The cause of PA is the release of adrenaline into the blood
It is because of the strong release that a state of adrenaline overdose occurs and a vegetative crisis appears. Therefore, treatment of panic attacks in the initial stages is aimed at reducing and regulating the amount of adrenaline in the blood. Then symptomatic treatment is carried out and work with fear of a recurrence of panic.
How adrenaline affect the human body? This is a substance that is secreted by the adrenal glands and provokes a stressful state in humans. When released into the blood, adrenaline is quickly destroyed, entering into various biochemical reactions. Therefore, as soon as the adrenal glands stop producing adrenaline, the state of stress goes away. However, a person himself can cause relapses of this condition, being under the influence of an experienced event.
ANAPRILIN
special instructions
Monitoring of patients taking propranolol should include monitoring heart rate and blood pressure (daily at the beginning of treatment, then once every 3-4 months), electrocardiogram, plasma glucose concentration in patients with diabetes mellitus (once every 4 months). -5 months).
In elderly patients, it is recommended to monitor kidney function (once every 4-5 months). The patient should be taught how to count the number of heartbeats and instructed about the need for medical consultation if the number of heartbeats is less than 50 beats/min. Before using propranolol, patients with chronic heart failure (early stages) must use cardiac glycosides and/or diuretics.
In smokers, the effectiveness of beta-blockers is lower.
Patients using contact lenses should take into account that during treatment there may be a decrease in the production of tear fluid.
Patients with pheochromocytoma are prescribed only in combination with alpha-blockers.
In thyrotoxicosis, propranolol may mask certain clinical signs of thyrotoxicosis (eg, tachycardia). Abrupt withdrawal in patients with thyrotoxicosis is contraindicated as it can increase symptoms.
When prescribing beta-blockers to patients receiving hypoglycemic drugs, caution should be exercised, since hypoglycemia may develop during prolonged breaks in food intake. Moreover, its symptoms such as tachycardia or tremor will be masked due to the action of the drug. Patients should be instructed that the main symptom of hypoglycemia during beta-blocker treatment is increased sweating.
When taking clonidine concomitantly, it can be discontinued only a few days after propranolol is discontinued.
It is possible that the severity of the hypersensitivity reaction may increase and the absence of effect from usual doses of epinephrine against the background of a burdened allergic history.
A few days before general anesthesia, you must stop taking the drug. If the patient took the drug before surgery, he should choose a drug for general anesthesia with minimal negative inotropic effect.
Reciprocal activation of the vagus nerve can be eliminated by intravenous atropine (1-2 mg).
Medicines that reduce the supply of catecholamines (for example, reserpine) may enhance the effect of beta-blockers, so patients taking such combinations of drugs should be under constant medical supervision to detect arterial hypotension or bradycardia.
Do not use simultaneously with antipsychotic drugs (neuroleptics) and anxiolytic drugs (tranquilizers).
Use with caution in combination with psychoactive drugs, for example, monoamine oxidase inhibitors, when used for a course of more than 2 weeks.
Avoid intravenous administration of verapamil and diltiazem during therapy with Anaprilin.
In case of increasing bradycardia (less than 50 beats/min), arterial hypotension (systolic blood pressure below 100 mm Hg), atrioventricular block, bronchospasm, ventricular arrhythmias, severe liver and kidney dysfunction in elderly patients, it is necessary to reduce the dose or stop treatment. It is recommended to discontinue therapy if depression caused by taking beta-blockers develops.
Treatment should not be abruptly interrupted due to the risk of developing severe arrhythmias and myocardial infarction. Cancellation is carried out gradually, reducing the dose over 2 weeks or more (by 25% in 3-4 days).
The drug should be discontinued before testing catecholamines, normetanephrine and vanillylmandelic acid in blood plasma and urine; antinuclear antibody titers.
Symptoms
The symptoms of a panic attack can vary from person to person. This is due to the fact that symptoms are the results of the human body’s struggle with unexpected chemical processes, and exactly how this struggle will manifest itself depends on the individual characteristics of the person. During a panic attack, you may experience difficulty breathing (a feeling that your throat is swelling), rapid heartbeat, and pulsating blood in your temples. A person may feel sick, feel either hot or cold, or feel uncontrollable trembling. But in the end, the most difficult feeling is a feeling of sudden and overwhelming fear or panic.
Anaprilin 10 mg Renewal No. 112
Hypersensitivity to the drug, atrioventricular block II-III degree, sinoauricular block, sinus bradycardia, arterial hypotension, uncontrolled chronic heart failure IIB-III degree, acute heart failure, acute myocardial infarction (systolic blood pressure less than 100 mm Hg) , cardiogenic shock, pulmonary edema, sick sinus syndrome, Prinzmetal's angina, cardiomegaly (without signs of heart failure), vasomotor rhinitis, occlusive peripheral vascular disease, diabetes mellitus, metabolic acidosis.
