Extramedullary tumor
An extramedullary tumor is a tumor localized in the anatomical structures surrounding the spinal cord (roots, vessels, membranes, epidural membrane. Extramedullary tumors are divided into subdural (located under the dura mater) and epidural (located above this membrane). Most extramedullary tumors are meningiomas (arachnoidendotheliomas) and neuromas .
Extramedullary meningioma (arachnoidendothelioma)
Meningiomas are the most common extramedullary tumors of the spinal cord (approximately 50%). Meningiomas are usually located subdurally. They belong to the meningeal-vascular tumors, originate from the meninges or their vessels and are most often tightly fixed to the dura mater.
Extramedullary neuroma
Neuromas occupy the second place among extramedullary tumors of the spinal cord (approximately 40%). Neuromas, developing from Schwann elements of the spinal cord roots, are tumors of dense consistency. Neuromas are usually oval in shape and surrounded by a thin, shiny capsule. In the tissue of neuromas, regressive changes are often found with decay and the formation of cysts of various sizes.
Clinical manifestations of extramedullary tumors
Any lesion that leads to a narrowing of the spinal cord canal and affects the spinal cord is accompanied by the development of neurological symptoms. These disorders are caused by direct compression of the spinal cord and its roots, but are also mediated through hemodynamic disorders.
With extramedullary tumors (both intradural and epidural), symptoms of compression of the spinal cord and its roots appear. The first symptoms are usually local back pain and paresthesia. Then there is a loss of sensitivity below the level of pain, dysfunction of the pelvic organs.
The clinical picture of extramedullary tumors consists of three syndromes:
- radicular;
- half spinal cord syndrome;
- syndrome of complete transverse spinal cord lesion.
The exception is the clinical picture of damage to the cauda equina of the spinal cord (symptoms of multiple damage to the spinal cord roots from the L1 level).
Extramedullary tumors are characterized by early onset of radicular pain, objectively detectable sensitivity disorders only in the area of the affected roots, reduction or disappearance of tendon, periosteal and skin reflexes, the arcs of which pass through the affected roots, local paresis with muscle atrophy according to the lesion of the root.
As the spinal cord is compressed, conduction pain and paresthesia with objective sensitivity disorders occur. When the tumor is located on the lateral, anterolateral and posterolateral surfaces of the spinal cord, in the case of predominant compression of its half, in determining the stage of development of the disease, it is often possible to identify the classic form or elements of Brown-Séquard syndrome.
Over time, symptoms of compression of the entire diameter of the brain appear and this syndrome is replaced by paraparesis or paraplegia. Decreased strength in the limbs and objective sensory disturbances usually first appear in the distal parts of the body and then rise upward to the level of the affected segment of the spinal cord.
The symptom of a cerebrospinal fluid push is a sharp increase in pain along the roots irritated by the tumor. This increase occurs when the jugular veins are compressed due to the spread of increased cerebrospinal fluid pressure to the “displaced” extramedullary subdural tumor. With extramedullary tumors, especially if they are located on the posterior and lateral surfaces of the brain, radicular pain and sometimes conduction paresthesia often occur with percussion or pressure on a certain spinous process.
How to recognize a spinal tumor?
Even benign tumors can be accompanied by unpleasant symptoms, such as pain and neurological disorders. You should be aware of the typical signs of a spinal tumor:
- Back pain, which is most often localized but can spread to other areas.
- Loss of sensation in the arms and legs (depending on the location of the tumor).
- Muscle weakness.
- Difficulty walking (especially with a tumor in the lumbar region).
- Bowel and bladder dysfunction.
- Paralysis.
Since all the above symptoms can be associated with other diseases, it is important to undergo a thorough examination to determine the exact cause of their occurrence.
