24.11.2016
Pinchuk Elena Anatolyevna
Deputy chief physician for medical work, kmn, neurologist, doctor of physical and rehabilitation medicine
Lipovka Nadezhda Sergeevna
Head of the Department of Medical Rehabilitation, Physician of Physical and Rehabilitation Medicine, Neurologist
Sobolev Arkady Igorevich
Doctor of physical and rehabilitation medicine, neurologist
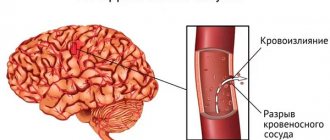
Normally, a person has elastic and strong blood vessels. However, high blood pressure and a number of other threatening factors make blood vessels fragile, as a result of which they are easily damaged. Such damage leads to a serious brain disease - stroke. Lesions may appear in different parts of the brain. One of the most dangerous places of occurrence is the brain stem. Hence the name of the disease – brainstem ischemic stroke.
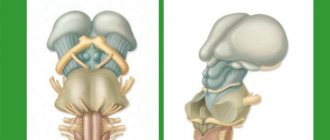
The brain stem is an important link between the brain and the spinal cord. It is through it that all impulses and commands enter the human body. A brainstem stroke is dangerous because hemorrhage in this area completely blocks the normal functioning of other parts of the brain: the cerebellum, the middle and medulla pons, the pons, and the entire thalamic region. A lesion in this area not only disables facial muscles, eye movement, but also important centers that are responsible for blood circulation, breathing, and thermoregulation. An atrophied brainstem disrupts the functioning of all human internal organs.
Causes of brainstem stroke
Brainstem stroke occurs for the same reasons as other stroke subtypes:
- Poor nutrition;
- Constant and prolonged stress;
- Increased blood cholesterol levels;
- Overweight;
- Abuse of hormonal drugs;
- Alcohol and smoking;
- Bleeding disorders;
Often, a stroke can occur against the background of existing diseases, such as hypertension, rheumatism, vascular atherosclerosis, diabetes mellitus.
The danger of a brainstem stroke is that it develops very quickly and suddenly. Although it is accompanied by almost the same symptoms as ischemic stroke:
- Speech and articulation disorder;
- Dizziness, pale skin;
- Sweating;
- Fluctuations in body temperature;
- Rapid pulse, tachycardia;
- High blood pressure;
- Impaired functioning of the facial muscles, which leads to asymmetry and strabismus;
- Violation of movements, breathing, speech.
In some cases, paralysis may occur, affecting all parts of the body. However, a person does not lose his thinking abilities. Already in the process of treatment and recovery after a stroke, he is able to understand and evaluate what is happening.
If at least one of the above symptoms appears, you should call a doctor. The sooner a diagnosis is made and treatment is started, the greater the victim’s chance of recovery. A brainstem stroke is diagnosed using MSCT and MRI, and a neurologist also checks the state of the cardiovascular system and respiratory function.
Classification, risk factors
Paying attention to the causes, the following types of brain strokes are distinguished:
- Ischemic - lack of blood supply due to the fact that blood does not flow to the brain tissues, as a result, the cells “starve” and then die from “hunger”.
- Hemorrhagic - damage to brain structures due to hemorrhage.
Hemorrhagic stroke, according to statistics, occurs less frequently than ischemic stroke, but is many times more dangerous, and its course is more severe.
Ischemic stroke of the brain stem occurs due to the following factors:
- Increased blood viscosity (with congenital pathologies of blood clotting, excessive use of certain medications).
- Constriction of blood vessels in patients with hypertension.
- Vasoconstriction in experienced smokers.
- Accumulation of cholesterol on the inner lining of blood vessels.
- Blockage of blood vessels by blood clots that are “born” in the cavities of the heart due to atrial fibrillation along the bloodstream to the brain.
The onset of hemorrhagic stroke is expected due to reasons such as:
- Sharp jumps in blood pressure.
- Overdose of anticoagulant drugs.
- Long-term chronic pathologies of cerebral vessels (arteritis, aneurysms).
If changes in the blood vessels of the brain are not very pronounced, a microstroke develops, rehabilitation for which and the previous therapy give faster and more effective results.
Treatment of brainstem stroke
The main therapy is aimed at eliminating the cause of the lesion - a blood clot or hemorrhage. Hematomas are removed surgically. If blood clots form, therapy is used to dissolve and prevent their formation. Drugs that thin the blood, regulate cholesterol levels, and control heart rate are administered. If respiratory function is lost, a special tube is inserted into the person's trachea to provide oxygen.