Side effect
From the cardiovascular system: sinus bradycardia, atrioventricular block, heart failure, palpitations, myocardial conduction disturbances, arrhythmias, decreased blood pressure, orthostatic hypotension, chest pain, spasm of peripheral arteries, cold extremities, mesenteric thrombosis.
From the digestive system: dryness of the oral mucosa, nausea, vomiting, diarrhea, constipation, pain in the epigastric region, impaired liver function, changes in taste, ischemic colitis.
From the nervous system: headache, insomnia, nightmares, asthenic syndrome, agitation, depression, paresthesia, increased fatigue, weakness, dizziness, drowsiness, confusion or short-term memory loss, hallucinations, tremor, catatonia, emotional lability, decreased speed of psychomotor reactions.
Carefully
Hepatic and/or renal failure, hyperthyroidism, myasthenia gravis, heart failure, pheochromocytoma, psoriasis, pregnancy, history of allergic reactions, Raynaud's syndrome, old age.
*for more details, see the instructions for medical use of the drug LS-002037
Overdose
Symptoms:
bradycardia, dizziness or fainting, decreased blood pressure, arrhythmias, difficulty breathing, cyanosis of fingernails or palms, or convulsions. Treatment: gastric lavage, administration of activated charcoal, if atrioventricular conduction is impaired, 1-2 mg of atropine, epinephrine are administered intravenously, if efficiency is low, a temporary pacemaker is installed; for ventricular extrasystole - lidocaine (class IA drugs are not used).
Interaction with other drugs
The hypotensive effect of propranolol is enhanced when combined with diuretics, reserpine, hydralazine and other antihypertensive drugs, as well as ethanol.
The hypotensive effect is weakened by non-steroidal anti-inflammatory drugs (sodium retention and blocking renal prostaglandin synthesis), estrogens (sodium retention) and monoamine oxidase inhibitors. Cimetidine increases bioavailability.
Treatment
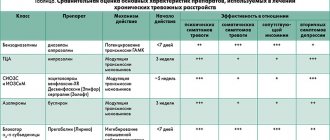
Treatment of panic attacks is currently very successful and effective. When treating phobias and panic attacks, treatment is initially aimed at the root cause of the state of panic - the release of adrenaline, and therefore adrenergic blockers are used. However, before therapy it is necessary to exclude diseases with similar symptoms, among which sympathoadrenal crisis can be distinguished. In one case, a vegetative crisis may occur due to an adrenal adenoma - this is a benign tumor, due to which excess adrenaline can be released into the blood. In another case, a symptomatic adrenal crisis may occur against the background of neurosis, and disturbances of the autonomic nervous system may also be observed. The crisis is triggered by an incorrect command from the human brain addressed to the adrenal glands, as a result of which they mistakenly release adrenaline. However, a modern psychiatric clinic has a sufficient range of equipment, and thanks to the work of highly qualified specialists, it will not be difficult to confirm or refute this diagnosis. Psychotherapy plays an important role in the treatment of panic attacks, since drug treatment alone cannot eliminate the underlying cause of the disease. Drug therapy will help temporarily eliminate or mitigate the symptoms of the disease, but intensive psychotherapy can find and eradicate the true causes of panic attacks.
Instructions for use ANAPRILIN-ZDOROVYE
In patients with diabetes mellitus, caution should be exercised when prescribing propranolol and hypoglycemic agents simultaneously, as propranolol may prolong the hypoglycemic response to insulin and change heart rate.
Class I antiarrhythmic drugs and amiodarone may potentiate the effect of propranolol on atrial conduction time and cause a negative inotropic effect. Propranolol is used with extreme caution in patients receiving concomitant treatment with cardiodepressants (chloroform, ether or related anesthetics), antiarrhythmic drugs (quinidine, lidocaine, procainamide), which may potentiate the depressive effects of propranolol.
Digitalis glycosides, when used concomitantly with beta-blockers, may increase atrioventricular conduction time.
Antihypertensive drugs potentiate the antihypertensive effect of propranolol.
The simultaneous use of propranolol with calcium channel blockers with negative inotropic action (veralamil, diltiazem) may lead to increased negative inotropic action in patients with impaired cardiac function and/or impairment of sinoatrial or atrioventricular conduction, leading to the development of severe hypotension. bradycardia and heart failure. A β-blocker or calcium channel blocker should not be administered intravenously within 48 hours after stopping the other. Concomitant use of dihydropyridine calcium channel blockers (eg, nifedipine) may increase the risk of hypotension and cause heart failure in patients with latent hypotension. The hypotensive effect of propranolol is enhanced when combined with diuretics (hydrochlorothiazide).
