Astrocytoma is one of the most common brain tumors. The inside of the tumor often contains cysts, which can grow to large sizes and cause compression of the brain matter.
Benign astrocytomas, located in an accessible location, give a better prognosis for life expectancy than high-grade astrocytomas or benign astrocytomas, located in a location inaccessible to the surgeon and having a large tumor size. The earlier a tumor is detected, the better the prognosis for its treatment.
At the Yusupov Hospital they deal with the diagnosis and treatment of astrocytes. The hospital is equipped with innovative diagnostic equipment that allows you to receive all diagnostic services.
Brain astrocytoma: what is it?
An astrocytoma is a glial brain tumor that develops from astrocytes, neuroglial cells that look like stars or spiders. Astrocytes support the structural component of the nervous system of the brain - neurons. Astrocytes influence the movement of substances from the wall of a blood vessel to the plasma membrane of a neuron, participate in the growth of nerve cells, regulate the composition of intercellular fluid, and much more. Astrocytes in the white matter of the brain are called fibrous or fibrous. Protoplasmic astrocytes predominate in the gray matter of the brain. Astrocytes perform the function of protecting brain neurons from chemicals and injuries, providing nutrition to neurons, and participating in regulating brain blood flow.
Brain tumors cannot be called cancer, since cancer does not develop from epithelial cells, but from cells of more complex structures. A malignant brain tumor practically does not metastasize beyond the brain, but the brain can be affected by metastases from tumors located in other organs and tissues of the body. A malignant brain tumor may be no different from a benign tumor. A brain tumor does not have a clear boundary, so its complete removal is almost impossible. The difficulty of treating such tumors is that the brain has a blood-brain barrier, through which many antitumor drugs do not pass; the brain has its own immunity. A brain tumor can affect the entire brain - the tumor itself can develop in one part of the brain, and its cells can be located in different places in the brain.
Polyclonal brain tumors are a tumor within a tumor. These include primary brain tumors. The difficulty is that such a combination of tumors should be treated with different groups of drugs - one of the tumors is insensitive to drugs for treating another type of tumor. A major role in the effectiveness of treatment of a brain tumor is played not by the determination of the histological type of the tumor, but by the location and size of the tumor.
Causes
There is currently no data on the reasons for the development of tumors from astrocyte cells. There is an opinion that some negative factors can serve as a trigger for tumor development:
- radioactive exposure. Radiation often causes the development of malignant brain tumors in patients. The risk of developing astrocytoma increases in patients who have undergone radiotherapy;
- long-term exposure to toxic chemicals. Working in hazardous work can cause the development of brain tumors.
- oncogenic viruses;
- hereditary predisposition;
- injuries;
- patient's age. Some types of tumors primarily affect children, others are more common in young people between 20 and 30 years of age, and a third type of tumor affects older people more.
When studying the causes of astrocytomas, two types of damaged genes were identified.
You might also be interested
Pleomorphic xanthoastrocytoma
Tumors of neuroepithelial tissue / Pleomorphic xanthoastrocytoma ICD/O / 9424/3 (G II). Pleomorphic xanthoastrocytoma is often a cystic, less often a solid tumor with a favorite localization in the temporal lobe, and occurs at a young age.
Diffuse astrocytoma
Diffuse astrocytoma is an infiltrative tumor without clear boundaries. With the relative clarity of the border of the macroscopic picture, the distribution of its cells is wider. Steadily progresses to an anaplastic form, affecting any parts of the central nervous system, less often the brain stem and occipital lobes.
Subependymal giant cell astrocytoma
Subependymal solid tumor at the foramen of Monroy, may contain calcifications, occurs in 15% of patients with tuberous sclerosis.
Ependymoma
Ependymoma is more common in children and is located mainly in the IV ventricle, and in adults it is often supratentorial, representing a cystic-solid or entirely solid node, which may contain petrification and be surrounded by perifocal edema.
Glioblastoma
Glioblastoma is a high-grade tumor of heterogeneous structure with central necrosis, rapid infiltrative growth, perifocal edema and the worst prognosis among all gliomas.
Brain stem tumors
Brainstem glioma is not a separate histological form, but only reflects the anatomical localization of a neoplastic lesion, which may include: diffuse and circumscribed astrocytomas, embryonal tumors, ependymoma and glioblastoma.
Medulloblastoma
Medulloblastoma is more common in children and is located infratentorially, representing a cystic-solid tumor, arising from the cerebellar vermis, with a tendency to grow into the lumen of the fourth ventricle.
Schwannoma (neurinoma)
Acoustic schwannoma (neurinoma, neurolemmoma) is a space-occupying formation of the cerebellopontine angle, growing into the auditory canal, expanding it into the cranial cavity, affecting mainly adults; Bilateral schwannomas are associated with neurofibromatosis type II.
Symptoms of astrocytoma development
Symptoms of tumor development depend on its location and size. Depending on its location, it can impair coordination of movement (tumor in the cerebellum) and cause disturbances in speech, vision, and memory. Tumor growth in the left hemisphere can cause paralysis on the right side of the body. A patient with a brain tumor suffers from a headache, sensitivity is impaired, weakness appears, blood pressure surges, and tachycardia. When the hypothalamus or pituitary gland is damaged, endocrine disorders develop. Symptoms of the disease depend on the location of the tumor in a specific part of the brain responsible for certain functions.