Intramedullary tumor
An intramedullary tumor is a tumor localized in the substance of the spinal cord. The incidence of intramedullary tumors is 10-18% of the total number of spinal cord tumors. If by their nature intramedullary tumors are often benign and slowly growing, then by their nature of growth and location they are the least favorable from the point of view of the possibility of their surgical removal. Intramedullary tumors of the spinal cord are mainly represented by gliomas ( ependymomas and astrocytomas ). Less commonly found are spongioblastoma multiforme, medulloblastoma, and oligodendroglioma.
Intramedullary ependymoma
Ependymomas most often arise from the ependyma of the central canal at the level of the cervical and lumbar thickenings. They can also develop from the filament terminale and be located between the roots of the cauda equina. Ependymomas are the most common intramedullary tumors. In 50-60% of cases, ependymomas are located at the level of the conus of the spinal cord and the roots of the cauda equina. This is followed by the cervical and thoracic spinal cord. Unlike the cervical and thoracic levels, where the tumor causes thickening of the spinal cord, at the level of the conus and roots it acquires all the properties of an extramedullary tumor. Sometimes ependymomas in this area can completely fill the spinal canal, reaching 4-8 cm in length. Ependymomas are classified as benign, slow-growing tumors. They differ from other spinal cord gliomas in their abundant blood supply, which can lead to the development of subarachnoid and intratumor hemorrhages. In more than 45% of cases, ependymomas contain cysts of varying sizes.
Intramedullary astrocytoma
Astrocytomas are characterized by infiltrative growth, are localized in the gray matter and are widely distributed along the length of the brain. Astrocytoma is the second most common intramedullary tumor after ependymoma in adults and accounts for 24-30% of all intramedullary neoplasms. In this age group, the peak incidence of tumors occurs in the 3rd and 4th decades of life. In children, on the contrary, astrocytoma is observed more often than ependymomas, accounting for up to 4% of all primary tumors of the central nervous system.
Diagnosis of intramedullary tumors
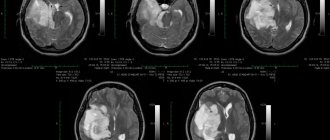
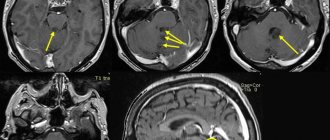
Radiological diagnosis of intramedullary tumors is quite widely developed, but most methods that can adequately judge the presence of a tumor lesion are labor-intensive and traumatic. One of the most sensitive methods in determining changes in the size of the spinal cord is magnetic resonance imaging (MRI), therefore, if the presence of an intramedullary tumor is suspected, the growth of which is usually accompanied by thickening of the spinal cord, the use of MRI should be considered the most appropriate.
Tumors of the spine and spinal cord
Tumors of the spine and spinal cord
Recurrent back pain is a common problem. Most cases of pain are the result of normal strains and strains or degenerative changes that occur with age.
But sometimes the cause of pain can be a spinal tumor - a malignant or benign neoplasm that develops in the spinal cord, its membranes or in the bones of the spine.
Tumors of the spine and spinal cord are a fairly rare pathology and account for no more than 0.5% of all cancers. Like tumors of other organs, they can be benign or malignant. Tumors of the spinal cord can originate both from its membranes (extramedullary) and from the white or gray matter itself (intramedullary). Treatment of tumors in the vast majority of cases is surgical: the tumor is removed with the integral use of an operating microscope.
Clinical picture
Back pain, especially in the middle or lower part, is the most common symptom of both benign and malignant spinal tumors. The pain can often be worse at night or upon waking. It can also spread through the spine to the legs, feet, or arms and may get worse over time despite treatment. Depending on the location and type of tumor, other signs and symptoms may develop, especially as the cancer grows and affects the spinal cord or nerve roots, blood vessels, or bones of the spine. These symptoms include:
- Loss of superficial sensation in the extremities (decreased sensitivity to pain, heat and cold)
- The appearance of deep sensitivity disorders in the limbs - the patient ceases to feel the approach of the floor with his feet
- The appearance of muscle weakness in the limbs (paresis), which can vary in location and severity depending on where the tumor is located and what part of the spinal cord it compresses
- Difficulty walking due to spasticity in the limbs, sometimes leading to falls
- Deterioration of bowel and/or bladder function, up to complete dysfunction of the pelvic organs (delayed bowel movements and urination, incontinence)
- Scoliosis or other spinal deformity caused by a large but benign tumor.
