From ancient Greek “coma” is translated as “deep sleep”. While a person is in a coma, the nervous system is depressed. This is very dangerous, because this process progresses and failure of vital organs is possible, for example, respiratory activity may stop. While in a coma, a person stops responding to external stimuli and the world around him; he may have no reflexes.
Stages of coma
Classifying coma according to the degree of its depth, we can distinguish the following types of this condition:
- Prekoma. While in this state, the person remains conscious, but there is slight confusion in actions and lack of coordination. The body functions according to the concomitant disease.
- Coma 1st degree. The body's reaction is very inhibited even to strong stimuli. It is difficult to find contact with the patient, but he can make simple movements, for example, turning over in bed. Reflexes are preserved, but are very weakly expressed.
- Coma 2nd degree. The patient is in a deep stage of sleep. Movements are possible, but they are performed spontaneously and in a chaotic manner. The patient does not feel touch, the pupils do not react to light in any way, and respiratory function is impaired.
- Coma 3rd degree. Deep state of coma. The patient does not respond to pain, the reaction of the pupils to light is completely absent, reflexes are not observed, the temperature is low. Disturbances occur in all body systems.
- Coma 4 degrees. A state from which it is no longer possible to get out. The person has no reflexes, the pupils are dilated, and the body is hypothermic. The patient cannot breathe on his own.
In this article we will take a closer look at the condition of a person in a penultimate degree coma.
First aid before the ambulance arrives
- Place the patient on his stomach, turning him slightly on his side, with his head hanging down. This will reduce the chance of suffocation.
- The patient's thermoregulation is impaired, so it is necessary to cover him with a blanket. If the incident happened on the street, then it is necessary to bring the patient indoors.
- Invite the patient to sniff cotton wool with ammonia to return the person to consciousness.
- If the person can drink, offer warm drinks: tea, water to replenish the lack of fluid in the body.
If a person is at the stage of a severe coma, then resuscitation measures may be required: artificial respiration, chest compressions.
Coma 3rd degree. Chances of survival
This is a very dangerous condition for human life, in which the body cannot practically function independently. Therefore, it is impossible to predict how long the unconscious state will last. It all depends on the body itself, on the degree of brain damage, and on the age of the person. Coming out of a coma is quite difficult; as a rule, only about 4% of people are able to overcome this barrier. Moreover, even if the person has regained consciousness, most likely he will remain disabled.
If you are in a third-degree coma and return to consciousness, the recovery process will be very long, especially after such serious complications. As a rule, people learn to speak, sit, read, and walk again. The rehabilitation period can take quite a long time: from several months to several years.
According to studies, if in the first 24 hours after the onset of a coma a person does not feel external irritants and pain, and the pupils do not react to light in any way, then such a patient will die. However, if at least one reaction is present, then the prognosis is more favorable for recovery. It is worth noting that the health of all organs and the age of the patient who has developed a 3rd degree coma play a huge role.
Challenge: just stay human
Then my conscious path to recovery began. Hospitals followed, in which I was already conscious and understood what was happening to me and where I was. I began to fight for my health and, step by step, with the help of doctors, I restored the functions of my body. There are videos of me barely walking, but these were the first, most important steps after the accident. I overstepped myself when I was studying: it was not easy, and it took months, years of effort.
I am sure that if I had not worked hard the first year, time would have been lost. If I were lazy or didn’t have the willpower, I might still be lying down or walking, but I wouldn’t be like anything. In December I was discharged in a wheelchair, and in January I began to get on my feet and move around with assistance. Everyone was shocked.
At home, massage therapist Maxim worked with me - he had golden hands, he did lymphatic drainage, developed my arm, and gave me coordination exercises. I started to slowly study myself. A healthy person will not understand why it is difficult to get out of a chair or get out of bed; this is all done automatically. And when I left the hospital, I didn’t understand how to do this. The second year the load was a little less, I relaxed more and thought: “Everything will be fine, I’ll go back to my old life.”
I have overcome the main difficulties: speech, motor functions, coordination have returned, I set goals, communicate with people, and work. There are many consequences left, but these are not serious. I walk well, but I can’t walk on a tightrope, just like I can’t walk on a curb. And I won’t be able to carry the mug without spilling. But the main thing is that I was able to start living again at 24 years old. And, having been in a coma, I now know that after death the soul does not die.
