Causes
There are not many reasons for the development of dyscirculatory encephalopathy. The main ones are hypertension and atherosclerosis. Discirculatory encephalopathy is less often spoken of when there is a tendency to lower blood pressure. Constant changes in blood pressure and the presence of a mechanical barrier to blood flow in the form of atherosclerotic plaques create the preconditions for chronic insufficiency of blood flow to various structures of the brain. Lack of blood flow means insufficient nutrition, untimely elimination of metabolic products of brain cells, which gradually leads to disruption of various functions.
It should be said that frequent changes in pressure lead to encephalopathy most quickly, while constantly high or constantly low pressure levels will lead to encephalopathy over a longer period of time.
A synonym for discirculatory encephalopathy is chronic cerebral circulatory failure, which, in turn, means the long-term formation of persistent disorders of the brain. Thus, the presence of the disease should be discussed only if vascular diseases are reliably present for many months and even years. Otherwise, you should look for another reason for the existing violations.
What are the causes of the disease?
Discirculatory encephalopathy develops due to the pathology of the capillaries, as a result of which they cannot fully supply the brain matter with nutrients and oxygen.
This happens for the following reasons:
- Hypertension causes damage to the integrity of blood vessels. They overlap and burst, causing brain matter to absorb plasma or blood. Harmful substances can also enter when the walls of blood vessels lose elasticity.
- Hypotension . The capillaries are weakly filled with blood, it slowly flows through them.
- In atherosclerosis, cholesterol plaques clog blood vessels. Due to improper metabolism, fats accumulate on the walls, gradually the lumen decreases and is completely blocked. Under such conditions, blood does not reach all parts of the brain.
- Osteochondrosis of one of the spine sections. With this pathology, the brain receives less blood than it should due to compression by spasmed muscles and bone processes of the vertebral artery.
- Impaired blood circulation can be caused by increased blood viscosity, which causes platelets to stick together and form clots or thrombi. They block the vessel, and the part of the brain that it supplied gradually dies.
- Nicotine addiction leads to a decrease in the lumen of capillaries, this is especially pronounced in the brain. With prolonged smoking, this condition becomes irreversible.
- Pathology of blood vessels and blood reduces the speed of movement of the latter throughout the body. Such diseases include thrombophlebitis and vegetative-vascular dystonia.
- Disturbances in the functioning of blood vessels are observed with congenital anomalies (pathological development of veins and arteries, angiodysplasia).
- Hematomas formed due to injuries to the brain or spine. They put pressure on the capillaries, compress them, and impair the access of oxygen and nutrients to the nerve cells.
- Hormonal imbalance . Endocrine glands produce hormones that regulate the state of the lumens of blood vessels in the brain. With their pathology, the production of hormones is disrupted. A hormonal imbalance often causes the development of dyscirculatory encephalopathy in women during menopause.
The transition of the disease to stage 3 is facilitated by stress, emotional stress, smoking, alcoholism, and osteochondrosis of the cervical spine.
You can study what autonomic dysfunction is and how it manifests itself in our article.
Inability to coordinate movements, spinocerebellar ataxia - features of symptoms and treatment of the disorder.
Symptoms
What should you pay attention to in order to suspect the presence of dyscirculatory encephalopathy? All symptoms of the disease are quite nonspecific and usually include “ordinary” symptoms that can also occur in a healthy person. That is why patients do not seek medical help immediately, only when the severity of symptoms begins to interfere with a normal life.
According to the classification of dyscirculatory encephalopathy, several syndromes that combine the main symptoms should be distinguished. When making a diagnosis, the doctor also determines the presence of all syndromes, indicating their severity.
- Cephalgic syndrome. Includes complaints such as headaches (mainly in the occipital and temporal regions), pressure on the eyes, nausea with headaches, and tinnitus. Any discomfort associated with the head should also be included in this syndrome.
- Vestibulo-coordinating disorders. They include dizziness, throwing up when walking, a feeling of instability when changing body position, blurred vision with sudden movements.
- Astheno-neurotic syndrome. Includes mood swings, persistently low mood, tearfulness, and feelings of distress. In case of pronounced changes, it should be differentiated from more serious psychiatric diseases.
- Dissomnia syndrome, including any sleep disorders (including light sleep, “insomnia”, etc.).
