An induced coma is actually a medicated sleep. This state differs from anesthesia in the duration of stay in it.
Under the influence of barbiturates, metabolic processes in the nervous tissue slow down. 60% of oxygen and glucose entering the brain support its bioelectrical activity. 40% of oxygen and glucose ensure metabolic processes and other activities.
In a patient in a state of drug-induced sleep, the bioelectrical activity of the brain is significantly reduced, which leads to an increase in free oxygen and glucose, which are redirected to maintain cellular metabolism in the nervous tissue. This is why a person is put into an artificial coma, in order to reduce the negative effects of oxygen deficiency and avoid hypoxic damage to the brain matter.
Artificial coma - what is it?
An artificial coma is a specific state of the body, also called drug-induced sleep, into which the patient is immersed with the help of special medications. A medically induced coma is different from a typical coma and is more like the deep sleep of anesthesia.
When a patient is placed into a medically induced coma, special drugs are used to temporarily slow down the patient's vital functions. Artificial coma is used in the treatment of serious illnesses to reduce the risk of death of the patient.
When a patient is put into an artificial coma, the work of the subcortical parts of the brain is inhibited, reflexes and pain sensitivity are suppressed, the breathing and heart rate decreases, body temperature decreases and muscles relax.
The patient is put into an artificial coma by administering barbiturates, benzodiazepines, ketamine, and propofol. Subsequently, to maintain an induced coma, the patient is administered doses of drugs that support medicinal sleep.
The patient's condition is constantly monitored by specialists (blood gas composition, electrolyte levels, acid-base balance, biochemical blood parameters are monitored).
For reference. It should be noted that the procedure for introducing a patient into an induced coma and further removing it from it is an extremely complex procedure. Therefore, in practice, drug-induced coma is rarely used, only for health reasons, when the potential benefits justify the possible risks associated with the procedure.
Degrees of coma
To simplify differentiation, doctors distinguish the following degrees of coma during strokes:
- 1st degree . It is determined by lethargy or loss of consciousness with preservation of reflexes. This is mild damage to brain cells during a stroke and slight depression of the functions of the nervous system. At the same time, skin reflexes are weakened and muscle tone is increased;
- 2nd degree . It is diagnosed by the patient falling into deep sleep, lack of response to external stimuli, skin reflexes and pain;
- 3rd degree . It is caused by extensive hemorrhage and is determined by the absence of many reflexes, consciousness, and the reaction of the pupils to light;
- 4th degree . It is not comparable to life, as it is characterized by the absence of spontaneous breathing, a sharp decrease in pressure and hypothermia. All reflexes are absent. A patient in this stage of coma has virtually no chance of returning to normal life.
Artificial coma - what for?
Induction into an artificial coma is carried out in severe pathologies, when placing the patient on medication is the only way to prevent the development of irreversible changes in organs and tissues.
For reference. Artificial coma can be used to speed up the patient’s recovery after a serious illness or injury, restore damaged nerve tissue, slow down or prevent the development of necrotic processes in tissues against the background of severe hypoxia.
For example, an induced coma helps slow blood circulation and metabolic processes in brain tissue, and therefore can prevent the development of a necrotic lesion and progressive cerebral edema during a major stroke .
Putting a patient into an artificial coma is used for:
- high risk of developing cerebral edema due to trauma, heart attack, stroke, extensive cranial hematomas of non-traumatic injury, brain tumors ;
- extensive burn damage;
- severe life-threatening intoxications;
- intractable seizures and status epilepticus;
- severe alcohol withdrawal syndrome;
- acute psychosis;
- asphyxia of newborns (severe hypoxia of newborns);
- rabies (medically induced coma is used as part of the experimental treatment of rabies; putting the patient into medicated sleep helps prevent the development of severe life-threatening brain damage).
Also, artificial coma is used when performing complex long-term operations on the heart and brain, with combined severe injuries with intense pain (if the patient requires several reconstructive operations, between which there is no point in restoring his consciousness).
What is the benefit
An artificial coma after surgery can be used for restorative purposes.
Most often, coma after surgery is used in the recovery period after extensive neurosurgical operations to provide a neuroprotective effect.
Putting the patient into an induced coma can reduce the risk of severe injuries in patients with prolonged convulsions. With cerebral edema, medicated sleep allows you to slow down metabolic processes in tissues, promotes narrowing of intracranial vessels, normalizes intracranial pressure and allows you to quickly stop the progression of edema.
For reference. Medically induced coma after major surgical interventions can significantly reduce the risk of life-threatening complications and speed up the rehabilitation period.