Initially, I wanted to forget all this, to abstract myself from the memories after the accident. I set myself the task of simply remaining human, and I succeeded.
For a long time, no one except my mother and father knew what happened to me. But I think I need to talk about this, because my story of recovery from the state of a vegetable to a person can inspire someone. I'll be glad about that.
Hero page on Instagram.
Chances of survival after an accident
About thirty thousand people a year die as a result of road accidents and three hundred thousand become their victims. Many of them become disabled as a result. One of the most common consequences of a road accident is traumatic brain injury, which often causes a person to fall into a coma.
If, after an accident, a person’s life requires hardware support, and the patient himself has no reflexes and does not respond to pain and other stimuli, a 3rd degree coma is diagnosed. The chances of survival after an accident that leads to this condition are negligible. The prognosis for such patients is disappointing, but there is still a chance of returning to life. It all depends on the degree of brain injury as a result of the accident.
If a stage 3 coma is diagnosed, the chances of survival depend on the following factors:
- Degree of brain injury.
- Long-term consequences of TBI.
- Fracture of the base of the skull.
- Fracture of the cranial vault.
- Fracture of the temporal bones.
- Concussion.
- Trauma to blood vessels.
- Brain swelling.
Diagnosis of coma in adults
To diagnose coma 1, 2, 3 degrees in the center of Moscow, the following methods are used.
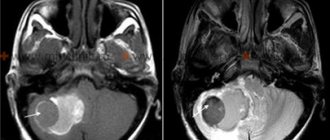
CT. One of the most informative methods of radiation diagnostics. The advantages of this procedure include the following:
- fast scanning;
- it is possible to obtain thinly sliced images (up to 0.1 cm) without increasing the radiation dose to the patient;
- increased resolution, which allows you to obtain clear images of internal organs.
MRI. A modern diagnostic method through which the doctor can obtain images of sections of soft tissues and organs in different planes.
Blood analysis. Performed to determine the concentration of hormones in the blood plasma.
Probability of survival after a stroke
A stroke is a disruption of the blood supply to the brain. It happens for two reasons. The first is blockage of blood vessels in the brain, the second is bleeding in the brain.
One of the consequences of cerebrovascular accident is coma (apoplectiform coma). In case of hemorrhage, a 3rd degree coma may occur. The chances of surviving a stroke are directly related to age and the extent of the damage. Signs of this condition:
- Lack of consciousness.
- Change in complexion (becomes purple).
- Loud breathing.
- Vomit.
- Trouble swallowing.
- Slowing heart rate.
- Increased blood pressure.
The duration of the coma depends on a number of factors:
- Coma stage. In the first or second stage, the chances of recovery are very high. With the third or fourth, the outcome is usually unfavorable.
- Condition of the body.
- Patient's age.
- Equipping with necessary equipment.
- Patient care.
Patient care
A comatose person is in intensive care, where his existence is supported by machines. Coma is a condition in which the heart continues to beat and the ability to breathe on its own is almost always maintained. Only consciousness is missing, which means that a person is unable to move, speak, hear and see, as well as cope with natural needs.
A patient in a coma needs care: feeding, hygiene, massage. Medical measures are required.
- Nutrition. Food enters the patient's stomach through a tube. To prevent dehydration, supporting vitamin drips are placed. The food itself is a mixture in powder form, similar to baby formula. It is prepared in the same way. You can also use baby fruit and vegetable purees.
- Hygiene. Every day it is necessary to wipe the body with a cloth soaked in soapy water and clean the patient’s mouth with a damp gauze cloth. You should wash your hair at least once a week. There are special care products for bedridden patients: lotions and foams for wiping the skin, napkins, caps for washing hair with shampoo.
- Massage. To prevent bedsores from forming on the body on the legs, shoulder blades and buttocks, you need to periodically turn the patient over, making light massage movements - the doctor will show them.
- Medical prescriptions for hemorrhagic stroke. If the patient has had a hemorrhagic stroke, then the possibility of recovery can only be discussed after removal of the hematoma in the brain through surgery. Neurosurgeons perform this procedure. A favorable outcome for hemorrhagic stroke is much less common than a fatal one. Subsequent treatment of a comatose patient takes place in the neurology department in the intensive care unit. If life-supporting functions are impaired, the patient is connected to a ventilator and a monitor on which all the necessary indicators are visible. They support the normal functioning of the body.