Spinal tumors progress at different rates. In general, malignant tumors grow quickly, while benign tumors can grow slowly, sometimes existing for several years before problems arise.
Types of spinal tumors
Spinal tumors are classified according to their location in the spine.
Extradural (vertebral) tumors.
Most tumors that affect the vertebrae spread to the spine from another location in the body, often from the prostate, breast, lung, or kidneys. Although primary cancer is usually diagnosed before significant back problems develop, back pain may be the first symptom of the disease in patients with metastatic spinal tumors.
Cancers originating in the bones of the spine are less common. These include osteosarcomas (osteogenic sarcomas), the most common type of bone cancer in children, and Ewing's sarcoma, a particularly aggressive tumor that affects young people. Multiple myeloma is a cancer of the bone marrow—the porous interior of bone that produces blood cells—that most often develops in adult patients.
Benign tumors such as osteoid osteomas, osteoblastomas, and hemangiomas can also develop in the bones of the spine, causing long-lasting pain, curvature of the spine (scoliosis), and neurological impairment.
Intradural-extramedullary tumors . These tumors develop in the dura mater of the spinal cord (meningiomas), in the nerve roots emerging from the spinal cord (schwannomas and neurofibromas), or at the base of the spinal cord (ependymomas). Meningiomas most often develop in women aged 40 years and older. They are almost always benign and are easy to remove, but sometimes they can recur. Nerve root tumors are usually benign, although neurofibromas, with prolonged growth and large tumor sizes, can develop into malignant ones. Ependymomas located at the end of the spinal cord are often large in size; their treatment can be complicated by fusion of the tumor with the roots of the cauda equina located in this area.
Intramedullary tumors . These tumors originate inside the spinal cord. Most are astrocytomas (which most often develop in children and adolescents) or ependymomas, the most common type of spinal cord tumor in adults. Vascular hemangioblastomas of the spinal cord are often intramedullary tumors. Intramedullary tumors can be either benign or malignant and, depending on their location, they can cause numbness, loss of sensation, or changes in bowel or bladder function. In rare cases, tumors from other parts of the body can metastasize to the spinal cord.
Diagnostics
Spinal tumors can sometimes go undiagnosed because they are rare and their symptoms resemble those of more common diseases. For this reason, it is especially important that your doctor obtain a complete history and perform a physical and neurological examination. If a spinal tumor is suspected, your doctor may order one or more of the following tests to confirm the diagnosis and identify the location of the tumor:
- Magnetic resonance imaging (MRI)
- Computed tomography (CT)
- Myelography
During myelography, a contrast agent is injected into the patient's spinal canal. The contrast agent then travels through the spinal cord and spinal nerves and appears white on X-rays and CT images. Because this test carries more risks than an MRI or traditional CT scan, myelography is not usually the first choice for diagnosis, but it may be used to identify compressed nerves.
- Biopsy
The only way to determine whether a tumor is benign or cancerous is to examine a small sample of tissue (biopsy) under a microscope. How the sample is obtained depends on the patient's health and the location of the tumor. The doctor may use a thin needle to remove a small amount of tissue, or a sample may be obtained during surgery.
Treatment
Ideally, the goal of treating a spinal tumor is complete removal, but this goal is complicated by the risk of permanent damage to surrounding nerves. Doctors must consider the patient's age, general health, type of tumor, and whether it is primary or has spread to the spine from other organs (metastasized).
Sometimes spinal tumors are discovered before they cause symptoms, often during a physical examination for another condition. If small tumors are benign and are not growing or pressing on surrounding tissue, close observation may be the only treatment option necessary. This is especially true for older people, for whom surgery and radiation therapy carry high risks. If you decide not to have surgery for a spinal tumor, your doctor will recommend periodic imaging to monitor the growth of the tumor.
