Home>Articles>Alcoholic encephalopathies: signs, forms, treatment
quick menu (hide)
- Symptoms of alcoholic encephalopathy
- Development of the disease
- Acute types of disease
- Chronic form of alcoholic encephalopathy
- Diagnosis and treatment
Chronic alcohol abuse leads to the development of various mental and physical problems over time. All organs in the body are affected by excessive use of a toxic substance, including brain function. Alcoholic encephalopathy manifests itself during the transition from stages II to III of alcoholism, but in some cases much earlier. The disease, whether acute or chronic, interferes with a person's ability to think rationally and retain memories. If left untreated, it can lead to permanent brain damage.
Symptoms of alcoholic encephalopathy
Alcoholics are at risk of encephalopathy, which causes brain dysfunction. Symptoms of the disease are accompanied by psychosomatic and neurological changes:
- Weight loss, lack of appetite;
- Loss of muscle coordination;
- Involuntary movements or paralysis of the eyes;
- Anxious state with changeable mood;
- Short-term memory loss;
- Fatigue;
- Delirium, hallucinations.
The illness is characterized by profound confusion, indifference, inattention, drowsiness, or stupor. Side effects of the peripheral nervous system increase, and many develop severe autonomic dysfunction, characterized by sympathetic hyperactivity - tremor, agitation, or hypoactivity - hypothermia, postural hypotension, syncope. The torpor may progress to coma and end in death.
Development of alcoholic encephalopathy
Encephalopathy leads to rapid damage to brain cells due to regular use of the toxin. Even in genetically healthy people with normal nutrition, constant poisoning of the body for more than 7 years is characterized by stage II or III of alcoholism. Symptoms also appear with periodic consumption of alcohol in large quantities - binge drinking. The pathology has a chronic or acute form.
The severe illness covers a wide range of alcohol-related intellectual and neurological syndromes, including Wernicke encephalopathy, Korsakoff's syndrome and other disorders affecting brain structures. The duration of the period from the first symptoms to a chronic disease is individual and depends on lifestyle. In some cases, clinical changes occur suddenly.
This pathology accounts for up to 70% of the death statistics - this figure is called by narcologists. Encephalopathy can be complicated by pseudoparalytic or psychoorganic syndrome, and can also lead to dementia. The prognosis for cure depends on timely diagnosis. Qualified timely treatment can correct all abnormalities.
Treatment of alcoholic encephalopathy requires hospital care and takes a fairly long period. Without medical attention, the disease becomes serious. Professionals monitor symptoms so the progression of the disorder is slowed or stopped.
Content:
- Features of alcoholic epilepsy.
- Risk factors for epileptiform syndrome in alcoholism.
- Precursors of an epilepsy attack.
- Symptoms.
- Consequences of epileptic episodes in alcoholics.
- Treatment.
Alcoholic epilepsy is a pathological condition caused by drinking alcoholic beverages. It can be observed both in chronic alcoholics and in people who drank alcohol for the first time. It is characterized by the presence of epileptic seizures, which are most often accompanied by convulsions. There are also automatic actions, and loss of consciousness is possible. Treatment is carried out by doctors of the following specializations: neurologists, narcologists, psychiatrists.
Causes of development of alcoholic encephalopathies
Experts call the cause of the pathology long-term alcohol poisoning of the body - regular uncontrolled or daily consumption of drinks, binge drinking for a week or more. Additional risks arise from low-quality, homemade or technical drinks. The individual characteristics of the body cause the development of the disease with small doses of alcohol and rare intakes.
The main cause of encephalopathy is a deficiency of B vitamins, which ensure normal brain functioning. Alcohol changes metabolism and requires increased levels of thiamine. During long-term drinking bouts, vitamin reserves are reduced due to lack of appetite, poor-quality or insufficient food. Then problems appear with the processing of thiamine in the intestines against the background of changes in liver function, as well as a decrease in the levels of vitamins B6 and P. Progressive deficiency causes disturbances in the metabolic processes of digestion, vascular permeability, which mainly ends in cerebral edema.
The disease is personal in its rate of development, dominant symptoms, development options and final outcome. The diagnosis involves two main groups of alcoholic encephalopathies - acute or chronic.
Acute pathologies include:
- acute mitigated encephalopathy;
- Gaye-Wernicke syndrome or hemorrhagic polyencephalitis;
- encephalopathy with immediate course.
In the anamnesis of chronic patients, severe psychoses and acute encephalopathies are observed against the background of alcohol dependence. The chronic form is diagnosed as Korsak's psychosis in the form of alcoholic paralysis, polyneuritic psychosis and alcoholic pseudoparalysis.