- Medical prescriptions for ischemic stroke. For ischemic stroke, the patient is prescribed anticoagulants and antiplatelet agents - Heparin, Trental, Warfarin, Acetylsalicylic acid, as well as drugs to stimulate cerebral circulation - Cereton, Actovegin, Gliatilin, Noocholin.
To protect against infections, a patient during a coma after any type of stroke is prescribed antibiotics and hepatoprotectors that restore the liver. Maintenance therapy must be supplemented with vitamins and minerals.
Signs of third degree coma during stroke
This condition has its own distinctive features:
- Lack of response to pain.
- The pupils do not respond to light stimuli.
- Lack of swallowing reflex.
- Lack of muscle tone.
- Reduced body temperature.
- Inability to breathe independently.
- Bowel movements occur uncontrollably.
- Presence of seizures.
As a rule, the prognosis for recovery from a third-degree coma is unfavorable due to the absence of vital signs.
Clinical symptoms
The main clinical sign is the patient’s absolute lack of consciousness, deprivation of mental activity and contact with the outside world. All other manifestations of the disease are associated with the causes that caused brain damage:
- Body temperature indicators. Hypothermia occurs in case of poisoning with sleeping pills, alcohol (can decrease to 32-34 C⁰). An increase in temperature to 42-43 C⁰ and dry skin accompany a coma caused by general overheating.
- Respiratory frequency. Slow, shallow breathing is a sign of an overdose of morphine-containing drugs, sleeping pills, and a decrease in the level of thyroid hormones. Deep breathing is a distinctive feature against the background of infectious intoxication due to pneumonia. This symptom occurs with kidney failure, brain tumors, uncontrolled sugar levels in diabetes in the form of acidosis.
- Pulse and blood pressure. A decrease in heart rate (bradycardia) signals coma due to heart pathologies. Frequent heartbeat - tachycardia, in combination with significant blood pressure numbers, indicate an increase in intracranial pressure. Hypertension, as a symptom, appears in patients in a coma after a stroke. Low blood pressure occurs in cases of poisoning with sleeping pills, heavy intra-abdominal bleeding, myocardial infarction, and diabetic coma.
- Skin color is also a significant diagnostic symptom. When intoxicated with carbon monoxide, the skin gradually acquires a dark red color. Suffocation is accompanied by a sharp decrease in the level of oxygen in the body’s blood, as a result of which the nail phalanges of the fingers and the nasolabial triangle turn blue. Bleeding from the ears and nose, bruises, bruises around the eyes (“a symptom of glasses”) correspond to a coma that manifested itself as a result of a traumatic brain injury. If the coma is caused by global blood loss, the skin becomes distinctly pale.
- Maintaining contact with others. A favorable encouraging sign is the ability of patients to utter some sounds. This is observed with mild coma or stupor. The more severe the patient's condition becomes, the faster the ability to make sounds is lost. The mild form is also characterized by reflex movements of the limbs in response to pain, possibly causing grimaces.
Probability of survival after neonatal coma
A child may fall into a coma in the event of a deep disorder of the central nervous system, which is accompanied by loss of consciousness. The reasons for the development of coma in a child are the following pathological conditions: renal and liver failure, meningoencephalitis, brain tumor and trauma, diabetes mellitus, water and electrolyte imbalance, cerebral hemorrhage, hypoxia during childbirth and hypovolemia.
Newborns fall into a comatose state much more easily. It is very scary when a third degree coma is diagnosed. A child has a higher chance of survival than older people. This is explained by the characteristics of the child’s body.
In the case when a 3rd degree coma occurs, the newborn has a chance of survival, but, unfortunately, it is very small. If the baby manages to get out of a serious condition, severe complications or disability are possible. At the same time, we must not forget about the percentage of children, albeit small, who managed to cope with this without any consequences.
Causes
Why do they fall into a coma? The main causes of this condition in adults:
- organic factors (stroke, gunshot wound, bruise, bleeding into the brain);
- internal chemical compounds. They are metabolic products that appear due to organ diseases;
- external chemical compounds. Poisoning of the central nervous system can occur due to an overdose of drugs, sedatives, or neurotropics.
The reasons listed above explain how people fall into a coma. Particularly worth highlighting is a factor that combines signs of organic and chemical causes. This is an increase in pressure inside the skull. A similar pathology is observed with head injuries and neoplasms in the nervous system.