- Cognitive impairment. They combine memory impairment, decreased concentration, absent-mindedness, etc. If the impairment is severe and other symptoms are absent, dementia of various etiologies (including Alzheimer's disease) should be excluded.
Symptoms of dyscirculatory encephalopathy stage II-III
After dyscirculatory encephalopathy moves to the second or third stage, the patient’s motor and cognitive impairments worsen. Namely, he is diagnosed with serious memory impairment, decreased intelligence, and difficulties in performing previously feasible intellectual actions. Doctors note that patients themselves cannot adequately assess their intellectual abilities, and also greatly overestimate their performance.
The more the disease worsens, the more difficult it is for patients to communicate with other people. They also have difficulty navigating in space. At the third stage of the disease, its symptoms become very pronounced and significantly reduce the patient’s quality of life: he has a personality disorder, impaired thinking, and deep dementia gradually develops. Over time, patients completely lose the ability to work, and also lose self-care skills.
Discirculatory encephalopathy grades 1, 2 and 3 (description)
Also, in addition to the syndromic classification, there is a gradation according to the degree of encephalopathy. So, there are three degrees. Discirculatory encephalopathy of the 1st degree means the most initial, transient changes in brain function. Discirculatory encephalopathy of the 2nd degree indicates persistent disorders, which, however, only affect the quality of life, usually not leading to a severe decrease in ability to work and self-care. Discirculatory encephalopathy of the 3rd degree means persistent gross disorders, often leading to disability of a person.
According to statistical data, the diagnosis of grade 2 dyscirculatory encephalopathy is one of the most common neurological diagnoses.
Complications of DEP grade 3
Since the patient is unable to perform certain actions and feels a decrease in performance, he experiences unreasonable mood swings. But the direct cause is damage to the subcortex of the brain, where the areas responsible for sleep, hearing and vision are located. The frontal lobes are affected. The result of all this is depression. These are not ordinary mood problems, but a mental disorder that is characterized by the “depressive triad.” This is the name of a complex of three symptoms:
- decreased mood and loss of the ability to feel joy;
- motor retardation;
- thinking disorders.
With this disease, you may notice a decrease in mood and loss of the ability to feel joy.
Attacks of aggression occur. Damage to the occipital zone is accompanied by visual disturbances. Difficulties with breathing appear, the normal voice turns into a nasal voice. Urinary incontinence is associated with a disruption in the transmission of information to organs from nerve cells. As a result, movement disorders appear.
There are more serious complications of stage 3 encephalopathy that can affect the patient’s life expectancy.
- A stroke is an acute disorder of cerebral circulation, as a result of which some areas of the brain stop working. Often a stroke leads to loss of coordination, mobility, and sensitivity. In severe cases, the patient dies, especially if medical assistance is not provided on time.
- Cardiovascular collapse is a type of heart failure that develops due to a severe drop in vascular tone. At the same time, the mass of circulating fluid decreases, so blood flow to the heart suffers. There is a drop in arterial-venous pressure, as a result of which the most important functions of the body suffer.
- Myocardial infarction is a complication of coronary heart disease, which occurs with the appearance of necrosis of the myocardial zone. It is explained by a relative or absolute lack of blood supply.
Each of these consequences can result in death. Life expectancy depends on the occurrence of these consequences and their results.
Diagnostics
Only a neurologist can diagnose the disease. To make a diagnosis, an examination of the neurological status requires the presence of revived reflexes, the presence of oral automatism reflexes, pathological reflexes, changes when performing coordination tests, and signs of disturbance of the vestibular apparatus. You should also pay attention to the presence of nystagmus, deviation of the tongue away from the midline and some other specific signs that indicate the suffering of the cerebral cortex and a decrease in its inhibitory effect on the spinal cord and reflex sphere.
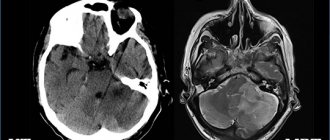
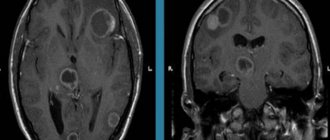
Only in addition to a neurological examination are additional research methods - REG, MRI and others. Rheoencephalography can reveal disturbances in vascular tone and asymmetry of blood flow. MRI signs of encephalopathy include the presence of calcifications (atherosclerotic plaques), hydrocephalus, and scattered vascular hypodense inclusions. Typically, MRI signs are detected in the presence of grade 2 or 3 dyscirculatory encephalopathy.