Primary
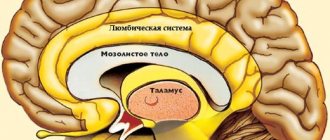
When astrocytoma is localized in the frontal lobe of the brain, patients experience the appearance of psychopathological symptoms: a feeling of euphoria, decreased criticism of their illness, aggressiveness, emotional indifference, the psyche can completely collapse. If the corpus callosum or the medial surface of the frontal lobes is damaged, patients experience memory and thinking impairment. When Broca's area is damaged in the frontal lobe of the dominant hemisphere, motor speech disorders develop. Patients with tumors in the posterior regions develop paresis and paralysis in the upper and lower extremities.
In case of damage to the temporal lobe, patients may experience the appearance of hallucinations: auditory, gustatory, visual, which over time are replaced by generalized epileptic seizures. Often the development of auditory agnosia - a person does not recognize previously known sounds, voices, melodies. An astrocytoma located in the temporal region threatens to dislocate and herniate into the foramen magnum, resulting in almost inevitable death. When the tumor is localized in the temporal and frontal lobes, patients often experience epileptic seizures.
When a tumor affects the parietal lobe of the brain, sensory disturbances, astereognosis, and apraxia in the opposite limb occur (with apraxia, purposeful actions are impaired in a person). Patients experience the development of focal epileptic seizures. If the lower parts of the left parietal lobe are damaged, right-handers experience impairment in speech, counting, and writing.
The least commonly diagnosed astrocytomas are those in the occipital lobe of the brain. Patients with these tumors develop visual hallucinations, photopsia, and hemianopsia (loss of half the visual field of each eye).
Secondary
One of the main signs of cerebral astrocytoma is the presence of paroxysmal or aching diffuse pain in the head. The headache has no clear localization and is caused by intracranial hypertension. In the early stages of the disease, the pain is paroxysmal and aching, but over time it becomes constant, which is associated with the progression of the tumor.
In patients with cerebral astrocytoma, intracranial pressure increases as a result of compression of the cerebrospinal fluid ducts and venous vessels. Headaches, vomiting, persistent hiccups appear, cognitive functions and visual acuity decrease. Severe cases are accompanied by a person falling into a coma.
Localization
A cyst with a node is more typical for infratentorial tumor localization, and a solid formation for supratentorial one.
Fig.4
Tumor cyst in the cerebellar hemisphere (asterisks in Fig. 4 and arrow heads in Fig. 4), leading to narrowing of the fourth ventricle and causing occlusive hydrocephalus with expansion of the ventricular system (arrow heads in Fig. 4).
When localized in the posterior cranial fossa (60%), the tumor can originate anywhere in the cerebellum—from the hemisphere or vermis [91].
Fig.5
Pilocytic astrocytoma grows along the optic tracts (arrow heads in Fig. 5), and is also unevenly contrasted (arrow heads in Fig. 5).
Fig.6
Supratentorially localized in the area of the bottom of the third ventricle (often associated with NF1) and chiasma (25 - 30%).
Cystic-solid formation in the region of the third ventricle (arrowheads in Fig. 6). Traces of surgical treatment in the form of damage to the trunk of the corpus callosum (arrow in Fig. 6). The tumor is not completely removed (arrow in Fig. 6), a heterogeneous conglomerate heterogeneously accumulates contrast (arrow head in Fig. 6).
Other, less common sites: the brain stem, cerebral hemispheres, and ventricles of the brain (more common in adults).
Diagnosis: types of tumor
The structure of malignant cells divides astrocytomas into two groups:
- fibrillar, gemistocytic, protoplasmic.
- piloid (pilocytic), subepidemic (glomerular), cerebellar microcystic.
Astrocytoma has several degrees of malignancy:
- first degree of malignancy - this type of benign tumor grows slowly, is small in size, is limited to healthy areas of the brain by a kind of capsule, and rarely affects the development of neurological deficits. The tumor is represented by normal astrocyte cells, which develop in the form of a nodule. A representative of such a tumor is piloid astrocytoma, pilocytic. Affects children and adolescents more often;
- second degree of malignancy - the tumor grows slowly, the cells begin to differ from normal brain cells, more common in young people aged 20 to 30 years. A representative of this degree of malignancy is fibrillar (diffuse) astrocytoma;
- third degree of malignancy - anaplastic astrocytoma. Grows rapidly, tumor cells are very different from normal brain cells, the tumor has a high level of malignancy;
- fourth degree - malignant glioblastoma, the cells do not look like normal brain cells. It affects important centers of the brain, grows quickly, and often it is impossible to remove such a tumor. It affects the cerebellum, the cerebral hemispheres, and the area of the brain responsible for the redistribution of information from the sensory organs - the thalamus.
