Coma is a borderline state between life and death. The result of inhibition of nerve impulses in the cerebral cortex, subcortex, and underlying sections. Clinically manifested by lethargy or loss of consciousness, decreased/lack of response to external stimuli, and disappearance of reflexes. Let's look at why coma develops after a stroke, what its duration is, the chances of survival and a full recovery.
Mechanism of coma development
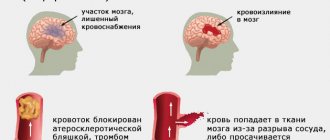
Damage to neurons is accompanied by changes in the metabolism of nervous tissue. Intracellular fluid exits into the intercellular space. As it accumulates, it compresses the capillaries, causing the nutrition of nerve cells to deteriorate even more and their work to be disrupted. A comatose state can develop very quickly (several seconds or minutes) or gradually (up to several hours, less often days). Most often, coma occurs after a massive or brainstem stroke caused by hemorrhage, less often by blockage of the cerebral arteries.
Forecast
As mentioned above, recovery from a coma is not always possible.
A certain percentage of victims emerge from a comatose state without restoration of motor and cognitive functions, i.e., they remain disabled for the rest of their lives.
The risk of death increases in the following cases:
- Over the age of 60-70 years .
- If the hemorrhage occurs in the brain stem .
- When a large area of the brain is damaged.
- If the person had bad habits (abused drinking alcohol and smoking).
In all other cases, especially at a young age, recovery from a coma is possible, but the rehabilitation process will still take some time.
Severity
There are 5 degrees of coma after a stroke of varying severity:
- Precoma – moderate confusion, stupor. The victim looks drowsy, reacts inhibited to external stimuli, or, on the contrary, is overly active.
- 1st degree – severe deafness. The patient reacts very slowly to strong external stimuli, including pain. Can perform simple actions (rolling around in bed, drinking), respond with a meaningless set of words/individual sounds, muscle tone is weak.
- 2nd degree – loss of consciousness (stupor), basic reflexes are preserved (reaction of the pupils to light, closing of the eye when touching the cornea). When approaching the patient, there is no reaction, his rare movements are chaotic. Pain reflexes are suppressed. The nature of breathing changes: it becomes intermittent, shallow, and irregular. Possible involuntary urination and bowel movements. Trembling of individual muscles and twisting of limbs are observed.
- 3rd degree – loss of consciousness, absence of pain response, some basic reflexes. Involuntary urination, defecation. Muscle tone is reduced. The pulse is palpable poorly, breathing is irregular and weak, body temperature is reduced.
- 4th degree (extraordinary) – absence of any reflexes. Agonal breathing, palpitations, ends in death.
Why is an artificial coma needed?
An artificial state is called a coma, which is achieved by administering narcotic substances (most often barbiturates) or cooling the patient’s body to a temperature of 33 degrees. They cause cerebral vasoconstriction, slowing cerebral blood flow, and reducing blood volume. Medically induced coma during stroke is necessary for some patients to eliminate cerebral edema - the most severe complication, causing more than 50% of deaths.
This technique is rarely used due to the large number of complications and unexpected results.
Duration of coma
The duration of a coma can be very different: from several hours to several days or weeks. Some patients die without regaining consciousness. Rarely does a patient remain in a coma for several months, a year, or more. But the chances of recovery after such a long coma are extremely low.
A quick exit is more likely when:
- moderate area of necrosis;
- ischemic nature of stroke;
- partial preservation of reflexes;
- young age of the patient.
Stages of medical care for patients in a coma after a stroke
Patients in a state of coma that has developed as a result of a stroke are provided with medical care at the prehospital stage by emergency physicians:
- restore airway patency;
- provide oxygen through an air duct or transfer the patient to artificial ventilation;
- prevent aspiration (foreign bodies entering the respiratory tract).
When there is a sharp decrease in blood pressure, drugs are used that have a vasopressor effect (alpha-adrenergic agonists) and improve myocardial contractility (cardiac glycosides), drugs that replenish the volume of circulating fluid (crystalloid solutions and low molecular weight dextrans). If the patient develops seizures, tranquilizers and antipsychotics are used. If necessary, barbiturates and inhalation anesthesia are used.
When a patient is admitted to the neurology clinic of the Yusupov Hospital, doctors take emergency measures:
- maintaining an optimal level of oxygen supply;
- monitoring of blood pressure and correction of cardiac activity;
- administration of pressor amines (1 ml of 1% mesotone solution intramuscularly or subcutaneously, caffeine, corticosteroids;
- constant monitoring and correction of acid-base balance in the body;
- control of swallowing (in the presence of dysphagia, a nasogastric tube is inserted to prevent aspiration bronchopneumonia and ensure adequate nutrition for the patient);
- control of the condition of the bladder and intestines.
There are currently no specific drug treatments for hemorrhagic stroke. Doctors at the Yusupov Hospital are taking measures aimed at reducing the usually high intracranial pressure. At the same time, they normalize blood pressure, the state of the blood coagulation system and the permeability of the vascular wall, and support the activity of the cardiovascular and respiratory systems. In the absence of contraindications, surgical interventions are performed at partner clinics. In the case of an ischemic stroke, patients are brought out of a coma and the restoration of lost functions is immediately begun using methods of drug therapy and physical rehabilitation.
If signs of coma appear, the patient should be placed on a horizontal surface, turn his head to the side and call an ambulance. Call and alert the clinic staff about the current situation. The Yusupov Hospital employs professors and doctors of the highest category who use modern equipment and medications that allow them to do everything possible to bring a patient out of a coma after a stroke.
