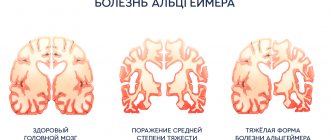
What is Parkinson's disease (PD)? This is a chronic pathology of the central nervous system with a gradually progressive course, the development of which is based on the degeneration and death of neurons that synthesize dopamine in the substantia nigra of the brain. Dopamine is known as a neurotransmitter, which in a healthy person is supplied in sufficient quantities by axonal transport to the subcortical nuclei of the brain. This process allows you to keep motor activity and muscle tone under control. In Parkinson's disease, the production of a biological substance is reduced due to neurodegeneration (destruction) of dopamine neurons, which gradually die.
As nerve cells die, dopamine synthesis becomes more and more inhibited. When the level of dead neurons reaches a critical level, the disease begins to manifest itself. A person develops serious movement disorders, which become a difficult ordeal for the patient and his family. Due to chronic degeneration of the structures of the substantia nigra of the brain, the pathological process is irreversible and permanent.
Causes of Parkinson's development
In fact, in the brain of every person, to some extent, neurons are doomed to death, which is a completely natural process for physiology. Experts have even calculated the pattern of loss of nerve cells in the brain in absolutely all people: over 10 years of life, approximately 4% of neurons die irrevocably. But the brain is unique because it can “turn on” peculiar compensatory mechanisms in order to maintain the normal functioning of the nervous system.
If the compensation potentials have dried up, and at the same time the extrapyramidal system (which includes the substantia nigra, etc.) has lost 80% of its neurons, symptoms typical of Parkinson’s disease arise. That is, in an abnormal position, the destruction of the corresponding type of neurons occurs more actively. And the older the person, the higher the likelihood of reaching the threshold level. Doctors hypothesize that the disease is associated with an increase in life expectancy, since the disease predominantly affects the elderly group.
In Parkinson's disease, a more intense decrease in the number of neurons than in normal aging physiology begins long before the onset of the main symptoms. And only decades later, when a person reaches old age, he realizes that he is sick.
Specifically, PD is classified as an idiopathic form, which indicates an independent (primary) disease that occurs for unexplained reasons. It follows that it is not associated with genetic factors or any other diseases. When examining a patient, doctors cannot determine the etiology of its development.
In medicine, there is another term - “parkinsonism”. Parkinsonism is a general concept that characterizes the syndrome as a whole, which is associated with lesions of the extrapyramidal system of primary or secondary origin. Unlike the primary form (true PD), secondary parkinsonism has an underlying cause that leads to the same clinical outcome. The root causes of secondary parkinsonism may be:
- intoxication of the body under the toxic effects of carbon monoxide, manganese, barbiturates, MPPT neurotoxin, cinnarizine, nicotine, etc.;
- chronic encephalitis;
- traumatic brain injuries;
- encephalopathy;
- cerebral atherosclerosis;
- cerebral stroke;
- brain tumors;
- heredity (family mutation of the α-synuclein and parkin genes).
Based on clinical data, in 3/4 of cases of parkinsonism syndrome, it is Parkinson’s disease that is detected, that is, the idiopathic (including juvenile) form.
Is it possible to do therapeutic massage: indications and contraindications
Manual manipulation can be carried out by inviting a specialist to your home. Massage techniques are relatively easy, so often the patient’s relatives often do it themselves.
The total time of one session should be at least an hour. The procedure begins with stroking, followed by rubbing. It helps relieve muscle stiffness, increase blood flow and reduce nervous excitability.
Next, the specialist kneads the skin and muscle groups, reducing the negative effect of the disease. This lasts for 15-20 minutes. Then the limbs are flexed and extended in all joints for 20-25 minutes.
The most popular massage method for Parkinson's disease is displacement and squeezing. The movements are performed quickly and energetically, which improves blood circulation and has a positive effect on the superficial muscle layers, subcutaneous tissue and connective tissue. The massage therapist performs them for 15-20 minutes.