Features of alcoholic epilepsy
Epilepsy is a pathology of the brain in which paroxysms of motor and mental disorders occur and recur over time. Seizures and other symptoms of epilepsy are caused by an excessive number of nerve impulses in the cerebral cortex.
To make a correct diagnosis, the frequency of epileptic seizures plays a role, since convulsive syndrome occurs in many diseases (for example, cerebrovascular accident, encephalitis).
Alcoholic epilepsy is different in that it occurs at stages 2-3 of the development of chronic alcoholism and manifests itself most often during the period of abstinence (during the “withdrawal syndrome,” also called a hangover).
Alcoholic encephalopathy of the brain - what is it?
The harbingers of the disease are violations of the body’s simple needs - reluctance to eat. Lack of nutrition leads to asthenia and sleep disorders. Patients are characterized by an aversion to fatty and protein foods, and a craving for carbohydrate foods appears. Continuous nausea and vomiting accompany the patient in the morning. A nutritional imbalance results in a disruption of metabolic processes, resulting in urinary tract infections and severe anorexia.
Toxic alcoholic encephalopathy is accompanied by a large number of metabolic disorders, as well as:
- liver and kidney failure;
- dehydration;
- electrolyte imbalance;
- fever;
- arterial hypertension;
- hypoxemia;
- infections, including sepsis.
Classic Gaye-Wernicke encephalopathy mainly manifests itself in moderate delirium. Patients develop obsessive visual fragmentary hallucinations and illusions, which are accompanied by repetitive movements. Excitement at intervals gives way to stupor, but muscle tone remains high. During attacks, patients scream, mutter, communication is excluded.
Acute alcoholic encephalopathies
Acute encephalopathy is characterized by a global functional change in the mental state due to systemic factors of the body, but is reversible with a return to the basic mental status with timely referral to specialists. The disorder is characterized by classic clinical
triad of ocular motor dysfunction, ataxia (cerebellar dysfunction) and mental disorders. Symptoms of Wernicke encephalopathy include:
- Difficulty speaking.
- Amnesia.
- Incoherent speech.
- Double vision.
- Hypotension.
- Difficulty swallowing.
- Intense eye movement.
- Attention deficit.
- Ataxia.
- Disorientation.
- Cold skin.
- Psychic identification.
The disease causes external changes - swelling of the face against a background of general exhaustion.
Various neurological disorders are detected - different pupil sizes, nystagmus, unexpressed paresis. At the same time, the temperature rises, the pulse and, accordingly, breathing becomes uneven, the pressure drops. Upon examination, an enlarged liver is detected, the tongue has a crimson tint. The more complex the clinical symptoms, the more complications accompany the patient, including stupor and suffocation. Often the acute course of the disease leads to coma.
According to statistics, death occurs 10-14 days after the onset of delirium, especially when accompanied by bedsores or pneumonia. If the disease is under the control of doctors, treatment lasts from 3 to 6 weeks and ends with psychoorganic syndrome. The patient partially loses memory and has difficulty adapting to the environment.
- Mitigated acute encephalopathy begins with asthenia, loss of appetite, worsening mood, and sleep disorders.
- The hyperacute form is characterized by immediate development and frequent death. Precursors appear from about 3 weeks.
Consequences of epileptic episodes in alcoholics
The very “convulsive readiness” in persons suffering from chronic alcoholism indicates deep-seated brain damage. Excessive consumption of ethanol leads to encephalopathy , which manifests itself as follows.
Sudden cardiac arrest due to arrhythmia, falling into a coma, and unexpected death are possible.
Pneumonia also occurs ; it is often accompanied by pulmonary edema, which is also life-threatening.
In some cases, an alcohol addict suffers severe injuries that lead to disability.
An unconscious state is fraught with retraction of the tongue and suffocation; the patient can also choke on his own vomit at this time.
In those suffering from alcoholic epilepsy, personality degradation occurs at an accelerated pace, aggressiveness increases, which can negatively affect others. Such patients often have suicidal thoughts, and with a psychotic disorder they may commit suicide.
Death can also occur from swelling of the brain stem tissue when it is wedged into the foramen magnum.
Since the conditions described pose a direct threat to the life of the addict, in no case should you leave him without qualified medical care , much less try to relieve the attack on your own, at home.
Alcoholic encephalopathies in chronic form
Signs of this form are: memory impairment, false memories, disorientation. Women suffer more often from Korsakov's psychosis, men less often. The forms of manifestation are: the inability to remember new information, difficulty remembering what happened before the illness, and arranging events in chronological order. Sometimes the patient can “remember” something that never happened to him - he is completely convinced that it really happened. It is also difficult for the patient to navigate in time, to say where he is and what time it is, how long he has been in a certain place. Neuritis is also characteristic.
If you completely eliminate alcohol consumption, symptoms may disappear and weaken.