Consequences of coma
The longer the unconscious state lasts, the more difficult it will be to get out of it and recover. A 3rd degree coma can occur differently for everyone. The consequences, as a rule, depend on the degree of brain damage, the length of time spent in an unconscious state, the reasons that led to the coma, the health of the organs and age. The younger the body, the higher the chances of a favorable outcome. However, doctors rarely make a prognosis for recovery, since such patients are very sick.
Despite the fact that newborns recover from a coma more easily, the consequences can be very sad. Doctors immediately warn relatives how dangerous a 3rd degree coma is. Of course, there are chances of survival, but at the same time a person may remain a “plant” and never learn to swallow, blink, sit and walk.
For an adult, a prolonged stay in a coma is fraught with the development of amnesia, the inability to move and speak, eat and defecate independently. Rehabilitation after a deep coma can take from a week to several years. In this case, recovery may never occur, and the person will remain in a vegetative state for the rest of his life, when he can only sleep and breathe independently, without reacting in any way to what is happening.
Statistics show that the chance of a full recovery is extremely small, but such events do happen. Most often, death is possible, or in case of recovery from a coma - a severe form of disability.
Movies lie
In May 2006, the journal Neurology published an article by the American doctor E. Wijdix entitled “Depiction of coma in modern feature films.”
A very unexpected topic for a serious medical journal that publishes the results of scientific research in the field of human brain activity and its diseases. It is clear that viewers do not expect complete life truth from a film, even a realistic one; film critics do not evaluate a work of art by how accurately a medical episode corresponds to the description of the disease in a textbook; what is more important is the symbolic level of the image, a certain global statement of the author. For example, in the film “Talk to Her,” the outstanding Spanish director Pedro Almodovar tells the story of a young talented ballerina who not only awakens after a many-year coma, but also almost completely recovers. At the end of the film, a girl comes to the theater to watch her favorite ballet, leaning only lightly on a cane. Dr. Wijdix harshly criticizes the film for the implausibility of such an outcome, but in fact this is the director’s deeply labored message about the great transformative power of love.
Meanwhile, Dr. Wijdix's concerns are not unfounded. Having analyzed 30 films produced between 1970 and 2004, he came to the conclusion that only in two patients in a coma are shown realistically, in the rest they are beautiful in appearance, like the heroine of the fairy tale “Sleeping Beauty,” and immediately after emerging from a coma they become cheerful and active, and even perform feats, defeating superior enemy forces (as in the American TV series “24 Hours”). Doctors in such films are depicted as caricatures and do not inspire any credibility.
But the most important thing was something else: out of 72 non-medical respondents, 28 viewers, that is, 39%, reported that when making decisions regarding loved ones who find themselves in a coma, they would rely on knowledge gleaned from watching movies. And this is a worrying sign.
It is difficult to say how representative this result is, but it can be assumed with a high probability that the “sleep of reason” is mythologized for most of us, and when we find ourselves in a severe stressful situation, if a misfortune has happened to a person close to us, we do not really know what to expect, but what to hope for and how to act.
Pre-hospital coma
CLASSIFICATION, DIAGNOSTICS
Definition
“Coma” is translated from ancient Greek as deep sleep. According to the classical definition, this term denotes the most significant degree of pathological inhibition of the central nervous system (CNS), characterized by a deep loss of consciousness, lack of reflexes to external stimuli and a disorder in the regulation of vital body functions.
However, it is more appropriate to define coma as a state of cerebral insufficiency, characterized by a violation of the coordinating activity of the central nervous system, dissociation of the body into separate, autonomously functioning systems, which at the level of the whole organism lose the ability to self-regulate and maintain homeostasis.
Clinically, coma is manifested by loss of consciousness, impairment of motor, sensory and somatic functions, including vital ones.
Main causes and pathogenesis
Comatose states develop for various reasons, which can be grouped into four groups:
- intracranial processes (vascular, inflammatory, volumetric, etc.);
- hypoxic conditions: with somatic pathology;
- in case of tissue respiration disorders (tissue hypoxia);
- when the oxygen tension in the inhaled air drops;
Classification
Depending on the causative factors, primary and secondary comas are distinguished (Table 1).
To assess the prognosis and choose treatment tactics, it is very important to determine what led to the development of a coma: focal brain damage with mass effect, damage to the brain stem, or diffuse damage to the cortex and brain stem. Moreover, the first two options are characteristic of primary ones, and the last one occurs almost exclusively in secondary comas.