Concomitant use of epinephrine, isoproterenol and dobutamine may reduce or block the effects of propranolol. Caution should be exercised when administering drugs containing epinephrine parenterally to patients using propranolol. as this may lead to vasoconstriction, hypertension and bradycardia. Caution should also be exercised when used with drugs such as isoprenaline and norepinephrine.
Propranolol may exacerbate the "withdrawal" hypertension caused by clonidine withdrawal. If these two drugs are used concomitantly, the β-blocker should be discontinued several days before stopping clonidine. When replacing clonidine with a β-blocker, use of the latter should begin several days after stopping clonidine. Reserpine, when used simultaneously with propranolol, can reduce the activity of the sympathetic nervous system, which leads to hypotension, bradycardia, dizziness, fainting, and orthostatic hypotension.
The use of propranolol during a lidocaine infusion may increase lidocaine plasma concentrations by approximately 30%. Patients who have already used propranolol have a greater tendency to have higher lidocaine blood concentrations than those who have not used propranolol.
When using propranolol concomitantly with ergotamine, dihydroergotamine or related drugs, caution should be exercised due to the possibility of vasospastic reactions.
When used concomitantly, prostaglandin synthesis inhibitors (eg, ibuprofen and indomethacin) may reduce the hypotensive effect of propranolol.
The administration of propranolol, like other beta-blockers, together with an anesthetic may result in attenuation of reflex tachycardia and increase the risk of hypotension. The anesthesiologist should be informed about the patient's use of propranolol and the drug with the least negative inotropic effect should be selected as an anesthetic agent.
Propranolol, tricyclic antidepressants and MAO inhibitors mutually potentiate each other's hypotensive effects. With the simultaneous use of propranolol with haloperidol, the development of hypotension and heart failure is possible, with chlorpromazine - an increase in the concentrations of both drugs in the blood plasma, resulting in an increase in the antipsychotic effect of chlorpromazine and the antihypertensive effect of propranolol. Propranolol increases blood concentrations of imipramine.
The simultaneous administration of propranolol with drugs that are metabolized with the participation of cytochrome P450 isoenzymes CYPD6, CYP2C19, CYP1A2 may lead to changes in the effectiveness and tolerability of propranolol. The metabolism of propranolol in the liver increases with a decrease in its level in the blood when used simultaneously with inducers of these enzymes - barbiturates, rifampicin, phenytoin, ethanol; decreases with increasing levels of propranolol in the blood when used simultaneously with enzyme inhibitors - amiodarone, cimetidine, serotonin reuptake inhibitors (fluoxetine, naroxetine, fluvoxamine), quinidine, ritonavir, imipramine. ciprofloxacin, isoniazid, theophylline, zolmitriptan. No interaction of propranolol with ranitidine and lansoprazole has been established.
Allergens used for immunotherapy or allergen extracts for skin testing, when used concomitantly with propranolol, increase the risk of severe systemic allergic reactions or anaphylaxis. Iodine-containing radiocontrast agents, when administered intravenously during propranolol therapy, increase the risk of developing anaphylactic reactions.
Panic attacks and willpower
There are a number of common points in the treatment of panic attacks and neuroses - their therapy involves searching for the internal cause of the attacks. Usually these reasons are psychological trauma and severe stress. However, if a person with a strong will was able to suppress them and displace the strongest experiences into the subconscious, then deeply hidden emotions will make themselves felt. Since a person has not allowed himself to fully experience a strong emotion - joy, grief, excitement, etc., this feeling will find a way out for the realization of nervous excitement. As a result, a panic attack may develop. But having found out the true cause of the disease, the psychotherapist can, using the patient’s volitional qualities, eliminate the source of the panic state. Therefore, treating panic attacks through psychotherapy is quite successful and effective, as it combats the underlying cause of the disease.
Outpatient and inpatient treatment
The Mental Health Clinic successfully combines the treatment of panic attacks both with medication and through psychotherapy. Most often, treatment for panic attacks is carried out on an outpatient basis, but there are also options for inpatient placement. The attending physician will select an antidepressant that will help relieve acute symptoms and draw up a treatment plan, including the prevention and relief of possible recurrences of panic attacks. Patients who clearly know how to help themselves when the disease manifests itself experience significantly less fear of the manifestation of a crisis, which reduces general anxiety and raises the emotional background in general. However, the most important psychiatric help for panic attacks is to conduct active psychotherapeutic work with the patient. This will allow you to find the root cause of the disease and, by completely eliminating it, get rid of the disease forever.
We can help you! Call us