For parkinsonism, the technique of tapping and striking is good. It causes contractions along the length of muscle fibers, thereby increasing overall tone. And clapping with palms in combination with chopping and striking techniques further improves the patient’s general condition.
If necessary, sessions are carried out in courses of 15-20 procedures, repeated once every two months.
How to do therapeutic massage:
Morbidity statistics
In terms of frequency of development among neurodegenerative pathologies, PD ranks second after Alzheimer's disease. According to WHO, the disease is quite widespread: in total, there are more than 6 million people in the world with such a complex diagnosis. The incidence rate in Russia corresponds to 140-160 cases per 100 thousand population. At the same time, from year to year a steady increase can be seen in the spread of pathology even among young people aged 30-40 years. According to statistics, every 10th patient is under 40 years of age. If the onset of PD occurs any year before the age of 40, it is called juvenile parkinsonism.
Based on the information provided by different authors, up to 55 years of age the morbidity risks average 0.5%, from 55-74 years old - 1.5%, 75-85 years old - 2.5-3%, over 85 years old - 4-4 ,5%. The most vulnerable group of people to the disease are men. Disability, as a rule, occurs 3-5 years after the manifestation of symptoms. The average survival rate is 15 years. Parkinson's disease is one of the diseases with relatively low mortality rates. The causes of death are mainly complications after a fall, lung infections, pulmonary embolism, and infectious pathogenesis of the urinary tract.
Signs on MRI.
In a supine position
Exercises in a lying position:
- Bringing the knees to the chest: lying on your back, bend your legs at the knee joint and pull them towards your chest, if necessary, helping with your hands, then return to the starting position.
- Bridge: bend your knees, placing your feet on the couch, and lift your pelvis, resting on your feet and shoulders, then return to the starting position
- Hip Rolls: Bend your knees, squeezing your hips together, then place your feet on the couch and tilt both knees to the right and left.
- Hip stretch: bend your right leg at the knee, keeping your left leg straight, grab the knee of your right leg with your hand and pull it to the left, then repeat the same with the other leg.
- Inner Thigh Stretch: Bend your knees with your feet flat on the couch and push your hips out, then back together.
- Bend: Bend your knees with your feet flat on the couch and lift your shoulders and head.
- Torso bending: lie on your stomach, try to rise and arch at the waist, leaning on your elbows.
- Leg curl: Lying on your stomach, bend your knee and try to touch your buttock with your heel, then repeat with the other leg.
Symptoms of Parkinson's disease: from early to late
Diagnosing Parkinson's disease at an early stage is fraught with great difficulties. Early symptoms are either absent altogether or are characterized by nonspecific manifestations that may not be perceived by people as a serious problem. Some of the first symptoms that may be associated with parkinsonism include:
- frequent or constant weakness, fatigue;
- mild coordination problems;
- slight violations of fine motor skills: for example, it is a little problematic to tie shoelaces, write with a pen;
- the appearance of painful sensations in the neck, lower back, shoulders and shoulder blades, which are often associated with osteochondrosis and arthrosis;
- depressive states, unreasonable anxiety;
- decreased olfactory sensations;
- disturbance of night sleep, but sudden falling asleep occurs during the daytime;
- problems with stool, in particular constipation.
Clinicians explain the development of such conditions, which precede obvious movement disorders, by the involvement of a significant number of nerve structures when neurodegeneration begins. The disease from the presymptomatic to the symptomatic stage occurs in several pathomorphological stages.
- First, the dorsal nuclei of the X cranial nerve and the peripheral part of the olfactory center of the telencephalon are affected.
- Then the brainstem, reticular substance, and locus coeruleus are damaged in a cascade.
- The previous two stages take approximately 2 to 4 years in total. Only then, at the third stage, does the progressive death of neurons in the substantia nigra and other structural components (amygdala, basal ganglia, hypothalamus) begin.
