Home>Articles>Alcoholic epilepsy
quick menu (hide)
- Reasons for appearance
- How does an attack go?
- Consequences and risks
- How is the treatment carried out?
- Treatment of alcoholism as a solution to the problem
Alcoholic epilepsy is a type of psychosis caused by prolonged consumption of alcohol in large doses. It usually appears at the 3rd stage of addiction. In the presence of external catalytic factors, it may appear earlier. At the initial stages, it does not have a pronounced form of seizures with tremor and paralysis, but rather manifests itself in irritability, absent-mindedness and other sudden changes in behavior. Without taking measures, it further develops to a state of pronounced epileptic seizures.
An alcoholic epilepsy attack occurs suddenly, so the disease is primarily dangerous for the person who drinks. However, manifestations of aggression and anger in the later stages are dangerous for others, since during a seizure, a person does not control his own behavior.
Reasons for appearance
The causes of alcoholic epilepsy, like most other pathologies in alcoholics, come down to organ disorders caused by the influence of alcohol. In this case, we are talking about damage to the brain. The fact is that long-term consumption of alcohol, especially with periodic heavy binges, leads to the accumulation of toxic substances and breakdown products of ethyl alcohol in the body. They affect all organs and lead to problems in the blood supply to the brain, which in turn causes irreversible and destructive consequences.
The problem is cumulative in nature, invisible in the initial stages, and becomes more and more noticeable after the 2nd stage of alcoholism. Therefore, most often, the disease manifests itself in alcoholics with a long history of addiction. However, in some cases, alcoholic epilepsy develops faster due to additional factors damage , for example, due to trauma, severe viral infections.
Alcohol for epilepsy
There is still no specific mechanism Scenarios for the development of the disease vary, but most often they come down to the following:
- A case associated with the appearance of seizures during intoxication with alcohol. The consequence of acute alcohol intoxication may be the first occurrence of the disease, even in the absence of seizures in the past.
- A case where an alcoholic abruptly stops drinking alcohol after prolonged use. As a result of acute withdrawal syndrome and alcohol damage to the nervous system and brain, seizures often occur.
It should be noted that the appearance of alcoholic epilepsy does not link the disease only to the consumption of alcoholic beverages. In other words, a disease that arose during alcoholism can become progressive even in a sober person.
How does an attack go?
Alcoholic epilepsy, the causes of which lie in disruption of the brain and other organs due to poisoning with the breakdown products of ethyl alcohol, is similar to standard epilepsy. The main and most striking difference is the disturbance of consciousness in alcoholics immediately before and after an attack. The disorder manifests itself in different ways. The patient may be in an unnaturally elevated or, on the contrary, depressed state, and exhibit excessive activity. In some cases, the appearance of auditory and sound hallucinations is observed.
Before, as well as during the seizure itself, a person behaves as follows:
- An attack can start with muscle pain, a compressive or acute headache;
- Due to contraction of the vocal cords, the patient experiences loud, uncontrollable screams;
- Uncontrolled urination occurs;
- Control of consciousness disappears, manifesting itself in different ways, from hallucinations to hysterics and aggression;
- A seizure is accompanied by muscle contractions resembling convulsions, tension in the limbs and other muscles of the body;
- The pulse increases noticeably - up to 170 beats per minute, while breathing, on the contrary, slows down due to tension in the lungs. The respiratory rate periodically decreases to 8 exhalations per minute;
- There is arching of the body due to muscle contraction; depending on the area of brain damage, the attack is accompanied by distortion of facial features or spasms of the limbs, or a combination of all symptoms in the most severe cases.
Recovery from an attack occurs quite suddenly. However, after suffering stress, the patient continues to feel pain in the limbs and other muscles, causing temporary paralysis. The pain continues for some time, after which the condition gradually clears up.
Alcoholic epilepsy, the consequences of which can be sad, is one of the manifestations of psychoses caused by alcoholism. Seizures rarely occur during heavy drinking. As a rule, they occur on the second or third day after, especially with a sharp exit from binge drinking. In some cases, there may be precursors of an attack, manifested in the form of headaches, dry mouth and other manifestations of malaise caused by poisoning.