Disease severity
Depending on the clinical manifestations, it is customary to distinguish three degrees of severity of this disease:
- 1st degree. In the initial stage of the disease, subjective sensations appear. The patient notes decreased performance, mood swings, sleep disturbances, decreased memory, and increased fatigue. In most cases, there are no objective signs.
- 2nd degree . It is characterized by more obvious manifestations of the disease. Neurological disorders are noted. Upon examination, a neurologist can detect deviations from the norm in the psychological and emotional sphere.
- 3rd degree . The last stage of DEP is characterized by serious neurological changes. The patient's mental state becomes unstable, there may be attacks of aggression, and coordination is impaired. In some patients, the functions of the visual and sensory systems are impaired. Mental abnormalities, lethargy, and periodic fainting are observed.
Treatment
Treatment must be comprehensive. The main factor in successful therapy is the normalization of the causes that caused the development of the disease. It is necessary to normalize blood pressure and stabilize lipid metabolism. Standards for the treatment of dyscirculatory encephalopathy also include the use of drugs that normalize the metabolism of brain cells and vascular tone. Drugs in this group include Mexidol, Cytoflavin, Gliatilin, Sermion. The choice of other medications depends on the presence and severity of certain syndromes:
- In case of severe cephalgic syndrome and existing hydrocephalus, they resort to specific diuretics (diacarb, glycerin mixture), venotonics (detralex, phlebodia).
- Vestibular-coordinating disorders should be eliminated with drugs that normalize blood flow in the vestibular structures (cerebellum, inner ear). The most commonly used are betahistine (Betaserc, Vestibo, Tagista) and vinpocetine (Cavinton).
- Astheno-neurotic syndrome, as well as sleep disturbances, are eliminated by prescribing mild sedatives (glycine, tenoten, etc.). In case of severe manifestations, antidepressants are prescribed. You should also adhere to proper sleep hygiene, normalize the work-rest regime, and limit psycho-emotional stress.
- For cognitive impairment, nootropic drugs are used. The most commonly used drugs are piracetam, including in combination with a vascular component (fezam), as well as more modern drugs such as phenotropil, pantogam. In case of existing severe concomitant diseases, preference should be given to safe herbal-based drugs (for example, tanakan).
Treatment with folk remedies for dyscirculatory encephalopathy usually does not pay off, although it can lead to a subjective improvement in well-being. This is especially true for patients who are distrustful of taking medications. In advanced cases, such patients should be oriented to at least take constant antihypertensive therapy, and during treatment, use parenteral methods of treatment, which, in the opinion of such patients, have a better effect than tablet forms of drugs.
Cognitive impairment in dyscirculatory encephalopathy
If damage to large cerebral arteries usually leads to strokes, then the basis of the non-stroke formation of DE syndrome in most cases is microangiopathy. Its most common causes are long-term uncontrolled hypertension or diabetes mellitus. Less commonly, non-stroke vascular damage to the brain develops as a result of vasculitis, hereditary pathology (for example, with CADASIS syndrome), senile amyloid angiopathy, etc. Narrowing of small-caliber cerebral vessels leads to small-sized (lacunar) cerebral infarctions, which often form without clinical stroke. According to statistics, for every stroke there are at least 1–2 “silent” cerebral infarctions. Microhemorrhages associated with diapedetic impregnation develop no less often. They can also be asymptomatic, under the guise of a transient ischemic attack or minor stroke. Another characteristic morphological change in DE is leukoaraiosis, which is a decrease in the density of white matter. It is assumed that the formation of leukoaraiosis is based on repeated episodes of short-term local dyscirculation that do not lead to a completed infarction [4,5,23,25,29]. Due to the peculiarities of the blood supply to the brain, the favorite localization of lacunar infarctions, microhemorrhages and leukoaraiosis are the subcortical basal ganglia and deep white matter. This localization determines the peculiarities of the DE clinic, in which the most common and early symptom complex is represented by cognitive impairment (CI). Prevalence of CI in DE. CI is one of the main types of neurological disorders in