Further, morphological disturbances continue, and, starting from stage 4, when the dopamine deficiency is 60%-80%, clinical symptoms appear. Their spectrum is quite diverse, but the most specific manifestations of parkinsonism are:
- tremor of the distal extremities - usually begins in one arm, and as the disease progresses, it spreads to the other arm and lower extremities;
- trembling of the head and its individual organs - the head trembles in the vertical ("yes-yes" type) and/or horizontal direction ("no-no" type), in addition, tremor of the tongue, eyelids and lower jaw may be observed;
- reduction in involuntary motor activity - general stiffness, freezing in a certain position, active movements at a slow pace are resumed after some delay (bradykinesia);
- puppet gait is when a person walks in small steps with the feet placed parallel to each other, while the arms do not move in a friendly manner and are pressed to the body, the head and body remain frozen;
- facial expression - frozen (petrified) facial expressions that do not correspond to the events taking place (emotions of joy and crying appear with a delay, and subside just as slowly and with a lag);
- speech disorders – the patient’s speech becomes monotonous and inexpressive, intonation is absent or weakly expressed, and tends to fade;
- violation of writing and handwriting - due to the reduced range of movements when writing, the letters become very small, so much so that the author himself is often unable to decipher what is written;
- muscle rigidity is muscle hypertonicity, which in certain muscle groups leads to the formation of a “mannequin” pose (the back is bent and together with the head tilted forward, the arms at the elbows are bent and close to the body, and the legs at the knees and hips are fixed in a position of slight flexion );
- loss of postural reflexes - a serious impairment of coordination of movements when walking, accompanied by difficulties at the start (it is difficult to start movements) and finish (it is impossible to stop the inertia of movement) with loss of the center of gravity (occurs in the later stages, often leading to injury);
- psychosis and vegetative disorders - deviations of the mental state are expressed by hallucinatory-paranoid syndrome, attacks of fear, affect of confusion, insanity, a tendency to repeat the same questions; autonomic dysfunction is manifested by orthostatic disorders, problems with urination and defecation;
- violation of metabolism, secretory functions - often accompanied by obesity or rapid weight loss to the lower limits, excessive secretion of saliva, greasy skin, hyperhidrosis.
Exercises while sitting
- depiction of different emotions (joy, anger, surprise;
- moving, raising, lowering eyebrows;
- lip compression;
- moving the tongue out in different directions.
For the muscles of the neck and shoulder girdle
- slow turns of the head to the right and left;
- tilting the head in different directions: towards the shoulders, forward and backward;
- raising and lowering the shoulders;
- circular movements in the shoulder joints: touch your shoulders with your fingers and hold your hands in this position, then carry out circular movements with bent arms;
- shoulder extension: bend your elbows and pull them back, bringing your shoulder blades together, hold for five seconds, then relax and repeat.
- straightening your back, resting your hands on your lower back;
- bend back and forth, holding the chair seat with your hands.
For the muscles of the upper limbs:
- circular movements with palms closed into a fist, outward and inward;
- finger-picking: alternately touching the thumb with the fingers.
For the muscles of the lower extremities:
- alternately straightening the legs at the knee joints;
- circular movements of the feet clockwise and counterclockwise;
- flexion and extension of the toes.
Diagnosis and treatment of Parkinson's disease
Doctors say that if pathology is identified and treated at an early stage (at the very beginning of neuronal death), it would be possible to slow down the speed of the destructive process and prevent the threshold level. So, a person even at 100 years old would not feel signs of the disease. But the trouble is that hardly anyone will go to the doctor if there are no problems. Patients come when symptoms appear, but the neuron reserves are already a disaster, there are almost none left, which makes it impossible to achieve such a long-term plan.
In neurological practice, there is another diagnostic problem: neurologists often make mistakes in making a diagnosis, ignoring the principles of differentiation and complexity. This leads to gross miscalculations in the prescription of symptomatic treatment; the patient often receives inadequate therapy, sometimes at an unreasonably late date. Many are simply being treated for a disease that is not what it actually is. Or they recommend medications and doses that do not correspond to the stage of pathogenesis, the patient’s age, concomitant pathologies, type of profession, etc. As a result, the clinical condition reaches a critical phase, which is why neurosurgical help is often required, that is, brain surgery.