In most cases, a brainstem stroke leads to death, since most of the vital functions of the human body stop working. In order to avoid such a serious disease as a brainstem stroke, it is important to be regularly examined by doctors if you have other diseases of the cardiovascular system. It is also necessary to give up bad habits, lead a healthy lifestyle, and eliminate stressful situations from your life as much as possible.
Clinical Brain Institute Rating: 4/5 — 17 votes
Share article on social networks
Impaired mental functions due to damage to the brain stem
The brain stem is an extended formation that continues the spinal cord and includes the medulla oblongata, pons and midbrain.
Lesions of the trunk most often occur as a result of tumors in the posterior cranial fossa, as well as with closed craniocerebral injuries, causing compression of the area in question and hemorrhage.
A study of traumatic lesions of the brainstem shows that diffuse axonal damage (DAD) of the brain in this area ranks third among all DADs in closed head injuries.
This damage occurs due to acceleration, compression and rotation of the head, resulting in tension and rupture of axons in the white matter of the brain, accompanied by pinpoint hemorrhages.
Rich neurological symptoms when the trunk is damaged are combined with disorders of higher mental functions. Thus, after loss of consciousness, amnesia for the events preceding the injury often occurs.
In the future, patients may experience disturbances in the sleep-wake cycle and increased exhaustion. However, in the long-term period after the injury, the consciousness of patients is clear, they are correctly oriented in place, time and their own personality. Patients present adequate complaints and are critical of their condition.
The central symptoms are modality-nonspecific mnestic disorders with primary short-term memory disorders. There is a narrowing of the volume of direct memorization to 3–4 words, and an increase in the inhibition of traces by external stimuli.
However, strengthening motivation or organizing the memorized material according to its meaning gives a clear compensatory effect, which indicates the general intellectual and mnestic safety of patients.
The category of patients under consideration is also characterized by attention disorders of a modality-nonspecific type. Patients are absent-minded and cannot concentrate on one task for a long time.
Thus, when performing a test on a serial count, they often make mistakes, but when they are pointed out, they try to make corrections. Increasing motivation and speech control make it possible to compensate for these defects. A characteristic feature of these disorders is also the fluctuation of symptoms and their different severity on different experimental days.
In the literature there are various references to the frequency and nature of mental disorders with damage to the pons and medulla oblongata.
Symptoms range from transient disturbances of consciousness to pathological drowsiness, severe and persistent memory disorders, lethargy or states of agitated excitement with affects that look like a manic state (if the anterior parts of the trunk are affected).
Mental disorders were noted in 38% of cases of infiltrating tumors of the trunk. In general, acute transient psychoses after operations on the pons and medulla oblongata occur less frequently than after operations on the cerebral hemispheres.
Differences in the structure and dynamics of psychoses in brainstem pathology were noted - rapid disruption and restoration of consciousness with secondary functional inhibition of cortical activity.
Patients brought out of sleep-like stupor answer questions correctly and provide anamnestic information. They have a relative preservation of personality, the possibility of a catatonic syndrome with amymia and general stiffness.
A.L. Abashev-Konstantinovsky described the following possible violations:
- attacks of olfactory hallucinations with astrocytoma of the pons;
- state of mild stupor, partial sensory and motor seizures in brain stem glioma;
- speech motor restlessness, distractibility, gross disorientation in place and time, speech agitation.
T.A. Dobrokhotova describes in her monograph a patient whom she observed after removal of a brainstem hematoma in the pons area. On the fourth day after the operation, he developed acute psychosis with hallucinatory experiences.
Hallucinations were distinguished by such features as:
- complexity (a combination of visual and auditory hallucinations with the subsequent addition of tactile ones);
- appears when the eyes are closed and disappears when they are opened;
- predominant appearance in the evening and night hours;
- the content of hallucinations in the form of visual images and voices of loved ones;
- preservation of a critical attitude towards hallucinations in most episodes;
- appearance against a background of hearing loss and tinnitus.
The confusion of consciousness in the described patient was characterized by experiences of influence: he claimed that he was “held upside down.”
The patient also experienced psychomotor agitation, anxiety, and visual illusions. After clearing consciousness, the patient reproduced the content of his experiences. In general, the patient's postoperative psychosis was characterized by relatively rapid and complete regression.