DE. In 1994, a group of reputable world angioneurologists proposed the term “vascular cognitive impairment” to refer to disorders of higher brain functions due to cerebrovascular pathology. This concept unites both vascular dementia and less severe impairments of cognitive functions of vascular etiology (Table 1). It is emphasized that vascular cognitive impairment, even not reaching the severity of dementia, develops as a result of a long course of the pathological process and marks a significant cerebrovascular lesion. They indicate a significant impairment in the blood supply to the brain and should therefore be considered as an indicator of a high risk of stroke and/or vascular dementia [23,24]. In a study carried out at the Clinic of Nervous Diseases named after. AND I. Kozhevnikov, it was shown that at stages I and II of DE, cognitive impairment is present in 88% of cases. Moreover, in 56% of the examined patients, the symptoms corresponded to the generally accepted diagnostic criteria for the syndrome of mild cognitive impairment [30]. In 32% of cases, cognitive impairment was mild in severity, that is, there were individual cognitive symptoms that did not form an integral clinical syndrome [16]. Thus, cognitive impairment is detected in the vast majority of patients with DE, and already in its early stages (Fig. 1). Typically, the development of cognitive impairment preceded the formation of other objective neurological disorders, such as gait disorders, other motor pyramidal, extrapyramidal and ataxic disorders. In other words, cerebrovascular disease, including quite severe disease, can manifest itself for a long time only as cognitive disorders. Therefore, assessment of the state of the cognitive sphere should be given special attention in the diagnosis of chronic cerebrovascular insufficiency [13,14]. Clinical features of CI in DE. Damage to the deep parts of the white matter of the brain leads to separation of the anterior cortical and subcortical parts of the brain with the formation of secondary dysfunction of the frontal lobes of the brain. Neuropsychological analysis of the semiotics of cognitive and other neuropsychiatric disorders in DE indicates frontal dysfunction as the leading pathophysiological mechanism for the development of these disorders. At the same time, the basis of cognitive impairment in DE is a decrease in the activity of mental processes, difficulties in switching cognitive programs and insufficient control of current cognitive activity [2,9,11,16,22]. The earliest cognitive symptoms of DE are shown in Table 2. DE is accompanied by difficulties in all cognitive domains, but attention, intellectual operations, spatial praxis and gnosis are most affected. Memory in most cases of DE suffers secondarily due to insufficient activity and selectivity of reproduction with relative safety of memorization and storage of information. However, in some patients with DE and moderate cognitive impairment, a more pronounced memory disorder with signs of primary insufficiency in remembering incoming information is determined (Fig. 2). In such patients, neuropsychological research methods indicate the so-called “hippocampal” type of mnestic disorders: there is a significant difference between immediate and delayed reproduction, the interweaving of extraneous material, and hints during reproduction are ineffective [15]. According to our observations, the “hippocampal” type of memory impairment is an unfavorable prognostic sign for the development of dementia. Dementia in such patients is of a mixed (vascular-degenerative) nature. Thus, the specific nature of mnestic disorders may serve as an early sign of the addition of an additional degenerative process. At the stage of vascular dementia, there is a pronounced diffuse impairment of all cognitive functions, due to which the patient is deprived of independence and independence. According to morphological research methods, at the stage of dementia, the prevalence of the concomitant degenerative process can reach more than 70% of cases. It is likely that chronic cerebral vascular insufficiency is a risk factor for earlier onset and rapid progression of genetically determined forms of neurodegenerative diseases. Clinically, mixed (vascular-degenerative) dementia differs from “pure” vascular dementia by the presence of more pronounced memory impairment for current and distant life events, and less often by the presence of primary dysphasic disorders [2,6,20,26]. The relationship between cognitive and other neuropsychiatric disorders in DE. Dysfunction of the frontal lobes of the brain as a result of separation of the cortical