Causes of subarachnoid hemorrhage
In most cases, this condition is caused by non-traumatic factors:
- aneurysm rupture;
- rupture of a vessel in the brain against the background of arterial hypertension, atherosclerosis and other vascular diseases.
Subarachnoid hemorrhage in the brain can also be caused by traumatic factors:
- traumatic brain injury;
- brain contusion;
- fracture of the skull bones.
Main services of Dr. Zavalishin’s clinic:
- consultation with a neurosurgeon
- treatment of spinal hernia
- brain surgery
- spine surgery
Neurology Center in Moscow
Hemorrhagic stroke. Kinds:
- Parenchymal hemorrhage
- Subarachnoid hemorrhage
- Parenchymal-subarachnoid hemorrhage
- Intraventricular hemorrhage
- Stroke hematomas - non-traumatic subdural and epidural hemorrhages
Parenchymal hemorrhage
Parenchymal hemorrhage is one of the forms of acute cerebrovascular accident of the hemorrhagic type. Manifested by the appearance of focal symptoms. This is paralysis in the leg and arm, speech disorder of the dysarthria type, and blindness may suddenly develop. The nature of the symptoms depends on the location and volume of the hemorrhage.
Usually the condition is accompanied by general cerebral symptoms - headache, nausea, vomiting, depression of consciousness. These phenomena persist for more than a day.
Clinical picture of cerebral hemorrhage
Brain dysfunctions of vascular origin occur. This is the result of rupture of pathologically altered arteries of the brain. This usually occurs against a background of high blood pressure, chronic arterial hypertension, or cerebral amyloid angiopathy.
The consequence of a ruptured vessel is hemorrhage into the cranial cavity. The blood that spills out damages the brain parenchyma, and the products of its breakdown also have a toxic effect on it. This leads to swelling of the brain, compression and displacement of structures within the brain.
Diagnosis of cerebral hemorrhage
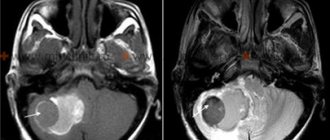
Reliable diagnostic methods are computed tomography and magnetic tomography.
If neuroimaging is not available, the diagnosis becomes less reliable.
Then it is recommended to analyze the clinical picture, spinal puncture data, and echoencephaloscopy.
Treatment methods for parenchymal hemorrhage
Carrying out basic therapy. The goals of basic therapy are to maintain normal blood pressure and eliminate cerebral edema.
Hematoma with parenchymal hemorrhage
Foci of hemorrhage range from very small to large. A large hematoma can destroy almost the entire hemisphere. Sometimes the simultaneous development of two or more lesions is possible. At various distances from the main focus, pinpoint hemorrhages can be seen. Foci of hemorrhage can be of the hematoma type and the hemorrhagic impregnation type.
Hematoma
The hematoma has a spherical shape, its edges are uneven. In the area of the hematoma there is blood that resembles a gelatinous mass; there may also be clots there. A zone of hemorrhagic infiltration is localized along the edges of the hematoma. Its width is 3-5 millimeters. This zone is followed by the zone of cerebral edema.
Brain edema provokes an increase in intracranial pressure and a disorder of venous circulation. If the hemorrhage has the form of hemorrhagic impregnation, then it does not have clear boundaries.
Symptoms of hematoma with parenchymal hemorrhage
Physical or emotional stress is a cause of hemorrhage. Usually the disease begins acutely, in the first half of the day, there are no warning signs.
It is possible to develop a comatose state - loss of consciousness, no active movements, no reaction to external stimuli, and vital functions are disrupted. When examining the patient, hemiplegia is revealed; paralyzed muscles have low tone.
If you lift a paralyzed limb, it falls like a whip. On the side of paralysis, the foot is rotated outward. Deep reflexes are not evoked. The pupils narrow or dilate and do not respond to light. On the affected side, the nasolabial fold is smoothed out, and the corner of the mouth is lowered.
Breathing with wheezing, exhalation or inhalation may be difficult. There is a slowing or increased heart rate. Pneumonia is likely to develop within 2-3 days.
Bedsores may appear in the area of the heels, buttocks, and sacrum. Severe vegetative symptoms are observed with hemorrhages in the ventricles of the brain.
When the first signs of cerebral hemorrhage occur, urgent medical attention is needed. The therapeutic department of the Neurology Center will provide highly qualified assistance in the diagnosis and treatment of cerebral hemorrhage.
Sign up for the Neurology Center:
- by phone: +7 925 191 50 55
- fill out the form: APPLICATION FOR TREATMENT
- Get advice by email [email protected]
- Clinic address: Moscow, Nagornaya st., 17 to 6
+7 (495) 506 61 01 –
REQUEST TO THE CLINIC
Clinical picture of subarachnoid hemorrhage
This condition develops rapidly against the background of a person’s normal well-being and manifests itself:
- sharp acute headache, worsening with the slightest physical activity;
- nausea, vomiting;
- convulsions;
- psycho-emotional disorders (fear, agitation, drowsiness);
- increased body temperature (up to febrile and subfebrile levels);
- disorders of consciousness (from stupor to fainting, coma);
- symptoms of damage to the oculomotor nerve (gaze paresis, drooping eyelid), hemorrhage in the eyeball.
In half of the cases, this condition leads to death. The main complications and consequences of subarachnoid hemorrhage:
- spasm of cerebral vessels caused by ischemia;
- recurrence of an aneurysm episode (may occur early or several weeks after the first episode);
- hydrocephalus (in the initial stages or in the late period);
- pathologies caused by subarachnoid hemorrhage in the brain (myocardial infarction, pulmonary edema, bleeding from a stomach or duodenal ulcer).