How to diagnose
A correctly collected history of the disease is of great importance for diagnosing alcoholic epilepsy. Since many diagnostic symptoms are common to the classic form of the disease, nuances such as:
- how does the attack begin?
- what is the duration of the seizures;
- character of sleep.
For those who are close to the patient, the doctor will ask about the form of epileptic seizures, their duration and previous manifestations.
Confirmation of the diagnosis is carried out using clinical tests of urine, blood, computed tomography, MRI, EEG, etc. Their goal is to identify epileptic foci in the brain and promptly prescribe treatment.
Consequences and risks
The consequences of seizures are the most dire, especially if the alcoholic is often left alone. Convulsions are accompanied by loss of coordination and loss of consciousness. In this condition, the patient is capable of injuring himself by falling or further in spasmodic attack. In addition, severe pain and disturbances in the functioning of the heart can provoke many negative consequences, causing a stroke or other problems.
If you do not take action and do not treat both epilepsy itself and alcoholism, which creates a negative background for many other problems, the situation will end in death or irreversible brain damage. If you notice the first symptoms of a seizure or a tendency to have one, you should immediately seek help from specialists.
results
The relatively small number of identified patients - 6.2% - can be explained by two reasons. Firstly, a number of patients could hide the facts of alcohol and/or drug use, so as not to cause a change in attitude on the part of doctors, and secondly, some patients who regularly drink alcohol consider their lifestyle to be completely normal, and the facts of alcohol use are not worthy attention.
Nevertheless, the vast majority (76 people) of those included in the study noted a connection between the attacks and alcohol.
In this group of patients, two main types of connection between alcohol and epilepsy can be distinguished: the development of epilepsy in people who have been abusing ethanol for a long time, and the provocation of epileptic seizures by a single dose of alcohol.
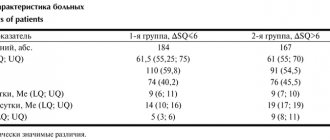
Long-term alcohol abuse was detected in 41 patients. Noteworthy is the high comorbidity of ethanol abuse and acquired structural lesions of the central nervous system: post-traumatic changes during neuroimaging were identified in 13 patients, encephalopathy in 4, a history of ischemic stroke in 1 patient, hemorrhagic in 1. After completion of the examination, the only epileptic seizure provoked by alcohol , was diagnosed in 3 patients, repeated (in the complete absence of seizures not provoked by ethanol use) - in 6, idiopathic generalized epilepsy (IGE) - in 1, cryptogenic epilepsy - in 10, symptomatic - in 19, non-epileptic seizures - in 2. A factor complicating the treatment of patients in the described group was the lack of compliance of the patients: out of 41 patients, 12 did not complete the recommended examination using neuroimaging methods, and a follow-up examination was possible in only 21 out of 41 patients. Among compliant patients, generally satisfactory results of therapy were obtained: remission was achieved in 7 out of 21 (33.3%), improvement in 8 (38.1%), and no effect was noted in 6 (28.6%).
The group of patients who experienced attacks associated with single (or non-systematic) alcohol consumption included 33 patients.
For patients in this group, the presence of acquired structural lesions of the central nervous system was less typical: post-traumatic changes were detected only in 4 patients, tuberous sclerosis, schizencephaly and adrenoleukodystrophy (1 patient each). The structure of epilepsy in the second group also had the following features: a single epileptic seizure provoked by alcohol was diagnosed in 3 patients, repeated ones (in the complete absence of seizures not provoked by the use of ethanol) - in 3, IGE - in 11, cryptogenic epilepsy - in 9, symptomatic - in 7, non-epileptic seizures were not detected in any case. A follow-up examination was carried out in 24 out of 33 cases, remission was achieved in 6 (25%) of 24 patients, improvement in 9 (37.5%), and no effect was noted in 9 (37.5%).
Obviously, the large number of patients with IGE in the second group is explained by the high potential for provoking attacks (including alcohol) in patients with genetically determined forms of the disease. It is interesting to note that in the second group, 9 cases had a family history of epilepsy, and 5 of them were diagnosed with IGE.