and subcortical cerebral regions leads to the formation of not only cognitive, but also emotional and behavioral disorders. The early stages of DE are most characterized by vascular depression and emotional lability. A decrease in background mood is observed in most cases of DE; it is often mild or moderate in severity. In this case, patients rarely complain of decreased mood or depression, but usually present somatic complaints. Complaints of headache, pain in the spine, joints, in the area of internal organs, various unpleasant sensations that have no reasonable explanation taking into account the objective neurological and somatic status are very typical. Sleep disturbances such as difficulty falling asleep or early morning awakenings are common. On the contrary, eating disorders are not typical. Vascular depression is usually accompanied by emotional lability, which is understood as a rapid change in affect, often combined with increased irritability, tearfulness, touchiness over minor occasions, etc. [2,3,12,28]. It is known that emotional disorders can have an adverse effect on the cognitive sphere. However, according to our data, the severity of depression in DE does not correspond to the severity of cognitive disorders. It is likely that in DE, cognitive and emotional impairments are independent, parallel neurological disorders associated with dysfunction of the anterior parts of the brain. In this case, the increase in frontal dysfunction is accompanied by a qualitative modification of emotional disorders with regression of the depressive component (see below). At the stage of mild cognitive impairment, according to our data, there is an inverse correlation between the severity of anxiety and cognitive impairment. It is possible that activation of the hypothalamic-pituitary-adrenal axis in patients with higher levels of anxiety helps to improve concentration and the process of memorizing information [13–15]. The severity of cerebrovascular brain damage is accompanied by a qualitative modification of emotional disorders. At the same time, the severity of vascular depression decreases, and, on the contrary, signs of apathy appear and increase, motivation and initiative decrease, and indifference to oneself and others develops [12,28]. Differential diagnosis between apathy and depression can be challenging, especially in patients with severe cognitive impairment. Both with depression and with apathy, the urge to engage in any activity is significantly reduced, and patients are not busy most of the time. However, with depression, inactivity is accompanied by an unpleasant emotional experience and internal suffering of the patient - in contrast to apathy, in which patients are emotionally indifferent, and experiences are absent or of a formal nature. Apathy and decreased initiative are usually associated with vascular dementia, while depression and emotional lability are observed in patients with mild to moderate cognitive impairment. Diagnosis of CI in DE. As mentioned above, cognitive and other neuropsychiatric disorders are the most common and early sign of DE. Therefore, for timely diagnosis of cerebrovascular insufficiency, an adequate assessment of the neuropsychic sphere is necessary. The most relevant is the study of the state of the cognitive sphere in elderly patients in the presence of cognitive complaints (memory loss, increased fatigue during mental stress) and in the presence of cardiovascular diseases, such as hypertension, atherosclerosis of the cerebral arteries, diabetes mellitus, etc. For assessment the state of cognitive functions uses a neuropsychological research method. In everyday clinical practice, so-called screening psychometric scales are used, which are a set of the simplest tests for various aspects of cognitive activity: memory, attention, intelligence, praxis, gnosis, speech, orientation, etc. The generally accepted standard for screening cognitive impairment is testing for Brief Mental Status Scale (MSMS) [21]. However, it should be borne in mind that this technique was originally developed for diagnosing Alzheimer's disease. The tasks included in this technique assess the functions of the posterior parts of the cerebral cortex, such as memory, orientation, counting, speech and constructive praxis. Patients with DE, even with significant severity of cognitive impairment, can receive a high score on the KSHOPS, since with DE the anterior parts of the brain are predominantly affected. Therefore, in patients with concomitant cardiovascular diseases, it is advisable to use neuropsychological tests sensitive to frontal dysfunction. Such methods are, in