Turning off consciousness - stunning - can have different depths, depending on which it is divided into:
- obnibulation - fogging, stupefaction, “cloudy consciousness”, stunning;
- doubtfulness - drowsiness;
- stupor - unconsciousness, insensibility, pathological hibernation, deep stupor;
- to whom - the most profound degree of cerebral insufficiency.
As a rule, instead of the first three options, a diagnosis of “precoma” is made. However, there are no pathogenetically substantiated distinctions between the four degrees of stunning, and therefore, regardless of the degree of loss of consciousness, it is permissible to use the term “comatose state,” the depth of which can be assessed using a simple but informative clinical scale of the depth of comatose states.
Possible complications
Among the complications of coma that are important at the prehospital stage, we can roughly highlight:
- conditions and syndromes associated directly with brain damage and swelling;
- pathological conditions and reactions caused by a violation of the regulatory function of the central nervous system.
- The first include such serious complications as:
- various breathing disorders until it stops;
- hemodynamic disorders, manifested by both arterial hyper- and hypotension, pulmonary edema, and cardiac arrest;
- central hyperthermia.
The latter, although they are “peripheral” in nature, can also be fatal:
- vomiting with aspiration of vomit into the respiratory tract and the development of asphyxia or Mendelssohn syndrome (acute respiratory failure due to broncho-obstruction, subsequent toxic pulmonary edema when acidic gastric contents enter the respiratory system);
- acute urinary retention (“neurogenic bladder”) with bladder rupture;
- ECG changes, which, unlike the “heart attack-stroke” syndrome, are in the nature of myocardial dystrophy.
Call structure "03"
According to our data obtained from analyzing the work of the Moscow Emergency Medical Service, the frequency of coma at the prehospital stage is 5.8 per 1000 calls. Quite often, the cause of coma at the prehospital stage remained not only unclear, but even unsuspected (coma of unknown origin) - 11.9%. At the same time, prehospital mortality reaches 4.4%.
Diagnostic criteria
Diagnosis of coma is based on identifying:
- varying degrees of depression of consciousness;
- reducing sensitivity to external stimuli up to its complete loss;
- specific signs of certain types of comatose states (Table 2).
Differential diagnosis is carried out with pseudocomatose states (isolation syndrome, psychogenic unresponsiveness, abulic status, non-convulsive status epilepticus).
Clinical picture
In addition to specific signs in the clinical picture of coma, a significant and sometimes leading role is played by signs of depression of consciousness and weakening of reflexes (tendon, periosteal, cutaneous and cranial nerves), progressing to complete extinction as the coma deepens. The youngest reflexes fade first, the oldest reflexes last. In the absence of focal lesions of the brain, the deepening of the coma is accompanied by the appearance and subsequent loss of bilateral pathological signs (Babinsky reflex); focal lesions are characterized by their one-sidedness. Meningeal signs - stiff neck, Kernig and Brudzinski symptoms, characteristic of damage to the meninges - meningitis, meningoencephalitis, also appear with cerebral edema and irritation of the meninges. The progression of cerebral insufficiency with loss of function leads to various respiratory disorders with hypo- or hyperventilation and corresponding respiratory changes in the acid-base state. Severe hemodynamic disturbances usually occur in a terminal state.
Questions that an emergency physician needs answers to
The list of questions and interpretation of the answers are given in table. 3.
UNDIFFERENTIATED AND DIFFERENTIATED THERAPY
Treatment of comas consists of differentiated therapy of individual comatose states and general, universal measures that do not depend on the causes, pathogenesis and clinical manifestations.
Undifferentiated therapy of comatose states
Measures to provide first aid to a patient in a comatose state have several goals, and the main measures must be carried out simultaneously:
- Mandatory immediate hospitalization in the intensive care unit, and in case of traumatic brain injury or subarachnoid hemorrhage - in the neurosurgical department.
Despite mandatory hospitalization, emergency treatment for comas should be started immediately in all cases.