In 2 patients who were not included in either the first or second groups, the relationship between seizures and alcohol consumption was considered unlikely; both were diagnosed with cryptogenic epilepsy and achieved a 50% reduction in the frequency of seizures (improvement).
The study also included a patient with the onset of attacks due to systematic use of heroin; after stopping the abuse, the frequency of attacks tended to increase, however, after the prescription of AEDs, remission was achieved (follow-up 4 years).
How is the treatment carried out?
Alcoholic epilepsy, the symptoms of which are a reaction to damage and malfunction of the brain, is a consequence of alcoholism. The occurrence of this type of psychosis is a sign that the body is working to the limit and in the near future, under the same loads, the saddest outcome will come if you do not radically change your life.
Treatment of epilepsy takes place in a hospital or at home, after calling a narcologist. Drug therapy is used for treatment In particular, the following types of drugs are used:
- Antispasmodic drugs;
- Drugs for restoring memory and brain activity;
- Sedatives and tranquilizers;
- Products for detoxification of the body;
- Vitamin cocktails to restore strength after a seizure.
Drugs are selected strictly on an individual basis, treatment occurs a course , with additional medications taken during an attack or when warning signs appear. The dosage and time of administration are also prescribed by the doctor; experimenting with them on your own is not recommended.
In combination with therapy prescribed by a specialist, it is allowed to use traditional medicine techniques, drink infusions and decoctions of herbs to calm and cleanse the body. Maintain rest and bed rest until full recovery.
Symptoms
In people with chronic alcoholism syndrome, the greatest risk of seizures occurs not during the period of active use, but at the peak of “withdrawal” - within one to two days after stopping or reducing the dose of alcohol . Symptoms of alcoholic epilepsy are varied and depend on the location and extent of the lesion in the brain cells.
- Precursors of an attack are anxiety and irritability , uttering phrases that are inappropriate for the occasion. Before the onset of the event, the skin acquires a bluish tint; during an attack, the patient falls and throws back his head. There is a strong clenching of the jaws, respiratory dysfunction, involuntary stool and urination.
- Among the characteristic signs are short-term loss of orientation and consciousness , and impaired cognitive functions.
- Mental disorders and persistent depression often occur against the background of traumatic brain injuries.
- Nonconvulsive seizures are recurrent in nature, accompanied by episodes of dysphoria, paroxysms (contractions of skeletal muscles), and motor automatisms. A typical symptom is a repetition of the attack pattern, which with a high probability can develop without connection with alcohol.
- Sudden convulsions of individual muscle groups are accompanied by short-term loss of consciousness, psychosensory and psychomotor symptoms.
The likelihood of manifesting an epileptic seizure increases as the “drinking experience” increases.” In most cases, with chronic intoxication in the post-attack period, a psychopathological syndrome with hallucinations, delusions, and impaired consciousness is observed. Subsequently, personality changes characteristic of alcohol dependence develop.
Treatment of alcoholism as a solution to the problem
Alcoholic epilepsy, the treatment and relief of which can be carried out relatively successfully both in the hospital and at home, is only a symptom of the underlying disease. The main cause of such diseases is alcohol addiction . To prevent attacks of epilepsy and other forms of psychosis from recurring again and again, you need to completely stop drinking or reduce alcohol consumption to a safe minimum.
To treat alcoholism, you need to seek professional help from a narcologist. The procedure includes both the medication part of the therapy and work with a psychologist, and often with a psychiatrist. The manifestation of epilepsy, delirium tremens and other psychoses is an extreme symptom of addiction, in which a person needs to be saved in the literal sense. To get started, you need to contact specialists who will provide assistance.
