic medications are often susceptible to symptoms of akathisia.
Causes
Most often, akathisia occurs as a side effect of taking psychotropic drugs. In more rare cases, the disease is caused by other reasons. Pathology may occur:
- While taking psychotropic drugs. In most cases, the syndrome appears from the use of neuroleptics, less often from antidepressants, sedatives, and atypical antipsychotics.
- Due to drug use. Akathisia is very often a syndrome that is present in drug addicts.
- Alcoholics. The negative effect of alcohol on the brain in long-term alcoholics leads to irreversible consequences in the subcortical ganglia, which provokes the occurrence of this syndrome.
- In patients with Parkinson's disease. Akathisia in such patients is not uncommon, but so far it has not been possible to establish whether this syndrome appears against the background of the underlying disease, or against the background of the drugs used for treatment, which act as a provoking factor.
Causes of akathisia
The reasons for the development of akatizive syndrome are divided into several types.
- Taking psychotropic drugs.
The most common side effect of chronic anxious restlessness occurs from taking antipsychotics: haloperidol, droperidol, pimozide. A similar effect is less common after atypical antipsychotics (olanzapine, aripiprazole) and antidepressants (mirtazapine). Sometimes sedatives (chlorpromazine) also lead to akathisia. The syndrome can also be caused by excessive use of sleeping pills, especially the barbiturates group.
- Drug use.
Mental changes towards the development of akathisia are characteristic of patients with opium and cocaine addiction. These drugs are strong poisons that depress nerve conduction in the brain. The list of substances that provoke akathisia also includes drugs from the amphetamine group, methylphenidate.
- Chronic alcoholism.
Long-term systematic consumption of alcohol has a detrimental effect on nerve endings and inhibits the functions of the subcortex of the brain. Neuromediation is disrupted, which negatively affects the functioning of the entire central nervous system.
- Parkinsonism, other mental disorders.
Both primary and secondary parkinsonism can cause akathisia. Science has not yet established exactly how great the role of concomitant medication is in treating the disease. The influence of two factors is likely to occur simultaneously. Chronic restlessness also occurs among patients with schizophrenia, anxiety and affective disorders.
Factors that increase the risk of chronic restlessness:
- genetic predisposition; in particular, science associates it with the gene of the first chromosome DRD2;
- various pathologies of the central nervous system;
- suffered traumatic brain injuries;
- dementia.
In addition, cases of akathisia are possible with abrupt withdrawal of psychoactive substances. An example would be someone waking up from anesthesia. Stopping treatment with antipsychotics and antidepressants can also cause a similar effect.
Characteristic symptoms
The picture of the disease consists of two characteristics: subjective (the patient’s internal sensations) and objective, or motor (excessive motor activity).
At the first stage, restlessness manifests itself in leg movements. A person cannot sit, stand, or lie quietly. He stomps, shuffles, jumps up, walks, shakes his leg, fidgets, tosses and turns from side to side.
Symptoms then spread to other parts of the body. This manifests itself in antics, jumping, darting glances, head shaking, constant meaningless, aimless movements.
The subjective component of the syndrome is expressed in anxiety, a painful feeling, often for no apparent reason. When complaining to a doctor, it is difficult for such a person to describe in words his internal sensations. They can be both sensory and psychological. The patient may feel a burning sensation, itching, aching inside the muscles and joints, but the diagnosis does not confirm any diseases of the musculoskeletal system. A person complains of psychological discomfort coming from within, a vague anxiety that forces him to move somewhere. The calmer the body position, the greater the feeling of anxiety.
In the later stages, the patient's character changes. He becomes irritable, suspicious, ingratiating. The pathology causes sleep disturbances in him. If akathisia is caused by an underlying mental disorder, then if left untreated it will only get worse.
Symptoms
A characteristic symptom is an internal feeling of restlessness and restlessness, which causes the need to move. The clinical picture of akathisia is accompanied by a sensory and motor component.
Sensory signs include unpleasant sensations of internal activity that cause the patient to move. At the same time, it is impossible to cope with motor excitation. Sensory symptoms can be general or somatic. The first group includes:
- alarm
- internal tension
- increased irritability
- causeless fear
- inability to relax
- sleep disturbance, worsening of the process of falling asleep, insomnia
The somatic clinic is difficult to convey in words, so problems often arise with diagnosing the condition. Somatic sensory symptoms include:
- heaviness and tingling in the legs
- feeling of twisting, twisting in the joints
- muscle aches
- burning, itching in muscles and joints
The motor component of akathisia is accompanied by pathological motor activity. For example, patients may cross their legs, shuffle, march in place, stroke their face, tap their fingers, or unbutton/fasten a button. Mild akathisia is characterized by erased symptoms, so it may be outwardly invisible to others. In this case, the patient is able to suppress external motor signs through willpower.
Classification of the disease, forms
Based on the prevalence of symptoms, akathisia is divided into the following forms:
- Motor akathisia. Patients experience movement disorders without anxiety. But at the same time they constantly move, mark time, walk, jerk their legs, etc. For example, a patient may stomp his foot in place without noticing, even when writing something.