For men, pseudoparalysis is more typical. It can develop at different rates, progress, and sometimes develop into psychosis and dementia. Characteristic signs may be: memory impairment, inability to perform normal functions, roughness, mood swings, neurological symptoms that can be seen clearly - tremor, trembling of the face, hands.
Signs
A prerequisite for the development of any alcoholic encephalopathy is chronic alcoholism in a person. As a rule, the disease develops at the end of the second and third stages of alcoholism. In women with constant abuse of ethanol, encephalopathy can be diagnosed 3-4 years after the start of drinking alcohol. The life expectancy of patients with alcoholic encephalopathy averages from 6 to 20 years.
Prodromal period
The prodromal period is characteristic of acute and chronic encephalopathies and can last from several weeks to several months. During this period, a person exhibits nonspecific symptoms: malaise, loss of appetite, general weakness, decreased mood, and others. Asthenic phenomena predominate and can lead to aversion to food and a sharp decrease in physical activity. A person is worried about heartburn, nausea, stool disorders, and changes in blood pressure. Changes in sleep occur in almost all patients. Drowsiness appears during the daytime and insomnia at night, nightmares occur, sleep becomes intermittent and superficial.
A person complains of palpitations, body aches, chills, which are replaced by a feeling of heat. There is trembling in the hands, headaches, dizziness. During the prodromal period, a person continues to abuse alcoholic beverages, which aggravates the general condition.
Acute encephalopathies
People who drink alcohol for a long time develop vitamin B deficiency, which leads to the development of encephalopathy.
According to the severity and duration of the disease, acute encephalopathies are divided into three types:
- Acute alcoholic Wernicke's encephalopathy.
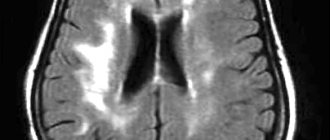
The cause of the development of Wernicke's encephalopathy is a deficiency of thiamine (vitamin B1), which is formed in people with prolonged alcohol consumption, fasting, or disruption of food absorption in the digestive tract due to other diseases. The exact mechanism of damage to the structures of the central nervous system due to vitamin B5 deficiency is not known, but it has been established that the gray matter of the brain, mamillary bodies, thalamus and cerebellum are primarily affected. Degenerative processes occur in nerve cells (neurons), microhemorrhages.
CM. SEE ALSO: Diabetic encephalopathy: features of the course and treatment
The clinical picture is dominated by a triad of symptoms:
- Ophthalmoplegia is a complete absence of voluntary movements of the extraocular muscles, which are responsible for the movements of the eyeballs. In the clinic, this is manifested by the development of strabismus or immobility of the eyes. Strabismus can be unilateral or bilateral, convergent or divergent. Horizontal or vertical large-scale nystagmus is often detected. Nystagmus is oscillatory movements of the eyeballs with a certain amplitude.
- Ataxia is a violation of motor coordination that occurs when the cerebellum and vestibular nerve nuclei are damaged. The person's gait is disturbed. It becomes unsteady, leads to falls and is accompanied by dizziness.
- Impaired consciousness. A person's concentration of attention decreases, memory deteriorates, inhibition of thinking and difficulty in learning new information appear. In severe cases, confusion and stupor occur, which may give way to coma.
They identify mental disorders that manifest themselves as visual, tactile, and verbal hallucinations. A person sees a snake instead of a crack on the wall or hears someone else's speech, tries to turn on an imaginary tap, talks to himself. In severe cases, hallucinations cease to be combined with the environment, the person is in a fictional space, but orientation remains in his own personality. As the disease progresses, drowsiness and apathy appear during the daytime, and hallucinations resume at night.
In severe cases, the hypothalamus is affected, which leads to a drop in blood pressure and the development of coma. Death occurs in the absence of treatment as a result of disruption of the regulation of the body's autonomic reactions by the hypothalamus (blood pressure, heart rate, vascular tone, etc.).
An early sign of recovery is normalization of sleep.
- Acute mitigated alcoholic encephalopathy.
The disease begins with a prodromal period, which is characterized by the appearance of nonspecific symptoms. Fatigue, loss of appetite, general weakness, and sleep disturbance appear. A person’s mood decreases, emotional depression appears, preoccupation with his condition and a search for non-existent diseases in himself. On the part of the peripheral nervous system, neuritis is diagnosed - damage to the nerve fibers that innervate a certain area. Neuritis is accompanied by pain, tingling or numbness. The prodromal period lasts on average 1-2 months and is replaced by the appearance of delirium. Delirium is auditory and visual hallucinations that are accompanied by delirium. The patient speaks out, talks to imaginary subjects, and does not come into contact with others. After the mitigated encephalopathy subsides, residual effects are revealed in the form of memory disorders that are difficult to treat. Neurological disorders associated with the development of delirium are insignificant.