In case of extensive strokes, putting the patient into an artificial coma helps restore damaged nerve cells, improve the functioning of the central nervous system after general resuscitation, and also prevents the development of necrosis of brain tissue.
If the patient has severe traumatic head injuries, a medically induced coma prevents the development of intracranial hemorrhage.
Introducing medicated sleep to newborns who have suffered severe intrauterine asphyxia allows normalizing metabolic processes in tissues, as well as restoring the functioning of the central nervous system.
Features of the use of artificial coma
Introducing the patient into a state of medicated sleep is carried out exclusively in the intensive care unit. The patient is under constant supervision of medical personnel.
To introduce the patient into a state of medicated sleep, the following is used:
- hypnotics used for short-term anesthesia (propofol allows you to put the patient into a state of medical sleep for several hours, and due to its short-term action it has the lowest risk of complications);
- tranquilizers benzodiazepines (diazepam preparations allow you to put the patient into medicated sleep for up to three days);
- barbiturates (provide the best neuroprotective effect for head injuries or strokes, and also help prevent the development of cerebral edema).
The patient's breathing in a state of medicated sleep is supported by ventilation. All functions of internal organs are constantly monitored using hardware and laboratory diagnostics (electrocardiogram, electroencephalogram, blood biochemistry).
For reference. With prolonged drug-induced sleep, the patient is transferred to parenteral (intravenous) nutrition. Mandatory prevention of the development of bedsores and concomitant bacterial infections is also carried out.
Use in resuscitation therapy
An artificial coma is often performed for pneumonia, when acute respiratory failure develops against the background of pneumonia. More often, such pathologies are detected in patients with complicated influenza, who quickly develop viral or bacterial pneumonia and respiratory distress syndrome (a life-threatening condition characterized by diffuse infiltration and hypoxemia - a decrease in the concentration of oxygen in the blood).
Patients are placed in the intensive care unit, where they are sedated with medication and connected to a ventilator. In some cases, patients may remain in this condition for longer than 2 weeks. Typically, the drugs used for sedation are sodium oxybutyrate and benzodiazepines, and for muscle relaxation - Pipecuronium bromide.
In the case of an ischemic stroke , the patient is placed in an induced coma if a large lesion is detected, which is associated with a high risk of progression of neurological disorders - this measure in some cases can improve the outcome of stroke. Severe traumatic brain injuries resulting from an accident, bruise, or attack are associated with acute disruption of blood flow, cerebral edema, dislocation and compression of the brain matter.
For reference. If the patient lies in a coma, cerebral edema decreases, which often leads to stabilization of brain functions; how long the patient needs to remain in this state will be determined by the attending physician. Medication-induced sleep after complex neurosurgery reduces the risk of brain damage.
Often, a comatose state develops spontaneously as a protective reaction of the body to a negative external influence - head injury, impaired cerebral blood flow, taking a large dose of alcohol or a narcotic substance, impaired respiratory and cardiac activity due to complicated, acute somatic pathology.
Your doctor will tell you how to get out of a coma in such cases. Typically, therapeutic measures are reduced to maintaining the vital functions of the body.
The patient regains consciousness on his own or enters a vegetative state (minimal consciousness). The patient can fall asleep and wake up, swallow food, blink, but does not respond to speech at all, does not speak, and does not walk independently.
The duration of the vegetative state, like the coma itself, is difficult to predict. It can last for years and even a lifetime.
Features of carrying out in childhood
Psycho-emotional reactions of patients often complicate the treatment process and negatively affect recovery. Drug sedation as an alternative to local anesthesia is indicated for some types of dental treatment. Painful manipulations, stress, and unfamiliar surroundings negatively affect the child’s psycho-emotional status.
Usually in such cases, adequate doses of hypnotics (hypnotics) or anxiolytics (tranquilizers, psychotropic drugs that eliminate anxiety) are administered. The disadvantage of sedation is that children are unable to answer important questions during sleep that the doctor may have during treatment.
For reference. Deep medicated sleep is indicated in cases where a child is connected to a ventilator. The procedure of tracheal intubation (insertion of a breathing tube into the tracheal cavity) and the lack of speech contact cause discomfort and fear in pediatric patients, which is accompanied by an increase in the concentration of cortisol, a hormone involved in the development of stress reactions.
In parallel, reactions such as increased blood pressure, increased heart rate, and tachypnea (rapid, shallow breathing) occur. In these cases, sodium thiopental or Midazolam is usually used.
What is sedation and why is it needed?