The doctor is obliged to conduct an in-depth assessment of motor, reflective, and mental disorders, then thoroughly differentiate the signs of the disease. However, this is not enough, because a similar clinic is often present in other pathologies and syndromes. For example, with hydrocephalus, brain tumors, depression, hysteria, catatonic stupor, Isaacs syndrome, essential tremor, etc. After examination, only a pathomorphological examination of the brain can finally and reliably determine whether parkinsonism occurs and which structures are simultaneously affected.
Neurosurgeon appointment: study of brain tomography data
Parkinson's disease is a lifelong pathology and cannot be completely cured. To improve the quality of life, the following medications can be prescribed to a patient separately or in combination:
- DA receptor agonists;
- amantadine agonists;
- B-type monoamine oxidase inhibitors;
- catechol-O-methyltransferase inhibitors;
- levodopa drugs.
The principle of action of drugs is aimed at correcting the disturbed biochemical balance in the basal ganglia and replenishing missing substances. As a result, while the patient takes them, the symptoms disappear or become less pronounced. After their withdrawal there is a rapid return of symptoms with a tendency to rapid progression. Medicines have a wide range of contraindications and a number of severe side effects, so they must be chosen very carefully by a good neurologist.
Recommendations
Recommendations for physical therapy for Parkinson's disease:
- try to do exercises every day;
- the volume of classes is determined by the attending physician and exercise therapy methodologist;
- conduct classes when antiparkinsonian drugs are most effective;
- during classes, wear comfortable clothes and shoes;
- divide the exercises into small parts, rest in between;
- Repeat each exercise 10 times.
In addition to the above exercises, it is important to maintain an active lifestyle, walk more (maintaining a walking rhythm will often be difficult, but you can determine the appropriate rhythm and pace of walking for yourself), talk (the speech motor muscles also need constant support), write (strengthening the muscles responsible for for fine motor skills).
Monitoring of patients who practiced physical therapy daily for Parkinson's disease showed that exercise for six months or more significantly contributed to the stabilization of motor coordination, improved balance, and significantly slowed down the progression of the pathology. Remember, the more careful you are with your exercises, the sooner you can return to full participation in everyday life, such as going to the theater or doing something you enjoy. Old age is not a time for passive relaxation, it is a time when children are adults and you can live actively, play sports, improve your health and fulfill your dreams.
Surgery for Parkinson's disease
In modern world practice, surgical methods are actively used to treat Parkinson's disease. Surgeries can significantly alleviate symptoms and contribute to a noticeable improvement in quality of life. Turning to promising neurosurgery is sometimes very advisable. They are of particular importance when the life expectancy is long and the condition is extremely unsatisfactory. We list all the indications when it is appropriate to solve the problem promptly:
- pharmacotherapy does not give the expected result, severe symptoms are not eliminated or are eliminated to a minimal extent;
- the disease progresses greatly and forces an increase in the amount, dosage, frequency of use of medications, and such changes cause acute intolerance of the body (dyskinesia of the limbs, nausea and vomiting, swelling, severe depressive and hallucinatory syndrome, etc.);
- there is a rapidly developing loss of ability to work, which is why it is impossible to do without accompaniment and help from loved ones;
- the patient’s own desire to undergo surgical treatment due to worries about losing his job, which requires constant contact and communication with people.
Surgeries for symptoms of Parkinson's disease have contraindications. Surgery may be refused if:
- elderly patient (75 years and older);
- severe dementia (surgery will worsen dementia);
- there is an oncological process in the body;
- there are lesions of the visual-sensory system with partial blindness (the risk from a standard operation is absolute loss of vision);
- have uncontrolled diabetes mellitus (gamma-knife and cyber-knife are not contraindicated for diabetics);
- It is dangerous to operate on a patient due to the high probability of cerebral hemorrhage (for example, during treatment with antithrombotic drugs with the impossibility of their temporary withdrawal, with resistant arterial hypertension, pathologies of the blood coagulation system, etc.).