particular, the clock drawing test and the battery of frontal tests by B. Dubois (Table 3 [17,28]). Mixed (vascular-degenerative) dementia is characterized by the presence of both cognitive symptoms of frontal dysfunction and involvement of the temporo-parietal parts of the brain [6]. Management of patients with DE and cognitive impairment. Treatment of vascular cognitive impairment should primarily be aimed at its cause, that is, at the underlying vascular disease causing DE. The relevance of this position is emphasized by the fact that vascular cognitive impairment is considered today as an indicator of a high risk of stroke. Therefore, establishing a diagnosis of vascular cognitive impairment should inevitably entail a comprehensive assessment of the state of the cardiovascular system and correction of modifiable risk factors for cerebral ischemia. These measures are important for the prevention of stroke, vascular and mixed dementia. The most common causes of DE are arterial hypertension, diabetic microangiopathy, atherosclerosis of the great arteries of the head and heart disease with an increased risk of thromboembolism in the brain. In the presence of arterial hypertension in patients without hemodynamically significant arterial stenosis, one should strive to achieve normotension (BP not higher than 140/90). However, control of arterial hypertension should be carried out gradually (an excessively rapid decrease in blood pressure can lead to worsening cerebral ischemia). The issue of target blood pressure values in patients with hemodynamically significant stenoses (more than 70% of the vessel lumen) of the main arteries of the head has not yet been resolved. Probably, one should not strive for complete control of arterial hypertension in these cases [1,3,22]. Atherosclerosis of the main arteries of the head is an indication for the prescription of antiplatelet agents: acetylsalicylic acid (50–150 mg per day) or clopidogrel at a dose of 75 mg per day. Dipyridomole also belongs to drugs with antiplatelet properties. Monotherapy with this drug does not have a convincing antiplatelet effect, but the addition of dipyridomole enhances the antiplatelet effect of acetylsalicylic acid [1,3]. In the presence of atrial fibrillation, valve defects, as well as a history of cardioembolic strokes, the effectiveness of antiplatelet therapy is insufficient. In these cases, the use of indirect anticoagulants is indicated to reduce the risk of repeated thromboembolism in the brain. The drug of choice is warfarin. Therapy with this drug must be carried out under regular monitoring of the international normalized ratio [1,3]. An important risk factor for cerebral ischemia is hyperlipidemia. Patients with DE should undergo regular lipid profile studies and, if hyperlipidemia is present, lipid-lowering drugs should be prescribed. Additional indications for lipid-lowering therapy are the presence of arterial stenosis, coronary heart disease and diabetes mellitus. The most promising is the use of drugs from the statin group (lovastatin, simvastatin, atorvastatin, etc.). Currently, the effectiveness of statins is assumed and actively studied not only in relation to the correction of lipid metabolism, but also the preventive effect of this class of drugs in relation to the neurodegenerative process, which often develops against the background of chronic cerebrovascular insufficiency [1,31,32]. Pathogenetically based measures are also the impact on other correctable risk factors for cerebral ischemia. Such factors include smoking, diabetes mellitus, obesity, physical inactivity, etc. [1,3]. In patients with DE, vasoactive drugs are widely used, which are expected to act primarily on the microvasculature without causing a “steal” effect. Such drugs include phosphodiesterase inhibitors (pentoxifylline, vinpocetine, gingko biloba preparations), calcium channel blockers (cinnarizine, nimodipine), alpha-blockers (nicergoline, piribedil) and some other drugs [2,3,9]. Another approach to the pathogenetic therapy of vascular cognitive impairment is to provide metabolic protection of brain neurons from ischemia and hypoxia. For this purpose, neurometabolic drugs are used that increase the survival of neurons in various pathological conditions, affecting the direct mechanisms of cerebral damage (lipid peroxidation processes, excitotoxicity, etc.). In addition to the neuroprotective effect, neurometabolic therapy also helps to optimize the reparative processes of the brain in the recovery period after acute cerebral injury. Therefore, neurometabolic therapy is used both in chronic brain failure and in the recovery