Over time, tumor cells of the first and second degrees degenerate and turn into cells of the third and fourth degrees of malignancy. Transformation of a tumor from a benign to a malignant neoplasm most often occurs in adults. Benign brain tumors can be as life-threatening as malignant tumors. It all depends on the size of the formation and the location of the tumor.
general characteristics
Pilocytic astrocytoma is more common in children, located infratentorially, and representing a cyst (asterisk in Fig. 29) with a parietal node (arrowhead in Fig. 1). It is less common in adults, mainly in the form of a solid formation and is located supratentorially (arrowhead in Fig. 2).
Fig.1
Fig.2
Treatment of astrocytoma
Treatment tactics for brain tumors depend on the location of the tumor, its size, and the type of tumor. A favorable prognosis in the treatment of diffuse astrocytoma exists for young patients, provided that the brain tumor is completely removed. Anaplastic astrocytoma is treated using a combined approach - surgery, radiation therapy, and polychemotherapy. The average life expectancy is about three years after surgery. The prognosis is favorable for young people who were in good health before surgery, provided that the tumor was completely removed.
Pilocytic (piloid) astrocytoma develops in children, has limited growth, characteristic localization, and morphological features. Treatment of the tumor has a favorable prognosis due to its slow growth and low malignancy. Treatment is carried out by surgery and complete removal of the tumor, which in some cases is not possible due to the location of the tumor in the hypothalamus or brain stem. Some types of piloidal astrocytomas (hypothalamic) have the ability to metastasize.
Clinical picture, treatment and prognosis
Clinical manifestations in children are quite pronounced, characterized by cerebellar symptoms (ataxia, nystagmus) and a set of symptoms of intracranial hypertension due to occlusive hydrocephalus. With total removal, the prognosis is good, survival is high, and relapses are rare. PA is slowly increasing, prognosis (more than 90% with 5-year survival and more than 70% with 20-year survival). Some surgeons advocate only resection of the nodule, since the walls of the cyst do not contain tumor elements, even if they become stronger. If removal is not possible, it is replaced by palliative treatment (ventriculo-atrial and ventriculo-peritoneal shunting). Cystic tumors have a better prognosis. The clinical course is benign, even with incomplete surgical resection, the 5-year survival rate is 90-100%, relapses are rare.
Author: radiologist, Ph.D. Vlasov Evgeniy Alexandrovich
Full or partial reprint of this article is permitted by installing an active hyperlink to the source
Brain astrocytoma: consequences after surgery
The consequences after surgery for astrocytoma depend on the size of the tumor and its location. Benign astrocytomas, located in an accessible location, give a better prognosis for life expectancy than high-grade astrocytomas or benign astrocytomas, located in a location inaccessible to the surgeon and having a large tumor size. After removal of an astrocytoma, tumor recurrence often occurs, which occurs within two years after surgery. The earlier a tumor is detected, the better the prognosis for its treatment.
Classification by cellular structure
Astrocytomas can be divided into groups according to their predominant cell type. The basis for dividing astrocytomas into “ordinary” and “special” is the significant difference in the clinical course and the significantly more favorable nature of the latter, which does not depend on the gradational degree within this group (they also more often occur in youth). The current understanding is that pilocytic and microcystic cerebellar astrocytomas are the same tumors as fibrillary astrocytomas, but only with a different location.
Forecast
After surgical removal of nodular forms of astrocytoma, long-term remission (more than ten years) can occur. Diffuse astrocytomas are characterized by frequent relapses, even after combined treatment.
With glioblastoma, the average life expectancy of a patient is one year, with anaplastic astrocytoma of the brain - about five years.
With other types of astrocytomas, the average life expectancy is much longer; after adequate treatment, they return to a full life and normal work activity.
Rehabilitation period
After removal of a brain astrocytoma, rehabilitation takes place in a medical center. After the surgery is completed, the patient will remain in the intensive care unit for a week or more. He is under 24-hour surveillance. A few days after surgical treatment, specialists prescribe magnetic resonance imaging or x-ray diagnostics.
If there are no complications after surgery, recovery continues in the rehabilitation center. The program includes physical therapy, massage, speech therapy correction and other techniques that allow the patient to restore impaired functions and normal quality of life.
Rehabilitation after surgery for astrocytoma and surgical removal of the tumor lasts 2-3 months. At this time, the patient must follow the recommendations of the attending physician and rehabilitation specialist, and undergo diagnostics to monitor the characteristics of recovery.
Radiation therapy
Radiation therapy for the treatment of astrocytoma most often begins after surgery and removal of the formation. But it is possible to use the technique before surgery in order to reduce the tumor. Radiation therapy also destroys remaining abnormal cancer cells after surgery.
If the formation is inoperable, surgery is not performed, but the patient requires palliative care. Radiation exposure can reduce the pathological focus and increase the patient's life expectancy. The specific method is selected by specialists based on the diagnostic results and the general health of the patient.
A type of radiation treatment is brachytherapy. The method involves the introduction of radioactive substances directly into the malignant tissues themselves. In this case, healthy cells are preserved in full and there is no need to remove functional areas of the brain.
Chemotherapy
Chemotherapy is an addition to surgical removal of astrocytoma. Cytostatic drugs destroy malignant cells when they enter the bloodstream and are distributed throughout the body. Chemotherapy is carried out in short courses and under the supervision of specialists.