Surgical treatment
New techniques and tools are allowing neurosurgeons to access tumors that were previously inaccessible. Powerful microscopes used in microsurgery make it possible to differentiate between tumor and healthy tissue.
Doctors can probe various nerves during surgery using electrodes, reducing the possibility of neurological damage. In some cases, doctors may use an ultrasonic aspirator, a device that uses ultrasound to destroy the tumor and remove remaining fragments.
Even taking into account modern advances in the treatment of tumors, not all of them can be completely removed. Surgical removal is the best option for many intramedullary and intradural-extramedullary tumors, but large ependymomas located in the terminal spine may not be removed due to the large number of nerves in that area. Although benign tumors in the vertebrae can usually be completely removed, metastatic tumors are usually not resectable.
Radiation therapy
This therapy is used after surgery to destroy remaining tissue that cannot be removed or to treat inoperable tumors. This treatment is usually the first-line treatment for metastatic tumors. Radiation may also be used to relieve pain or if surgery carries too many risks.
Patient prognosis
The following factors are of greatest importance in determining the prognosis of the disease:
1. Type of tumor (malignant, benign, primary or secondary, and specific type).
2. Anatomical location - determines the possibility or impossibility of radical surgery.
3. Timely diagnosis and treatment - the earlier the tumor was detected, the higher the chances of a complete cure.
4. The patient’s age and the presence of concomitant diseases will affect the choice of treatment method.
5. Presence of metastases to other organs.
Types of benign spinal tumors
Enostosis (bone island) is a latent formation that is usually discovered incidentally during radiology. It usually does not require treatment.
Osteoid osteoma. It is an active benign tumor that most often occurs in children and adults, usually in men. In the spine, it most often occurs in the lumbar region, a little less often in the cervical region. It can cause scoliosis, radicular pain, and gait disturbance and must be treated to avoid further complications. Usually treated with surgery.
Osteoblastoma. This spinal tumor is similar in origin to the previous one, but manifests itself differently. It usually develops in adults aged 20–30 years, and is more common in men than women (incidence ratio 3:2). Osteoblastoma can develop in the cervical region (rarely in the lumbar and thoracic) and spread to the vertebral body. Symptoms include a dull, localized pain, paresthesia, or even paralysis if the tumor is large enough. In an aggressive stage, osteoblastoma can lead to calcification and sclerotic deposits; in an advanced form, it can spread to and destroy bones, leak into tissues and cause significant calcium deposits. Osteoblastoma is treated surgically, but sometimes there is a risk of damage to vital vessels and nerves, so the operation must be performed with the highest precision.
Aneurysmal bone cyst. These are benign cysts, which are multi-chambered inclusions in the bones filled with blood. The thoracic spine is most often affected, followed by the cervical and lumbar spine. The possibility of damage to the vertebral body is 75%. The formations can irritate nearby tissues, vertebrae and discs. CT and MRI can detect inclusions with fluid inside. Surgery can get rid of the tumor, but there is a high risk of its recurrence.
Results of MTR examination for spinal oncology
Magnetic resonance imaging equipment shows pathological degeneration of tissues, changes in blood supply to the studied areas of the spine, determines transformations of the boundaries, size and shape of internal organs. Layer-by-layer images show a clear and detailed picture of oncology from the early stages to metastasis of cancer cells to neighboring tissues and regional lymph nodes.
MRI detects vascular tumors, formations of nervous structures (including the brain and spinal cord), soft tissues, and parenchyma of internal organs. To increase information content and detect oncology in the initial stages, a contrast agent is used. The tomograph images clearly show the malignancy of benign neoplasms.
Important!
The MRI method is reliable and informative. But based on his data, the radiologist does not make a final diagnosis. The purpose of the study is to recommend additional examination and detect indirect signs of oncology.
If the results show a cancerous process, laboratory tests are prescribed and a tissue sample is taken for a biopsy.