- Restoring (or maintaining) an adequate state of vital functions:
- breathing: - sanitation of the airways to restore their patency, installation of an air duct or fixation of the tongue, artificial ventilation of the lungs using a mask or through an endotracheal tube, in rare cases - tracheo- or conicotomy; oxygen therapy (4-6 l/min through a nasal catheter or 60% through a mask, endotracheal tube); In all cases, tracheal intubation should be preceded by premedication with a 0.1% atropine solution in a dose of 0.5-1.0 ml (with the exception of poisoning with anticholinergic drugs);
- blood circulation: - for arterial hypertension, administration of 5-10 ml of a 25% solution of magnesium sulfate (iv bolus over 7-10 minutes or drip), bolus administration of 3-4 ml of a 1% solution (6-8 ml 0 .5% solution) of dibazole, and with a slight increase in blood pressure, a bolus injection of 5-10 ml of a 2.4% solution of aminophylline (within 3-5 minutes) is sufficient;
- the fight against arterial hypotension is carried out in three stages: - slow intravenous administration of dexamethasone at a dose of 8-20 mg or mazipredone (prednisolone) at a dose of 60-150 mg; - if ineffective - dextran 70 (polyglucin) in a dose of 50-100 ml IV in a stream, then IV drip in a volume of up to 400-500 ml; coma due to intoxication, exicosis and hemoconcentration is an indication for infusion of 1000-2000 ml of 0.9% sodium chloride solution or 5% glucose solution; - if ineffective - drip administration of dopamine at a dose of 5-15 mcg/kg/min or norepinephrine;
- for arrhythmias - restoration of adequate heart rhythm.
- Immobilize the cervical spine for any suspected injury.
- Providing the necessary conditions for treatment and control.
The requirement to comply with the “rule of three catheters” (catheterization of a peripheral vein, bladder and installation of a gastric, preferably a nasogastric, tube) when managing coma at the prehospital stage is not so categorical:
- in a comatose state, drugs are administered only parenterally and preferably intravenously; installation of a catheter in a peripheral vein is mandatory;
- Bladder catheterization should be carried out according to strict indications;
- The introduction of a gastric tube during a coma with a preserved gag reflex without preliminary intubation of the trachea and its sealing with an inflated cuff is fraught with the possible development of aspiration of gastric contents.
- Diagnosis of carbohydrate metabolism disorders and ketoacidosis:
- determination of glucose concentration in capillary blood using visual test strips; at the same time, in patients with diabetes mellitus who are accustomed to hyperglycemia due to inadequate treatment, it is necessary to take into account the possibility of developing a hypoglycemic coma even with normal glucose levels;
- determination of ketone bodies in urine using visual test strips; this manipulation is impossible in case of anuria, and when ketonuria is detected, it requires differential diagnosis of all conditions in which ketoacidosis is possible.
- Differential diagnosis and control of hypoglycemia, which is a pathogenetic link in a number of comatose conditions.
Bolus administration of a 40% glucose solution in an amount of 20.0-40.0; when the effect is achieved, but its severity is not sufficient, the dose is increased (see below).
- Prevention of a potentially fatal complication - acute Wernicke encephalopathy.
This syndrome is the result of vitamin B1 deficiency, most pronounced during alcohol intoxication and prolonged fasting and aggravated by the intake of large doses of glucose. In this regard, the administration of a 40% glucose solution in the absence of intolerance in all cases should be preceded by a bolus administration of 100 mg of thiamine (2 ml of vitamin B1 in the form of a 5% solution of thiamine chloride).
- Therapeutic and diagnostic use of antidotes:
- opiate receptor antagonist: - the diagnostic administration of naloxone should be treated with caution, since a positive reaction (albeit incomplete and short-term) is also possible with other types of coma, for example with alcoholic coma; — indications for the administration of naloxone are: respiratory rate < 10 per minute; pinpoint pupils; suspected drug intoxication; - the initial dose of naloxone (IV or endotracheal) can range from 0.4-1.2 to 2 mg with possible additional administration after 20-30 minutes if the condition worsens again; to prolong the effect, it is possible to combine IV administration with subcutaneous administration;
- benzodiazepine receptor antagonist: - in case of poisoning or suspected poisoning with benzodiazepine drugs, administration of flumazenil is indicated (0.2 mg intravenously over 15 seconds, followed by 0.1 mg every minute if necessary for a total dose of 1 mg); — the danger of using flumazenil lies in the risk of developing convulsive syndrome in mixed poisoning with benzodiazepines and tricyclic antidepressants.