period of stroke. Neurometabolic drugs include pyrrolidone derivatives (piracetam, etc.), peptidergic and amino acid drugs (Actovegin, Cerebrolysin, Cortexin, Semax), neurotransmitter precursors (choline alfoscerate) [2,3,8,9]. In domestic neurological practice, the exchange rate of vasoactive and neurometabolic drugs is traditionally accepted: 2-3 months of 1-2 year per year. Pathogenetically substantiated is also a longer intake of drugs of this group for DE (up to 6-12 months). The simultaneous administration of a vasoactive and metabolic drug is permissible and justified. Numerous studies indicate that the neurochemical basis of vascular cognitive impairment is acetylcholinergic deficiency. The reason for its occurrence in DE is the ischemic damage to the periventricular white matter, which, among other things, is acetylcholinergic axons. It should be noted that acetylcholinergic deficiency also naturally develops in the most common forms of degenerative dementia - Alzheimer's disease and dementia with Levy Taurus. Therefore, drugs with acetylcholinergic properties are indicated in the presence of cognitive disorders of both degenerative and vascular etiology and mixed (vascular -defenerative) etiology [9.18.19,22,27,28]. The central acetylcholinergic effect is possessed by the neurometabolic drug Kholin Alfoscerate. The use of this drug helps to increase the synthesis of acetylcholine and increase the activity of cerebral acetylcholinergic system. Thanks to the indicated properties of choline, alphascerates are successfully used for pathogenetic therapy of cognitive disorders with vascular pathology of the brain. Against the background of the use of this drug, there is an improvement in memorization and reproduction of information, an increase in concentration, mental performance. The drug also contributes to the regression of emotional disorders and an increase in the functional adaptation of patients with DE. In addition to the acetylcholinergic effect, Kholin alpha -athosete, being the predecessor of phosphatidylcholine, has a membrane -stabilizing effect. This pharmacological property of the drug is associated with its neuroprotective effect in conditions of ischemia and hypoxia, as well as in other pathological conditions [7,8,10]. At the stage of vascular and mixed dementia for symptomatic purposes, inhibitors of central acetylcholinerase (galantamine, rivastigmin, ipidacrine) and the reversible NMDA receptor memantine [19,27,28] are successfully used. With vascular depression, antidepressants who do not have a central cholinolytic effect are used (selective inhibitors of the reverse capture of serotonin, selective inhibitors of the reverse capture of serotonin and norepinephrine) [28]. Thus, cognitive disorders are an important component of DE syndrome. Diagnosis of vascular cognitive impairment is of great importance for the correct assessment of the neurological status, syndromic, topical and nosological diagnosis. The tactics of patients with DE and cognitive disorders should include the effect on the etiological foundations of DE, that is, on the underlying vascular disease, pathogenetic mechanisms of DE and the available symptoms. Against the background of adequate therapy, it is possible to significantly reduce the risk of developing repeated acute cerebrovascular accident and transformation of mild and moderate cognitive disorders into dementia. An important task of the doctor is also improving the quality of life of patients and their relatives.
Literature 1. Warlow C.P., M.S.Dennis, J. van Geyn et al. Stroke. Practical guide for the management of patients // Transl. from English –SPb. –1998. –P.629 2. Damulin I.V. Alzheimer's disease and vascular dementia. //Ed. N.N. Yakhno. –M. –2002. –P.85. 3. Damulin I.V., Parfenov V.A., Skoromets A.A., N.N.Yakhno. Circulatory disorders in the brain and spinal cord. //In the book: “Diseases of the nervous system. A guide for doctors." N.N.Yakhno, D.R.Shtulman (ed.). –M.: “Medicine”. –2005. –P.231–302. 4. Levin O.S., Damulin I.V. Diffuse changes in white matter (leukoaraiosis) and the problem of vascular dementia. //In the book: “Advances in neurogeriatrics.” Ed. N.N.Yakhno, I.V.Damulina. –M.: publishing house MMA. –1995. –P.189–231. 5. Martynov A.I., Shmyrev V.I., Ostroumova O.D. et al. Features of damage to the white matter of the brain in elderly patients with arterial hypertension. //Clinical medicine. –2000. –No. 6. –P.11–15. 6. Mkhitaryan E.A. Preobrazhenskaya I.S. Alzheimer's disease and cerebrovascular disorders.//Nevrol. magazine (Appendix). –2006. –No. 1. –pp.4–12. 