In a study of 24 patients with brainstem infarctions, significant similarity in symptoms was revealed when comparing the results of tests performed in 43 patients with infarctions in the cerebellar region.
In both cases, changes in mental functions manifested themselves in the form of dysregulation and delayed reproduction. Optical-spatial functions suffered to a lesser extent.
Another study presents observational data on 25 patients with brain stem infarctions, which notes that with rostral and medial lesions in the pons, neglect of the motor defect, paraphasia and violent laughter are observed.
S.B. Buklina analyzed UPF disorders in 25 patients before and after surgery to remove hematomas, cavernomas and arteriovenous malformations. A neuropsychological examination conducted before surgery showed that only 2 patients had no symptoms of HMF disorder.
Most often, patients with lesions of the brainstem experienced symptoms that were similar to symptoms of lesions in various parts of the frontal lobes.
The identified symptoms associated with a violation of the factor of the kinetic organization of serial movements and actions completely coincided with similar disorders with damage to the premotor zone of the cerebral hemispheres.
Another group of symptoms was less common and manifested itself in the form of disturbances in programming and control of activity, similar to those that occur with damage to the prefrontal parts of the frontal lobes.
Significantly less common were symptoms that were similar to dysfunction of the medial parts of the frontal lobes, manifested in the form of impairments in criticism of one’s condition and orientation in time.
In the literature there are descriptions of cases of successful operations to remove malignant tumors of the pons. These data are of great interest because they make it possible to assess the scale of compensatory changes occurring in patients after surgery.
Thus, one of the studies describes an 11-year-old patient who underwent total removal of a bulky malignant glioma of the right half of the pons. Before the operation, the patient complained of severe dizziness and unsteadiness of gait.
On neurological examination, the patient was clearly conscious. The author notes large-scale horizontal and vertical nystagmus, deviations to the right in the Romberg position, and decreased pain and tactile sensitivity on the left as the main symptoms.
Within 7–10 days after the operation, a picture of frontal syndrome was observed in the form of uncriticality, foolishness and loss of self-control over behavior. According to the neurologist, the patient had severe cerebellar syndrome.
Neuropsychological examination 3 weeks after surgery and psychophysiological examination with EEG monitoring 4 weeks later revealed a complex picture indicating dysfunction in different parts of the cerebral hemispheres.
During the neuropsychological examination, mirror performance of Head's tests was observed in half of the presentations, disturbances in the transfer of postures of the fingers from left to right in 66% of presentations, while the transfer from right to left was intact.
When performing a graphic test, violations of program retention were observed with perseverative replacement by repetition of one element instead of two against the background of pronounced megalography.
In tests for visual gnosis, difficulties were noted in recognizing crossed out, superimposed and under-drawn images. Counting operations involving passing through tens and serial counting turned out to be inaccessible, as was the understanding of many logical-grammatical constructions.
Just as in tests for auditory gnosis, the patient complained: “I can’t imagine.” At the same time, the patient did not have any difficulties with the task of understanding prepositional constructions, performed with visual support (test “Barrels and boxes”).
In the tactile sphere, this patient showed disturbances in somatosensory afferent synthesis. Accurate performance of touch localization tests was complicated by the inaccessibility of the dermolexia test on both hands.
Stereognosis was completely preserved in the right hand, and only in half of the presentations in the left. These results clearly indicate the involvement in the pathological process of connections between parietal structures and the nuclei of the thalamus, caudate nucleus and cerebellum.
In general, the identified symptom complex was a combination of “cerebellar” syndrome with “disconnection” of cortical-cerebellar connections, resulting in a postoperative deficit in the integrative dynamic organization of mental activity.
4 months after the operation, this patient showed adaptive changes in neurophysiological activity, which made it possible to significantly compensate for the resulting neurological and neuropsychological deficit. Thus, horizontal nystagmus disappeared, statics and coordination improved significantly.
The patient's visual, auditory and tactile gnosis was almost completely restored, copying according to a model and performing graphic tests improved, and impairments in counting and understanding logical-grammatical structures disappeared.
Thus, damage to the brain stem leads to disorders of various cognitive functions, which are often reversible.
Programs:
Assessment of rehabilitation potential
Movement restoration
Rehabilitation after stroke
Restoration of cognitive functions
Early (resuscitation) rehabilitation