- Combating intracranial hypertension, edema and swelling of the brain and meninges:
- the most effective and universal method is mechanical ventilation in hyperventilation mode, which provides the required result within an hour. However, at the prehospital stage, this method can only be used for health reasons;
- in the absence of high blood osmolarity (for example, with hyperglycemia or hyperthermia), and also if there is no threat of developing or increasing bleeding, dehydration is achieved by administering an osmotic diuretic - mannitol - in the amount of 500 ml of a 20% solution for 10-20 minutes (1-2 g/kg); to prevent a subsequent increase in intracranial pressure and an increase in cerebral edema (rebound syndrome), up to 40 mg of furosemide is administered upon completion of the mannitol infusion;
- the traditional use of glucocorticoid hormones is based on their proven effect in the case of brain tumors; Dexamethasone (8 mg) has the greatest effectiveness and safety;
- limiting the administration of hypotonic solutions, as well as 5% glucose solution and 0.9% sodium chloride solution (no more than 1 l/m2/day), which does not apply to comas occurring against the background of hemoconcentration (hyperglycemic, hyperthermic, hypocorticoid , alcoholic).
- Neuroprotection and increased wakefulness:
- when focal symptoms prevail over cerebral symptoms, piracetam is effective (drip infusion at a dose of 6-12 g);
- in case of disturbances of consciousness to the level of superficial coma, the following are indicated: - sublingual (or cheek) administration of glycine in a dose of 1 g; - intravenous administration of the antioxidant Mexidol at a dose of 200 mg (6 ml of 0.5% solution) as a bolus over 5-7 minutes;
- in case of deep coma, intranasal administration of Semax at a dose of 3 mg is performed (3 drops of a 1% solution in each nasal passage).
- Measures to stop the entry of toxin into the body in case of suspected poisoning:
- gastric lavage through a tube with the introduction of a sorbent (if poison enters through the mouth);
- washing the skin and mucous membranes with water (if poison enters through the integumentary tissue).
- Symptomatic therapy:
- normalization of body temperature: - in case of hypothermia - warming the patient without using heating pads and intravenous administration of heated solutions; - with high hyperthermia - hypothermia using physical methods and pharmacological agents (drugs from the group of analgesics-antipyretics);
- relief of seizures: - administration of diazepam (Relanium) at a dose of 10 mg;
- relief of vomiting: - administration of metoclopramide (cerucal, reglan) at a dose of 10 mg IV or IM.
- For all comas, ECG registration is mandatory.
Differentiated therapy of individual comatose states
- Hypoglycemic coma. Bolus administration of a 40% glucose solution (with preliminary administration of 100 mg of thiamine) in a dose of 20-40-60 ml, but due to the threat of cerebral edema, no more than 120 ml; if further administration is necessary, infusion of glucose in decreasing concentrations (20-10-5%) with the introduction of dexamethasone at a dose of 4-8 mg to prevent cerebral edema and as a counter-insular factor; when large doses of glucose are administered and there are no contraindications, subcutaneous administration of up to 0.5-1 ml of a 0.1% solution of adrenaline is permissible; in case of prolonged coma (more than several hours), intravenous administration of up to 2500 mg of magnesium sulfate (10 ml of 25% solution) is indicated.
- Hyperglycemic ketoacidotic and hyperosmolar non-ketoacidotic coma. Infusion of 0.9% sodium chloride solution in a volume of 1 l and 1.5 l, respectively, in the first hour. In case of hyperosmolar coma and prolonged course of ketoacidotic coma, heparin therapy is indicated - up to 10 thousand units intravenously.
- Hunger (alimentary-dystrophic) coma. Warming the patient, infusion of a 0.9% sodium chloride solution (with the addition of a 40% glucose solution at the rate of 60 ml per 500 ml of solution) at an initial rate of 200 ml per 10 minutes under the control of respiratory rate, heart rate, blood pressure and auscultation pattern lungs, fractional administration of vitamins - thiamine (100 mg), pyridoxine (100 mg), cyanocobalamin (up to 200 mcg), ascorbic acid (500 mg); hydrocortisone - 125 mg; in case of hemodynamic ineffectiveness of adequate infusion therapy and the appearance of signs of stagnation, pressor amines - dopamine, norepinephrine.