- Mental form. Restlessness is almost reduced to zero, but subjective sensations are a source of discomfort. Most often it is constant anxiety, restlessness, and strong internal tension.
- Sensory. A person feels itching, muscle contraction, and other unpleasant sensations (usually in the lower extremities). He constantly scratches himself, rubs his knees, changes his position, etc.
Classic akathisia combines all of the above symptoms. The patient's complaints usually coincide with observation data of his behavior. The patient experiences a feeling of anxiety for no reason, which pushes him to move in an unknown direction and for what reason.
There is also a classification based on etiology, i.e. origin of the syndrome:
- Parkinsonian akathisia;
- Iatrogenic;
- Withdrawal symptoms;
- Caused by psychoactive substances;
- Post-stroke;
- Spontaneous (due to mental disorders).
The disorder varies in the timing of symptoms:
- Acute form. Develops in the first days, sometimes hours after the influence of a provoking factor. For example, a patient is taking antipsychotics, and the dosage of the drug has been increased. In such cases, reduce the dose or replace the drug with another. The syndrome gradually subsides after this.
- Chronic form. It is observed in a quarter of patients treated with antipsychotics. Occurs after taking the medicine for a month or more. It also gradually regresses after changing the drug.
- Late form. Symptoms of the disease appear months or years after the onset of exposure to the substance. In this form, discontinuation of the drug causes a deterioration in the condition. A person gets better only with an increase in dose, but not for long. Such akathisia may persist for the rest of life or gradually disappear after stopping taking the substance.
- Withdrawal syndrome. Familiar to any person who has quit drinking, smoking, using drugs, taking potent medications such as antipsychotics, sleeping pills, etc. It appears during the first two weeks after stopping taking the substance, but may persist longer (4-7 weeks). If withdrawal akathisia does not disappear after two months, a late form of the syndrome cannot be ruled out.
Correction and therapy of deviations
Therapy for this disease should be selected individually, taking into account the clinical picture and severity of the disease.
The most effective treatment method is complete withdrawal or significant reduction in the dosage of the drug that triggered the appearance of these symptoms. However, in practice this is not always possible, due to the mental state of the patient. Canceling medications can lead to a serious deterioration in his well-being.
The main component of therapy is the prescription of medications that can increase the effectiveness of antidepressants or antipsychotics without causing their side effects. Thanks to this, it is possible to significantly reduce the dosage of drugs that provoke akathisia.
There are a number of treatments for the disease. Antiparkinsonian drugs, such as Biperiden, Benztropine, etc., help to cope with the disorder. Such drugs are often prescribed as an addition to antipsychotics, which eliminates their side effects. The dosage should be selected by the attending physician.
Experts also prescribe the following groups of medications:
- Antihistamines and anticholinergic drugs . They are not included in the category of powerful medications, but they can be part of effective therapy. In this case, the use of Diphenhydramine and Atarax is indicated. An additional advantage of this treatment is the fact that such drugs have a slight sedative effect, which helps calm the person. The drugs reduce agitation and restore sleep.
- Tranquilizers . Such remedies significantly reduce the activity of the disease, eliminating feelings of anxiety, sleep disturbances and spontaneous arousal. Such medications are usually prescribed if the doctor is unable to conduct a detailed diagnosis.
- Beta blockers . A number of experts claim that drugs such as Metoprolol and Propranolol help reduce the effect of neuroleptics and eliminate anxiety.
- Anticonvulsants . Such products are highly effective. Recommended drugs include Pregabalin and Valproate. They help cope with feelings of anxiety.
- Weak opioids . Such drugs as Codeine and Hydrocodone are highly effective for this diagnosis.
In late forms of the disease, discontinuation of the main drug is indicated. It should be replaced with an atypical antipsychotic. Your doctor may prescribe Olanzapine or Clozapine.
With this diagnosis, the prognosis directly depends on the type of disease and the causes of its occurrence. For example, drug-induced akathisia can last from 1 month to six months. In this case, the withdrawal form of the disease lasts about 15-20 days.
Basic principles of diagnosis
Neurologists and psychiatrists are involved in the diagnosis and treatment of akathisia. Making a diagnosis is often difficult due to dementia, an unclear description of subjective sensations by the patient himself, and his lack of understanding of what is happening. In addition, at the very beginning of the pathology, patients can still control hyperkinesia through willpower: do not jump up, do not swing their legs, etc. Some patients have a negative attitude towards doctors and the treatment process. In practice, there are cases when such negativism is the only visible manifestation of akathisia.
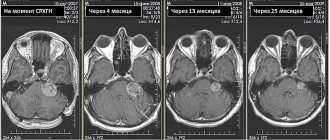
Diagnostics today uses many modern methods: MRI, CT, MSCT, EEG, REG of the brain. However, they allow us to exclude other diseases, nothing more. The doctor needs to interview the patient about the sensations he is experiencing and observe the patient’s behavior. Since the patient may hide symptoms and restrain movements, it may be necessary to interview relatives.