7. Odinak M.M., Voznyuk I.A. Modern means of treating ischemic stroke. //Terra-Medica -1999. No. 2. – P.28–36. 8. Parfenov V.A. Metabolic therapy of ischemic stroke. //Russian medical journal. –2002. –T.10. No. 25. –P.21–30. 9. Preobrazhenskaya I.S., Yakhno N.N. Vascular cognitive impairment: clinical manifestations, diagnosis, treatment. // Neurological Journal. –2007. –T.12. –No. 5. –P.45–50. 10. Selezneva N.D., Kolykhalov I.V., Gerasimov N.P., Zharikov G.A. Gavrilova S.I. The use of gliatilin for the treatment of dementia of the Alzheimer's type. //Social and clinical Psychiatry. –1998. No. 4. – P.42–51. 11. Yakhno N.N., Levin O.S., Damulin I.V. Comparison of clinical and MRI data in dyscirculatory encephalopathy. Message 2: cognitive impairment. //Nevrol.zhur. –2001. –T.6, No. 3. –P.10–19. 12. Yakhno N.N., V.V. Zakharov. Cognitive and emotional-affective disorders in dyscirculatory encephalopathy. //Russian medical journal. –2002. –T.10. No. 12–13. –pp.539–542. 13. Yakhno N.N., Lokshina A.B., Zakharov V.V. Mild and moderate cognitive impairment in dyscirculatory encephalopathy. //Neurological journal. –2004. –No. 2. –P.30–35. 14. Yakhno N.N., Lokshina A.B., Zakharov V.V. Mild and moderate cognitive impairment in dyscirculatory encephalopathy. //Clinical gerontology. –2005. –T.11. –No. 9. –P.38–39. 15. Yakhno N.N., Zakharov V.V., Lokshina A.B. Syndrome of mild cognitive impairment in dyscirculatory encephalopathy. //Journal of neurol. and a psychiatrist. them. S.S. Korsakov. –2005. –T.105. –No. 2. –P.13–17. 16. Yakhno N.N. Cognitive disorders in a neurological clinic. //Neurological journal. –2006. –T.11. –Appendix No. 1. –P.4–12. 17. Dubois B., A. Slachevsky, I. Litvan, B. Pillon. The FAB: a frontal assessement battery at bedside. //Neurology. –2000. –V.55. –P.1621–1626. 18. Erkinjuntti T., Roman G., Gauthier S. et al. Emerging therapies for vascular dementia and vascular cognitive impairment. //Stroke. –2004. –Vol.35. P.1010–1017. 19. Erkinjuntti T., Roman G., Gauthier S. Treatment of vascular dementia–evidence from clinical trials with cholinesterase inhibitors. //J Neurol Sci. –2004. –Vol.226. –P.63–66. 20. Fu C, Chute DJ, Farag ES et al. Comorbidity in dementia: an autopsy study. //Arch Pathol Lab Med. –2004. –V.128. –N.1. –P.32–38. 21. Folstein MF, SEFolstein, McHugh PR Mini–Mental State: a practical guide for grading the mental state of patients for the clinician. J Psych Res, 1975, V.12, pp 189–198. 22. Golomb J., Kluger A., Garrard P., Ferris S. Clinician's manual on mild cognitive impairment // London: Science Press, 2001. 23. Hachinski VC, Lassen NA, Marshall Y. Multi-infarct dementia: a cause of mental deterioration in the elderly. //Lancet. –1974. –V.2. –P.207. 24. Hachinski V. Vascular dementia: radical re-definition. In Vascular dementia: etiology, pathogenesis and clinical aspects. //Ed. By L.A.Carlson, S.G.Gottfries, B.Winblad. –Basel ETC: S.Karger. –1994. –P.2–4. 25. Hershey LA, Olszewski WA Ischemic vascular dementia. //In: Handbook of Demented Illnesses. Ed. by JCMorris. –New York etc.: Marcel Dekker, Inc. –1994. –P.335–351 26. Korczyn AD Mixed Dementia—the Most Common Cause of Dementia / Ann. NY Acad. Sci. – 2002. – V.977. – P.129–134. 27. Kumar V., Messina J., Hartman R., Cicin–Sain A. Presence of vascular risk factors in AD patients predicts greater response to cholinesterase inhibition. //Neurobiol. Aging. –2000. –Vol.21. –N.1S. –P.S218. 28. Lovenstone S., Gauthier S. Management of dementia. //London: Martin Dunitz, 2001. 29. Pantoni L., Garcia J. Pathogenesis of leukoaraiosis. //Stroke. –1997. –V.28. –P.652–659. 30. Petersen RS, Touchon J. Consensus on mild cognitive impairment. //Research and practice in AD. EADS–ADCS joint meeting. –2005. –V.10. –P.24–32. 31. Simon M., Keller P., DeStrooper B. et al. Cholesterol depletion inhibits the generation of beta–amyloid in hippocampal neurons. //Proc Natl Acad Sci USA. –1998. –V.95. –P.6460–6464. 32. Shepherd J., Blauw G., Murphy M. et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomized placebo controlled trial. //Lancet. –2002. –V.360. –P.1623–1630.
Prevention
There are not many methods for preventing the disease, but standard treatment cannot do without prevention. To prevent the development of dyscirculatory encephalopathy, as well as to reduce its manifestations, you should constantly monitor the level of blood pressure, the content of cholesterol and its fractions. Psycho-emotional overload should also be avoided.
If you have dyscirculatory encephalopathy, you should also regularly (1-2 times a year) undergo a full course of vasoactive, neuroprotective, nootropic therapy in a day or round-the-clock hospital to prevent progression of the disease. Be healthy!