- Fulminant encephalopathy (hyperacute form).
It is characterized by a rapid onset and a high incidence of deaths on days 2-5 from the onset of the disease. The prodromal period lasts about 2-3 weeks and is replaced by the development of psychosis, which is represented by occupational delirium (the patient believes that he is at work).
A person’s body temperature rises to 40-41 C, which is difficult to bring down with antipyretic drugs. Consciousness is impaired to the point of coma.
Chronic encephalopathies
The clinical picture of Korsakov's psychosis is dominated by memory impairment
- Korsakov psychosis.
It is believed that the basis of the disease is damage to the nuclei of the thalamus against the background of long-term alcoholism. More often it develops after alcoholic psychosis, which was accompanied by severe hallucinations. The clinical picture is dominated by memory disorders in the form of loss of life episodes of varying duration that preceded the disease (retrograde amnesia) and the inability to remember new information (fixation amnesia). Such patients cannot remember the room number, the address of the hospital, what they ate for breakfast and other points, but they remember long-ago events well. Memory impairment does not upset patients and they are not concerned about their condition. Another symptom of Korsakoff psychosis is false memories. They arise in response to questions that are asked to a sick person, and he replaces “memory lapses” with fictitious events. Patients may be disoriented in place, time and people around them. Easily fatigued and lack of interest in the world around us is revealed.
- Alcoholic pseudoparalysis.
CM. SEE ALSO: Diabetic encephalopathy: features of the course and treatment
The disease manifests itself with psychopathological and neurological symptoms.
Psychopathological symptoms are represented by the patient’s ideas of his own greatness, lack of criticism of his behavior and the behavior of those around him, and euphoria. From the nervous system, tremors are detected in the hands, tongue and facial muscles. Speech becomes slurred, memory is impaired, and convulsive seizures may occur. Alcoholic pseudoparalysis during treatment can completely stop or, conversely, progress. This depends on the patient’s concomitant and previous diseases.
How to diagnose and treat alcoholic encephalopathy?
Diagnosis of the disease is not difficult - it is done on the basis of symptoms and anamnesis. Differential diagnosis is also carried out with other manifestations of psychosis - for example, with brain tumors, schizophrenia and other lesions and diseases.
To cure a patient, you need:
- A complex of proper, balanced nutrition with the optimal amount of vitamins and proteins;
- Nootropics are prescribed, drugs that have a beneficial effect on metabolism and blood circulation in the brain;
- Prescribe treatment for somatic disorders;
- Protection against the transition of acute to chronic form, treatment of alcoholism using various methods - medication, coding and others;
- Therapy with a psychologist, work in a group to help the patient live a normal life without alcohol.
The most important factors for success in treatment are: an individual and comprehensive approach, complete cessation of alcohol consumption.
Treatment
The sooner treatment for encephalopathy is started, the greater the chance of stopping the progression of the pathology and restoring full brain function.
First of all, it is necessary to eliminate the cause of neuronal damage:
- adjust blood sugar levels;
- stabilize blood pressure;
- restore the functioning of the liver, kidneys, pancreas;
- reduce blood cholesterol levels;
- remove toxins;
- normalize hormone levels, etc.
Direct treatment of encephalopathy requires the prescription of drugs that improve blood flow in the vessels of the brain and metabolism within the cell. Depending on the cause and extent of the lesion, doctors may prescribe:
- nootropics (Cerebrolysin, piracetam): aimed at enhancing metabolism;
- blood thinners (aspirin, pentoxifylline, etc.): help accelerate blood flow, prevent the formation of blood clots;
- antioxidants: neutralize toxins;
- angioprotectors (Cavinton, nicotinic acid and others): necessary to accelerate blood circulation and metabolism;
- vitamin-mineral complexes, amino acids;
- symptomatic drugs: sedatives, anticonvulsants, etc.
For encephalopathy, courses of treatment are carried out regularly, at least 2 times a year. This allows you to keep the disease under control. The selection of specific drugs and determination of dosage is carried out only by a doctor. There is no single treatment regimen for all patients.
To enhance the effect of drugs, non-drug treatment methods are used:
- physiotherapy (reflexotherapy, electrophoresis, magnetic therapy, laser therapy);
- physical therapy to improve muscle condition and facilitate control over them;
- massage to relax and improve blood circulation;
- acupuncture.
In some cases (with the vascular nature of encephalopathy), it is necessary to resort to surgical treatment:
- elimination of a blood clot from the lumen of blood vessels;
- expansion of narrowed sections of the artery with the installation of a stent that supports the walls in the correct position;
- bypass: restoration of blood flow by creating an alternative path that bypasses the affected area.