Sedation is the intravenous administration of non-narcotic hypnotics that induce shallow sleep. It is used for various types of endoscopy, for colonoscopy, but most often in the dentist’s office. When a person is dozing, light contact with him is possible: vital reflexes and body functions are preserved and the patient responds to the doctor’s requests, for example, to turn his head or “bite a piece of paper.” Sedation is accompanied by local anesthesia to numb the work area itself.
According to anesthesiologist Yuri Timonin, propofol does not cause side effects, and the substance itself has a short-term effect and is quickly eliminated from the body. The big advantage of sedation is that it allows you to increase the treatment time to 3.5–4 hours, without stress for the patient, with easy awakening and no unpleasant consequences after it. Doctors recommend this method for arterial hypertension and angina pectoris, as well as for those who are afraid of dentists to the point of losing consciousness.
How long does an induced coma last?
The duration of drug-induced sleep is different for each patient and depends on the initial severity of his condition and diagnosis. Since the likelihood of complications directly depends on the duration of the induced coma, doctors try to reduce its duration as much as possible.
In most cases, the patient is put into medicated sleep for several hours or days. Less commonly, a medically induced coma can last up to several months.
Prognosis and consequences of coma
Coma after a stroke is a dangerous condition; the prognosis of patients is disappointing and depends on the patient’s condition, the degree and timely response of doctors. It is extremely rare for older people to regain consciousness. The chances of recovery are reduced if the duration of coma exceeded 14 days. Patients with stage 1 have the most favorable prognosis, stage 2 gives questionable results, and with stage 3-4 the person does not recover from coma. If the patient manages to regain consciousness, it will take a long time to recover.
The risk of complications increases in parallel with the length of time a person remains in this condition. The patient may develop heart failure, nervous system disorders, infections, and bedsores. The result of mechanical ventilation is often:
- pneumonia;
- tracheobronchitis;
- stenosis.
Fistulas often form on the walls of the esophagus, gastrointestinal functions are disrupted, renal failure, sepsis develop, and blood circulation is impaired. Urinary retention can cause peritonitis and bladder rupture. Symptoms of heart failure and nervous system disorders often persist long after recovery from a coma. The following are considered fatal risk factors:
- recurrent stroke of any type;
- excess of more than 15 mg/l of creatine in the blood;
- complete loss of response to treatment and pain;
- existing brain damage;
- presence of twitching for more than 3 days;
- The patient's age is over 65 years.
If the patient ends up in the hospital in a timely manner, doctors will have the opportunity to stop the comatose process and reduce the severity of possible consequences.
- How many days does a coma last after a stroke and is there a chance of survival?
Coma state
During a medically induced coma, the following occurs:
- slow breathing;
- decreased heart rate;
- reduction in blood and intracranial pressure;
- muscle relaxation;
- decrease in body temperature;
- slowing down metabolic processes in tissues;
- vasoconstriction;
- decreased kidney function;
- decrease in the amount of fluid in the body;
- decrease in cerebral blood flow rate.
Another indicative manifestation of drug-induced sleep is the patient’s lack of consciousness.
For reference. Breathing during an induced coma is supported by a ventilator.
Diagnosis for coma
It should be noted that coma can cause disability and even death.
A patient in an induced coma is maximally vulnerable to the effects of any negative factors. Therefore, his condition is constantly carefully monitored by medical personnel.
To monitor the effectiveness of treatment, the quality of maintaining medicated sleep and the state of vital signs, the following is used:
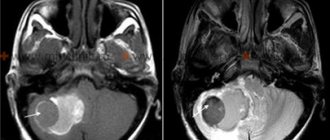
- electroencephalogram (allows you to constantly monitor the state of the patient’s cerebral cortex);
- CT and MRI to monitor the patient’s condition and make a further prognosis;
- electrocardiogram (monitoring the state of the patient’s cardiovascular system);
- cerebral angiography (allows for the most accurate assessment of the state of blood circulation in the brain);
- a ventricular catheter that allows you to measure intracranial pressure and the degree of oxygen saturation of the body;
- biochemical blood test, general blood test, assessment of blood oxygen saturation, assessment of acid-base balance and blood electrolyte levels.
For reference. Constant monitoring of the patient’s condition helps prevent the development of complications and promotes timely recovery from drug-induced sleep.
There's a long way ahead
Alla tenderly holds Mikhail’s hand and strokes his shoulder in between camera flashes.
She saw her husband in person only a week ago - after 25 days of separation. “We were both nervous, it was like a first date.” I was afraid to go into the room. At the door I collected my thoughts for about five minutes, the nurse asked: “Why are you standing there?” But I just couldn’t cross the threshold. But now we are doing well - we are slowly recovering and gaining strength. You see, we are already sitting, taking our first steps.