In the neurosurgical arsenal for the treatment of patients diagnosed with parkinsonism/Parkinson's disease, stereotactic techniques with proven effectiveness are used, these are:
- thalamotomy;
- pallidotomy;
- deep brain stimulation;
- radiosurgery using Gamma Knife or Cyber Knife.
During surgery
The main principle of surgical treatment is based on local destruction of the subcortical nuclei of the brain, which are responsible for the appearance of trembling syndrome and muscle rigidity. Such operations significantly allow patients to adapt to the conditions of everyday life, because some are unable to even perform basic actions - bring a spoon to their mouth, sign, fasten a button.
After undergoing neurosurgical intervention, patients, and this is of paramount importance, regain the ability to independently care. Another compelling argument in favor of surgical therapy is the opportunity to switch to the lowest, non-aggressive drug doses. Surgery in many cases makes life full or as close to normal as possible for a healthy person.
Let's consider what all the surgical tactics are that save people from those malicious torments prepared for Parkinson's disease.
Thalamotomy procedure
Thalamotomy is a stereotactic technique of neurosurgery, at which point a destructive effect is exerted on individual nuclei and pathways of the thalamus. The procedure is performed under local anesthesia, the person remains conscious and in full contact with the doctor. After anesthesia, the head is secured in a stereotaxic frame. Next, a 1.5-cm hole is made in the skull, through which a probe-electrode is introduced to the thalamus under CT control. When an electric current is applied, the tip of the probe heats up to 75-80 degrees, which causes ablation (cauterization) of the nerve structures of interest. After the intervention, a sterile bandage is applied to the skull.
Destruction of the thalamic region is effective only for contralateral (unilateral) tremor. The procedure is complex, long (manipulations take up to 2 hours), and the degree of invasiveness is average. It shows good to excellent results in 90% of cases. After thalamotomy, a stable and long-lasting anti-tremor effect is achieved; in most patients it is noted immediately in the operating room. Complications do not occur very often, in 2% of patients. Postoperative disorders are mainly represented by sensory and mental disorders, unilateral paresis.
The video is in English, but very clear:
Operation pallidotomy
The essence of pallidotomy is the destruction of the medial part of the globus pallidus in order to suppress its hyperactivity. The globus pallidus is responsible for regulating muscle tone and motor abilities. When it is overactive, as is the case with parkinsonism, inadequate reproduction of movements occurs. The procedure makes it possible to suppress its pathological impulses, which provoke inhibition of the nerve cells of the thalamus and motor areas of the cerebral cortex.
This operation is similar to thalamotomy, the difference is the functional area for direct destruction. This method can be considered as a treatment for dyskinesia from taking levodopa, combined with painful muscle spasms. Improvement in such dyskinesias occurs in 90% of cases, rigidity and bradykinesia can be reduced in 80%, tremor - only in 50-55%. Of course, if the operation was carried out flawlessly. However, if the patient's leading symptom is tremor, pallidotomy is inappropriate; thalamotomy is preferable.
Surgical suture after the procedure.
During manipulations on the globus pallidus, it is extremely important to use the most gentle intraoperative destruction systems (for example, cryoprobes) for such a vulnerable area.
Due to the close location of the optic tract and the internal capsule, and individual variability in the size of the SB, palliodotomy is increasingly being abandoned in leading clinics around the world. The technique is associated with a high risk of irreversible consequences: loss of visual fields, intracerebral hemorrhages, dysarthria, etc.
Deep Brain Stimulation Method
The unique Deep Brain Stimulation technique, invented in the 80s by French specialists, has become a good alternative to thalamo- and pollidotomy. The technique involves implanting electrodes into the brain. They will provide proper control of tremors, stiffness and slowness of movement by recognizing and blocking abnormal signals from the central nervous system. This neurostimulation procedure is not suitable for patients with non-motor impairments.