The patient's condition is assessed using a special Burns scale, which includes three points each to characterize the subjective and objective components. The degree of a person’s worries about the manifestations of his disease is separately assessed. Akathisia should be distinguished from other conditions and pathologies with increased motor activity (anxiety, psychomotor agitation, Tourette's syndrome, etc.).
Diagnostic principles
Akathisia is very difficult to diagnose. This pathology is very difficult to visualize using laboratory or instrumental methods.
To make an accurate diagnosis, the doctor must carefully examine the patient's symptoms and medical history. Some people have difficulty describing the clinical picture. In this case, the doctor can identify only one component of the disorder - for example, motor or sensory. As a result, the patient's condition will be assessed incorrectly.
To accurately determine the severity of a person’s condition, a special Burns scale was invented. In this case, the person is in a standing and sitting position for 2 minutes.
At the same time, the specialist assesses the presence of motor disorders and identifies the degree of emotional activity. Finally, the patient himself evaluates his condition. The final score can range from 1 to 5.
Treatment of akathisia
The therapeutic method is prevalent in the treatment of the disease. If acasative syndrome is caused by taking medications, you need to immediately change the dosage or replace the drug.
Patients are prescribed magnesium drugs, which, depending on the etiology and symptoms, are combined with medications from other groups. It can be:
- Beta blockers;
- Central anticholinergics;
- Antiadrenergics;
- GABAergic drugs;
- Dopaminergics;
- 5-HT-2 blockers.
With timely treatment, the prognosis is good. The course of treatment for withdrawal syndrome lasts about three weeks, for other forms – up to 8 months. The patient's relatives need to carefully monitor his condition.
Akathisia and insomnia
Symptoms of akathisia prevent the patient from sleeping peacefully. Patients experience constant difficulty falling asleep, roll over in bed, and have restless thoughts entering their minds. There are known cases of awakening from sleep in order to walk around the house or street. Constant lack of sleep at night leads to daytime sleepiness. After some time, “confusion between day and night” occurs, i.e. sleep time inversion.
If you take sleeping pills to combat insomnia, they do not always help and may even worsen the problems. The patient spends a lot of strength and energy on meaningless movement, without restoring strength through night sleep. Exhausted, some people see no way out and, in desperation, try to commit suicide.
Classification
It is customary to distinguish several classifications of akathisia. According to the etiological principle, the syndrome is usually divided into several different types:
- iatrogenic;
- parkinsonian;
- withdrawal symptoms;
- spontaneous;
- post-stroke.
According to the clinical manifestations of pathology, 3 types are distinguished:
- Motor – manifests itself mostly in movement disorders. Such patients feel the need for systematic movement, while there are no complaints about feelings of restlessness, anxiety, or discomfort in the body.
- Sensory-psychic. This type is characterized by complaints of deteriorating mental state, while there is no motor component. People complain of an overwhelming feeling of anxiety, fear, and panic.
- Classical. Patients with this type of disease have both complaints of anxiety and typical manifestations of motor hyperactivity. All these signs together allow specialists to make the correct diagnosis almost accurately and in the shortest time.
In any case, when choosing a treatment method, the key point is the provoking factor and the time of onset of the syndrome.
It is customary to distinguish 4 types of akathisia according to the time factor:
- Spicy. Occurs immediately after starting treatment with antipsychotics. As soon as the medication is stopped, the symptoms of the pathology gradually disappear;
- Chronic. The first signs appear a long time after the start of treatment. In 1/3 of cases, the syndrome occurs during treatment with antipsychotics. Once the patient stops taking the medications, symptoms disappear over time;
- Late. It makes itself felt no earlier than after 5-6 months. after starting medication. When treatment is discontinued, the patient begins to feel improvements, but in some cases patients may be bothered by certain manifestations of akathisia for the rest of their lives;
- Withdrawal akathisia. Appears in the first 14 days after stopping the medication and goes away within 30 to 45 days. If the symptoms of the pathology do not disappear after this time period, this indicates the presence of a late form.
Prevention
The best prevention of chronic restlessness syndrome is not to take psychotropics, sleeping pills and antidepressants. To do this, you need to lead a lifestyle so as not to bring your body to a state that requires taking them. Try to avoid stress if possible, learn to experience it adequately, perceive life philosophically, and look at it positively.
In cases where drug correction of pathologies is still necessary, it is important to use medications rationally, avoiding overdoses. Experts try to prescribe medications with the least extrapyramidal potential, starting with small doses.
Do not under any circumstances self-medicate for insomnia, depression, chronic fatigue syndrome, vegetative-vascular dystonia and other unpleasant syndromes. Wrong choice of drug without taking into account general medical history and drug interactions can lead to serious consequences. It sounds like a hackneyed truth, but it’s worth saying again about the benefits of a healthy lifestyle . First of all, you need to completely give up alcohol and drugs. A person who has nothing to give up will never experience akathisic drug withdrawal syndrome.
Relatives and friends of a person at risk need to provide him with all possible support. It is also extremely important to set this person up only for positive changes.