Now Mikhail is being treated by surgeon Vyacheslav Erokhov
. He, as is typical for a man, is unemotional and approaches the issue of therapy with a cool mind:
“We still need to work with the patient.” Mikhail shouldn’t lie still, I constantly remind him of the phrase “Movement is life”, I try to stimulate him this way. Now the patient is receiving antibacterial and antiulcer therapy, his skin is treated to prevent bedsores, he is given expectorants, blood tests and x-rays are done. He has already passed the critical stage and does not require constant medical supervision, but it is still too early to relax. Mikhail realized that he had passed the intensive care unit, and for now he thought that everything was over for him. Not really. He has a lot of work ahead of him and a long road of rehabilitation.
Surgeon Vyacheslav Erokhov
Why is an induced coma dangerous?
The most common complications of an induced coma are bedsores. In order to avoid their development, the patient’s relatives and medical personnel must periodically change the position in which the patient is, give him a gentle massage, and carefully monitor skin hygiene.
Attention. Due to muscle relaxation, lack of consciousness and impaired swallowing, an induced coma can be complicated by severe aspiration pneumonia associated with the reflux of gastric contents into the lungs.
It is also possible to develop:
- laryngeal stenosis and pulmonary edema (against the background of constant mechanical ventilation (artificial ventilation));
- acute cardiovascular failure;
- collapse;
- renal failure;
- infectious and inflammatory processes in internal organs;
- sepsis.
After the patient is brought out of a medically induced coma, there may be a temporary decrease in memory, impaired speech and motor activity, and lethargy.
The duration of the rehabilitation period in this case will depend on the duration of the induced coma and the severity of the resulting disorders.
For reference. It should be noted that during the first year after drug-induced sleep, approximately every 10 patient manages to return to normal life. In other cases, the period of complete recovery takes a longer period of time.
Types of drug coma
Depending on the drug used, there are several types of narcotic coma. To administer the necessary antidote, predict the situation and carry out relevant resuscitation measures, it is important for doctors to know which drug resulted in intoxication.
Heroin coma
Heroin coma most often occurs from an overdose of this drug. Intoxication with this drug leads to the rapid development of severe complications. To remove heroin particles from the body, effective antidotes are used - Naltrexone or Naloxone. If you suspect that a loved one is using heroin, it is better to buy an ampoule of the medicine at the pharmacy in advance, so that if necessary, you can immediately administer the drug, without causing more serious consequences.
HEROIN ADDICTION TREATMENT
Toxic coma
Low-quality drugs prepared in an artisanal way are a common cause of toxic coma. This is especially true for synthetic substances, which may contain ammonia, detergents, manganese and other life-threatening substances.
Opiate coma
When a coma occurs as a result of an overdose of opiate drugs, hardware detoxification with the help of Naloxone is most often performed. A large amount of this drug, which is an opiate antidote, is injected into the body to bind narcotic toxins and remove them from the body.
Coma after an overdose of pills
Drug overdose can occur as a result of:
- erroneously taking a potent drug in large quantities,
- intentionally taking drugs in greatly increased dosages to obtain a narcotic effect.
As a result of an overdose of tablets, there is a high probability of a drug-induced coma. Most often, intoxication occurs due to exceeding the dosage of the following drugs:
- sleeping pills,
- sedatives, painkillers,
- nootropic drugs,
- cardiac drugs.
Find out treatment recommendations without leaving home for free
To select a treatment plan, you just need to leave a request, we will contact you to select the time and specialist you need
Submit your application
How to be brought out of an induced coma
Bringing a patient out of an induced coma is an extremely complex procedure that requires special training. The administration of medications that support the patient's medicated sleep is stopped gradually.
Relatives of the patient need to understand that recovery from a coma and further rehabilitation can last many months.
The patient's consciousness is restored gradually, periods of delirium, memory impairment, speech impairment and motor activity are possible.
For reference. During rehabilitation, patients gradually learn to eat, get out of bed, and walk on their own. Restoring memory, speech and motor activity can take from several months to a year.
Forecast for recovery
The prognosis is always extremely serious. First of all, due to the fact that patients are put into an artificial coma only in the presence of severe pathologies.
The further prognosis for rehabilitation and recovery depends on the main diagnosis, the duration of the medically induced coma, the patient’s age, the presence of concomitant pathologies and complications.
Important. The longer the patient is in an induced coma, the longer the further recovery period and the lower the likelihood of full recovery.
The most optimistic prognosis is observed in patients who were put into a short-term medical coma - up to several hours. There is also a good prognosis for complete rehabilitation in patients who have been in a medical coma for up to several days.