Treatment of alcoholic epilepsy
Recovery occurs only when you undergo comprehensive measures and eliminate the bad habit. In this case, it is possible to predict a positive course and cessation of uncontrolled outbreaks. Treatment of alcoholic epilepsy and its prevention is of great importance not only for the health of the whole organism, but also for the preservation of human intelligence. Unauthorized cessation of alcoholism is a difficult task that only a few can cope with. Many people cannot withstand the “dry” period, break down and begin to abuse even more than before the disease manifested itself. If you want to free yourself and prevent deterioration, even death, you need the help of specialists. The diagnosis in question can only be cured thanks to special biotherapy, a course of psychotherapy, as well as a number of rehabilitation procedures. Stages:
- Getting rid of ethanol breakdown products, prescribing drugs that inhibit the processes of excitation of brain cells, anticonvulsants, restorative drugs at the subcellular level. Thanks to this technique, normal restoration processes of neural tissue and organs are achieved. Removing the remaining alcohol will make it easier to refuse a new dose, eliminating the physiological aspect of cravings.
- A comprehensive fight against psychological factors and the main reasons for their occurrence: depression, depression, dissatisfaction and others.
- Rehabilitation activities.
There is always a chance to feel the taste of a full life again, just believe in yourself and use the services of our professionals.
Does alcoholic epilepsy recur?
It all depends on the neglect. When seizures have already become unprovoked, therapy will help reduce the risk of relapses. If convulsions appeared only while drinking alcohol, we can say that after completing our course of therapy and giving up alcohol, or using it wisely, paroxysms will no longer bother you.
Disease and the effect of alcohol on the body
Alcohol reduces the effectiveness of drugs that need to be taken to treat the disease, although it significantly increases the sedative effect. When a person abuses medications or does not take them as needed, the effect remains minimal. In many cases, epilepsy and alcohol are harmful to health. Incorrect treatment is dangerous for the patient’s life, resulting in:
- decreased effectiveness due to low concentration of the active drug in the blood;
- increased alcohol intoxication from a number of medications, which can lead to negative consequences (manifests individually);
- increased sedative effect.
Fact: 1-2 to 5-6 units of alcohol consumed per week does not affect the frequency and number of seizures in most patients with epilepsy. reason to completely stop drinking alcohol. But at any dosage there may be a negative effect with consequences if the patient does not control the dose and neglects the recommendations of doctors.
Determination of the conditional permissible dosage depends on the effect of the amount on each patient suffering from epilepsy. This is purely individual and requires a careful approach. If it was discovered during observation that alcohol is a provocateur of attacks, stopping consumption completely would be the best solution. For people who have been addicted for a long time, epilepsy after alcohol is guaranteed to bring negative consequences.
What increases the risk of having a seizure
All people who abuse alcohol have an increased risk of having an epileptic seizure.
The following factors increase risk:
· High alcohol consumption and low quality.
· Sleep deprivation.
· Low blood sugar. A jump in glucose levels can also occur due to alcohol consumption if you have diabetes or a predisposition to it .
· Stress, overwork.
· Flashing or flickering lights, such as in discos, movies or computer games, can also trigger epileptic attacks.
The following types of attacks are distinguished:
- Generalized convulsive seizures consist of sudden muscle tension and short-term cessation of breathing. Then convulsions begin, lasting from 10 seconds to 20 minutes. The attack stops on its own, after which the child falls asleep.
- Nonconvulsive generalized seizures (absences) are less pronounced. They consist of sudden freezing, the patient’s gaze becomes absent. Sometimes the child's eyelids may tremble and his eyes may close. Duration is about 5-20 seconds; in the acute period, the child does not react to external stimuli. Once finished, he can continue to do his own thing. Typically, childhood epilepsy of this type begins at the age of 5-7 years and is more common in girls. After puberty, a child may “outgrow” the disease. But you shouldn’t wait for this, since the absence form can develop into a more complex one.
- Atonic attacks are characterized by sudden loss of consciousness with muscle relaxation. They are easily confused with fainting. If seizures occur frequently, this is a serious reason to contact a neurologist and pediatric epileptologist.
- Infantile spasm is an involuntary tilt of the head or torso forward with hands pressed to the chest. Seizures can occur after waking up, especially abruptly, and are typical for children under 3 years of age. By the age of five, childhood epilepsy of this type can either go away completely or change into another form.
In addition to the types described, there are other forms. If there is something alarming about your child’s condition, you should seek advice from a pediatric epileptologist.