The minimally invasive session is carried out in 2 stages. At the first stage, under local anesthesia, special electrodes are inserted through a tiny hole in the skull into the area of the subthalamic nucleus. Three-dimensional CT navigation is used for highly accurate and safe introduction of electrodes. The free ends of the electrodes are left under the scalp. Over the course of approximately 1 week, the implants are tested and adjusted using magnetic devices. Once the desired effect is achieved, proceed to the second stage.
In the second stage, a pulse generator is implanted under the skin, slightly below the collarbone. The ends of the electrodes are connected to an electrical pulse generator, then a cosmetic suture is applied to the area of skin incision. After the intervention is completed, a control check of the installed system is performed. At first, there may be painful symptoms at the operation site, which will gradually subside. In general, the procedure is relatively easy to tolerate and is rarely complicated by consequences. The severity of tremor is reduced, as observations show, in many cases by 85% or more.
Upon discharge, the patient is given a special magnetic remote control, which can be used to turn the main device off or on. If symptoms worsen, the doctor will change the neurostimulator settings using only external control sources. The stimulator is powered by batteries with a service life of 5 years or more, the latest models are designed for a service life of up to 10 years.
Radiosurgery using Gamma Knife, Cyber installations
Radiosurgery operations using Gamma and Cyber knives have become a huge success in the neurosurgical world. Such procedures are safe, painless and bloodless, since they are carried out without the involvement of trephination and incisions, and do not require direct contact of surgical instruments with brain tissue. The patient does not need to be hospitalized; the session takes place on an outpatient basis. In terms of therapeutic power, advanced technologies are not inferior to, and sometimes even superior to, classical operations.
Gamma Knife and CyberKnife are the “gold standard” of modern radiosurgery. With their help, in just 1 session, the lesions that cause the clinical picture of Parkinson's disease are eliminated. The techniques work on the principle of targeted exposure to a pathological area with a radioactive beam, for example, the thalamus or globus pallidus. A concentrated dose of radiation is delivered to areas that are responsible for the appearance of trembling syndrome and other disorders. Under the influence of radioactive energy, the irradiated object is destroyed and rendered harmless, and this is followed by relief for the patient.
A doctor from a nearby office will monitor the process using computer equipment. There is no need to be afraid of radiation; “smart” installations only work in an isolated field, precisely at a selected point. Therefore, they will not have a negative effect on the body and nearby brain structures. The patient just needs to lie on the installation table for 30-60 minutes. And within an hour after the therapy, he will be able to leave the medical facility and return to everyday activities the next day. The effectiveness of tremor treatment using the Gamma or Cyber Knife system is 95% or more.
Specialized clinics
In Europe, one of the leaders in the field of neurosurgical treatment and rehabilitation of patients diagnosed with Parkinson's disease is the Czech Republic. The Czech Republic has extensive experience in restoring musculoskeletal functions and the lost potential of the central nervous system not only in Parkinsonism, but also in Alzheimer's disease, epilepsy, and brain tumors. Medical care is provided according to modern neurosurgery standards.
Czech specialists exclusively use proven, effective and gentle technologies that are relevant to the present time. Clinics in the Czech Republic are world-famous institutions that are not inferior to medical institutions in Germany and Israel. And at the same time, prices for radio- and neurosurgical care for parkinsonism in the Czech Republic are many times more affordable (at least 1.5 times lower) than in these countries.
Movements while standing
Exercises in a standing position:
- Extend your arms in front of you, turn your palms towards each other, then slowly spread your arms to the sides and back to the starting position.
- Half squats: leaning on the back of a chair, slowly bend your knees, keeping your back straight.
- Lifting on your toes: leaning on the back of a chair, rise on your toes, lifting your foot off the floor.
- Stretching: leaning on the back of a chair, stretch your leg straight back, squat down, bending the other at the knee, then return to the starting position and repeat the exercise, stretching the other leg.