- Alcohol coma. To suppress bronchorrhea and as a premedication before tracheal intubation, a bolus injection of 0.5-1 ml of a 0.1% atropine solution. Within 4 hours after drinking alcohol, gastric lavage through a tube (after tracheal intubation) to clean rinsing water and the introduction of enterosorbent, warming, infusion of a 0.9% sodium chloride solution with an initial rate of 200 ml per 10 minutes under control of respiratory rate are indicated. Heart rate, blood pressure and auscultation picture of the lungs with a possible subsequent transition to Ringer's solution, bolus or drip administration of up to 120 ml of 40% glucose solution, fractional administration of vitamins - thiamine (100 mg), pyridoxine (100 mg), cyanocobalamin (up to 200 mcg ), ascorbic acid (500 mg); in case of hemodynamic ineffectiveness of adequate infusion therapy, pressor amines - dopamine, norepinephrine.
- Opiate coma. Administration of naloxone (see above); if tracheal intubation is necessary, premedication with 0.5-1.0 ml of 0.1% atropine solution is required.
- Cerebrovascular coma (coma due to stroke). Since at the prehospital stage of care, differential diagnosis of ischemic and hemorrhagic strokes is absolutely impossible, only undifferentiated treatment is carried out here (see above): in severe cases, to reduce capillary permeability, improve microcirculation and hemostasis - bolus administration of 250 mg of ethamsylate, to suppress proteolytic activity - drip administration of aprotinin (Gordox, Contrical, Trasylol) in a dose of 300 thousand KIU (30 thousand ATRE);
- stroke is the main indication for the use of glycine, Semax, Mexidol, and piracetam.
Activities prohibited in comatose states
In any comatose state, regardless of the depth of cerebral insufficiency, the use of drugs that depress the central nervous system (narcotic analgesics, neuroleptics, tranquilizers) is fraught with aggravation of the severity of the condition; The exception is coma with convulsive syndrome, for which diazepam is indicated.
Coma is a contraindication to the use of drugs that have a stimulating effect (psychostimulants, respiratory analeptics); the exception is the respiratory analeptic bemegride, which is indicated as a specific antidote for barbiturate poisoning.
Nootropic drugs (piracetam) are contraindicated in cases of disturbances of consciousness deeper than superficial stupor. Insulin therapy is prohibited at the prehospital stage.
Indications for hospitalization
Coma is an absolute indication for hospitalization, refusal of which is possible only if an agonal state is diagnosed.
Common errors
The most common mistakes in the prehospital stage in general and in comas in particular are related to the correction of arterial hypertension. As a rule, it is carried out by intramuscular (!) administration of magnesium sulfate, less often - dibazole, which is always combined with papaverine, which is not indicated in these cases; Dangerous clonidine and pentamine are used, often in combination with other antihypertensive drugs, which often leads to an excessive decrease in blood pressure.
The most commonly used solution for infusion therapy is isotonic sodium chloride solution, less often - a 5% glucose solution, which is to the detriment of colloidal solutions.
It is extremely rare to carry out diagnostic administration of a 40% glucose solution, which is mandatory when providing assistance to comatose patients; Moreover, in no case was the administration of concentrated glucose preceded by the administration of thiamine.
Due to the lack of opportunity, glycemia and ketonuria are not determined at the prehospital stage, and flumazenil and mexidol, which are not included in the package, are not used. Only in isolated cases is a catheter installed in a peripheral vein, which does not allow the possibility of “infusion therapy” to be taken seriously. Before tracheal intubation, premedication with atropine is not performed. Oxygen therapy is extremely rarely performed.
Doses of a number of drugs are limited and rarely exceed 0.4 mg for naloxone, and 2 g for piracetam. Moreover, the latter was administered to patients with the most severe cerebral symptoms, that is, when it is contraindicated. In the treatment of cerebral edema, furosemide is used too actively and osmotic diuretics are almost never used. Quite often, glucocorticoids are used for the treatment and prevention of cerebral edema, but preference is given to prednisolone rather than the drug of choice, dexamethasone.
Drugs that are contraindicated in comatose states are often used.
An insufficiently thorough examination of patients should be considered a significant mistake: it is impossible to conduct a full differential diagnosis, assess the severity of the condition, prognosis and determine treatment tactics without information about respiratory rate, heart rate or blood pressure. Very often the ECG is not recorded. A serious mistake, which, however, is observed too often, is the refusal to hospitalize comatose patients.
If treatment begins before the arrival of the ambulance team, then most often drugs are used that are contraindicated in patients in a coma: respiratory analeptics and psychostimulants (sulfocamphocaine, cordiamine, caffeine), clonidine, droperidol and cardiac glycosides.
A. L. Vertkin, Doctor of Medical Sciences, Professor V. V. Gorodetsky, Candidate of Medical Sciences