Among the long-term consequences of subarachnoid hemorrhage in the brain: memory disorders, attention, psycho-emotional disorders (depression, insomnia, agitation). Also, a standard complaint of patients who have suffered this condition is headache. Somewhat less frequently, hormonal disorders develop in the hypothalamic and pituitary gland systems.
Causes of hemorrhages in the ventricles of the brain
The reasons for the formation of hemorrhage in the ventricles of the brain are not fully understood and there are no specific clear reasons for this pathology.
Risk factors include the following:
- Arterial hypertension (in primary hemorrhages) is a chronic increase in blood pressure, especially dangerous in the absence of at least basic treatment.
- Uncontrolled use of antiplatelet agents, fibrinolytics.
- Vascular aneurysms are enlargements of an artery and can be congenital or acquired.
- Diabetes mellitus (with this disease the level of glucose in the blood constantly increases, which causes all kinds of complications).
- Mechanical damage to cerebral vessels (trauma).
- Hemorrhagic diathesis is increased fragility of the walls of blood vessels.
- Oncological diseases - benign and malignant tumors.
- Infectious and inflammatory processes in brain tissue (encephalitis).
There are many reasons that contribute to hemorrhage in the ventricles of the brain. They primarily affect nervous tissue. Primary factors provoke multiple complications, which leads to hemorrhages of this kind. One of the first such complications is an increase in the permeability of the walls of the vessels of the ventricular system.
Diagnosis and treatment of subarachnoid cerebral hemorrhage
The doctor clarifies the victim’s medical history and conducts an external examination. The diagnosis is established on the basis of CT data, which makes it possible to determine the extent of the process, the presence of edema, and assess the condition of the cerebrospinal fluid system. If the results are negative, a lumbar puncture is performed.
MRI is a sensitive tool for diagnosing pathology after a few days. Vascular angiography is used to determine the source of bleeding in the brain.
Therapy for subarachnoid hemorrhage takes place in a neurological hospital and depends on the severity of the patient’s condition. It is aimed at solving the following problems:
- stabilization of the patient's condition;
- prevention of recurrent episode;
- normalization of homeostasis;
- treatment and prevention of ischemia, vascular spasm;
- therapy for the disease that caused the hemorrhage.
The aneurysm is clipped or endovascular occlusion is performed. Vasospasm and ischemia are treated with medication. In case of local spasm of a vessel, a vasodilator drug is injected directly into it or balloon angioplasty is performed.
In 50% of cases, subarachnoid hemorrhage leads to death. The majority develop significant impairments in the functional activity of the brain.
You can get help with this pathology at the Department of Neurosurgery of the City Clinical Hospital named after. A.K. Eramishantseva. The clinic has modern diagnostic equipment and advanced equipment for performing complex operations.
Symptoms of hemorrhage in the ventricles of the brain
One of the very first symptoms is the rapid development of a coma. If the rush of blood into the ventricles occurs quickly, then a rapid loss of consciousness is observed. If the ventricular system is filled with blood gradually, then consciousness is not lost immediately, but after some time.
As the volume of blood in the ventricles increases and swelling occurs, the loss of consciousness becomes deeper, respiratory distress, changes in pulse, vasomotor disorders in the face, limbs and in the torso itself, and cyanosis are observed. Damage to the brain causes hemipreparalysis of gaze in the opposite direction. Jumps in body temperature may be observed - initially the temperature drops below normal, but during the day it may rise significantly (up to 40), and if blood enters the third ventricle, the temperature can reach critical levels - 42 degrees.
Laboratory tests show an increase in leukocytes in the blood, sometimes protein and sugar are present.
Early contracture can also be considered a sign of hemorrhage in the ventricles of the brain. Periodic tonic spasms are observed, occurring spontaneously or during respiratory movements. Tonic spasm is a condition during which the head is thrown back, the legs are convulsively extended, and the arms are bent and clenched in the fingers.
If hemorrhage occurs in the lateral ventricles, then the following clinical picture is observed:
- the comatose state develops rapidly;
- vomit;
- the frequency and rhythm of breathing is disrupted;
- change in heart rate - first it slows down and then increases;
- facial hyperemia;
- profuse sweating;
- severe increase in body temperature;
- pendulum-like movements of the eyeballs when the body is in a horizontal position;
- tonic convulsions during breathing;
- increased tendon reflexes and at the same time decreased skin reflexes.
Hemorrhages into the ventricle most often lead to rapid death, since the spilled blood affects vital centers.
Treatment and prevention of hemorrhage in the ventricles of the brain
Even if this type of pathology is suspected, the patient requires urgent hospitalization and the necessary standard therapy - stabilization of respiratory function, blood pressure, normalization of body temperature, administration of anticonvulsants, and, if necessary, drugs to eliminate cerebral edema. Therapy is aimed at stopping bleeding.
Surgical treatment is carried out on a strictly individual basis, taking into account the patient’s condition and all contraindications. Surgical intervention after the onset of a coma is advisable only in the first 10-12 hours.
Prevention of hemorrhage into the ventricles of the brain includes, first of all, timely treatment of arterial hypertension, responsible use of medications, and treatment of blood clotting diseases.
Differential diagnosis of subarachnoid hemorrhage
Carry out with a number of diseases of the nervous system:
- cerebral venous thrombosis,
- disorders of spinal circulation,
- cervical osteochondrosis with cervicalgia syndrome,
- migraine,
- syncope, epilepsy,
- tumors of the central nervous system (xanthochromia in the cerebrospinal fluid),
- sinusitis.
- meningoencephalitis (bullous rash with SAH).
ECG changes in the form of a wide and deep negative T wave may require the exclusion of acute myocardial infarction.
A similar electrocardiographic picture is associated with the release of catecholamines, which affects the state of coronary blood flow. Most often, focal changes on the ECG with subarachnoid hemorrhage are observed over the age of 50-55 years.