Prognosis, recovery after coma
Post-stroke coma is considered the most severe type of coma (1):
- only 3% of patients manage to recover and fully recover;
- 74% of comas after a stroke end in death;
- 7% of patients manage to regain consciousness, but they lose all higher functions (the ability to think, talk, perform conscious actions, carry out commands);
- 12% of patients remain deeply disabled;
- 4% of people recover, maintaining moderate impairment.
Factors influencing the forecast:
- Localization of the focus of necrosis. If a stroke affects the medulla oblongata, where the centers for controlling breathing and heartbeat are located, death occurs very quickly.
- Duration of coma: the longer it lasts, the less hope for a full recovery, the higher the risk of death.
- Depth of coma. In medicine, the Glasgow scale is used to assess it. During the examination, the doctor tests a person’s ability to open their eyes when exposed to various stimuli, speech, and motor reactions. For each attribute a certain point is awarded (table). The lower the score, the less favorable the outcome for the patient.
| Reaction | Ball |
| Eye opening when pressed | |
| There is | 2 |
| No | 1 |
| In response to the patient's question | |
| answers inappropriately | 3 |
| makes strange sounds | 2 |
| does not react | 1 |
| When a limb is pinched forcefully | |
| withdraws | 4 |
| bends | 3 |
| unbends | 2 |
| does not react | 1 |
Coma degree (based on total points):
- 6-7 – moderate;
- 4-5 – deep;
- 0-3 – brain death.
Prognosis after ischemic, hemorrhagic
Cerebral hemorrhage usually occurs in a more severe form. The mortality rate in such patients reaches 70%; even after removal of the hematoma, the rate is not much lower. Unfavorable factors include:
- breakthrough of blood into the ventricles of the brain;
- uncontrolled arterial hypertension;
- large volume of hematoma;
- progressive cerebral edema;
- signs of displacement of the stem part;
- acute heart failure;
- increase in creatinine content in the blood;
- convulsive syndrome, lack of consciousness, reactions to painful stimuli for more than 3 days;
- age after 70 years.
With ischemic stroke, a more benign course is observed; it is rarely accompanied by a profound impairment of consciousness. This happens with repeated vascular accidents, massive blockage of the brain arteries with cholesterol plaques, lack of treatment or complete disregard of doctors’ recommendations.
Blockage of arteries in the brain
Precoma and the first degree of coma can still give the patient a chance for recovery; with a higher degree, the prognosis is considered doubtful, and the onset of extreme coma is usually regarded as fatal.
Treatment, patient care
The treatment regimen for comatose patients differs little from the management of other patients after a stroke. In the event of an ischemic stroke, the main task of the doctor is to restore the patency of the brain vessels and prevent recurrent thrombus formation. Both types of stroke require the use of diuretics that reduce brain swelling and intracranial pressure.
Patients are also prescribed medications to correct blood pressure levels and heart function. If a person cannot breathe on his own, he is connected to a ventilator.
Patients in a coma after a stroke require round-the-clock care. To prevent bedsores, patients are turned over every 2-3 hours, and pads and bolsters are placed under protruding parts of the body. Every day a person is washed, washed, diapers or urine bags are changed.
Comatose patients are fed through a feeding tube - a plastic tube that is inserted into the stomach through the nose. The patient's diet consists of various liquid dishes: pureed soups, vegetables, infant formula.
The study showed that patients who were given recordings of relatives' family stories recovered faster and better. While scrolling through the recording, memory and speech areas in their brains were activated (4).
Therefore, relatives are advised to talk with their loved ones. Be sure to introduce yourself first. Then tell the patient how your day went, remember some events that unite you. Be sure to express your love and tell him that you are looking forward to his recovery.
Coming out of a coma
The process of coming out is not like waking up. The first symptom is that the patient opens his eyes and keeps them open for some time. So far he does not respond to voice or touch. The patient's gaze is usually not focused, he looks somewhere into the distance. Chaotic movements of arms and legs are possible.
As the person improves, he begins to “wake up” from pain (for example, a pinch or touch). Movements become more purposeful. For example, the patient may try to pull out the catheter. Unfortunately, sometimes this is the maximum result that can be achieved.
Stable improvement is said to occur if a person begins to respond to being called by name and becomes able to follow simple instructions (shake a hand, move a leg). If everything goes well, the patient's condition will continue to improve. He can begin to recognize those around him, carry on a conversation, fulfill requests, and become interested in what is happening. Further recovery depends on the severity of brain damage due to stroke or coma.
Causes and pathogenesis of the disease
Advertising:
In young people, the most common causes of stroke are due to rupture or damage to vascular malformations
- congenital anomalies in the structure of arteries and veins in the brain. With prolonged existence in aneurysms, dural fistulas and various types of vascular deformations, the tone of the walls decreases, they become thinner and can rupture under the pressure of blood.
Cholesterol, which is found in many foods, has the ability to form plaques on the walls of blood vessels. They interfere with normal blood circulation. Read more in the article: “plaques in the vessels of the cervical spine.”
Another common cause of pathology is a chronic increase in blood pressure due to hypertension, kidney disease, heart disease, and pheochromocytomas. Rarer causes of cerebral hemorrhage are:
:
- deposition of amyloid protein inside the walls of blood vessels;
- atherosclerotic artery disease;
- inflammation of the wall of a cerebral vessel;
- thrombophilia and erythremia;
- overdose of blood thinning drugs.
Pathogenesis can develop in two directions. The altered vessel spontaneously ruptures with massive hemorrhage, or gradually becomes permeable with blood plasma leaking into the brain tissue.
In the presence of predisposing diseases, a hemorrhagic stroke can be triggered by stress, drinking alcohol, overheating, heavy physical work, and smoking a large number of cigarettes.