Rehabilitation of cerebral palsy is carried out for all sick children; such a program will help return the child to a full life. It is carried out under the supervision of a doctor, the doctor assesses the degree of brain damage and selects the most effective methods. It will not be possible to get rid of the disease completely, but if you do all the exercises and training, you can regain lost functions: motor activity, speech and correct the psychological status. The most effective results are observed if rehabilitation of cerebral palsy is carried out in specialized centers.
It is better to start recovery in the early years, because at a young age a child’s brain is formed and actively developing. With this approach, it is possible to effectively compensate for the main disorders that arose during intrauterine development.
Forms of the disease
Cerebral palsy does not progress, because organic brain damage occurs during pregnancy. But in the absence of rehabilitation, these complications become permanent, and a person has to live with them all his life. The main signs of cerebral palsy are movement disorders, weakening of muscle tone, the appearance of pathological reflexes, and speech impairment. All these disorders can be significantly compensated for if a rehabilitation program is started in time.
Before starting treatment, the doctor determines the form of the disease:
- spastic diplegia - damage to the muscles of the back, legs and arms, rigidity of the lower extremities is more pronounced;
- double hemiplegia – the muscles of the arms are most affected, and mental retardation is observed;
- atonic-astatic type of pathology - deterioration of muscle tone throughout the body due to damage to the cerebellum and its pathways;
- hemiparetic form - unilateral lesion with predominant weakening of the upper extremities.
How is the rehabilitation of cerebral palsy carried out? – the first two forms are more amenable to correction than others, but with constant treatment and training, even with the most severe course of paralysis, good results can be achieved.
Types and severity of cerebral palsy
The exact diagnosis, form and severity of cerebral palsy is determined by a neurologist. If the child does not need constant medical intervention and additional monitoring, then up to 6 years of age a mandatory examination is carried out 2 times a year, after 6 years - once a year and as necessary. For this purpose, standardized scales are used to assess the physical condition, musculoskeletal system, neurological status, functional, motor, and communication abilities of the child.
The GMFCS motor dysfunction scale is widely used in diagnostics. On its basis, an assessment of the patient’s physical abilities is built - for example, when determining a rehabilitation program. According to the GMFCS scale, cerebral palsy is divided into several levels:
- Level 1 - the child moves independently, but has difficulty with more complex motor skills.
- Level 2 - the child moves independently, but with limitations.
- Level 3 - the patient uses additional devices (stick, walker) and moves on a flat surface.
- Level 4 - the child can sit on his own, but not walk. Moves in an active wheelchair, or the patient is carried.
The doctor also evaluates how easily and effectively the patient exchanges information with family members and strangers, because rehabilitation and habilitation of cerebral palsy includes not only physical abilities, but also communication and socialization.
Recovery stages
The first steps in the treatment of cerebral palsy are the most difficult - the child has lesions in the cerebral structures, which cause motor impairments. In the future, it will be easier to cope with pathology; as neural connections are restored and formed, it will be easier for the nervous system to adapt to new conditions.
There are several stages of recovery; such rehabilitation is carried out for cerebral palsy from an early age. It includes:
- preparing the nervous system for upcoming loads and movements;
- biomechanical effects to destroy neural connections and restore muscle tone;
- consolidation of the results obtained, stabilization of coordination of movements and self-care.
The second stage is the most difficult; many difficulties arise during this period. A complete restructuring of the nervous system is coming - the child will actually have to learn to walk again, talk normally and deal with stress.
Comprehensive rehabilitation program for cerebral palsy in children and adults
The course is based on tools that will help correct the impairments caused by cerebral palsy and strengthen the patient’s socialization skills, ability to learn and self-care. A large role in this is played by therapeutic exercises, hydrokinesitherapy, kinesiotherapy, as well as staying in the sensory room.
Our rehabilitation center has extensive experience in working with cerebral palsy. This helps to develop effective recovery programs taking into account the individual characteristics of each patient.
The course includes:
- Individual kinesiotherapy - 20 procedures;
- Individual mechanotherapy – 20 procedures;
- Individual hydrokinesitherapy – 8 procedures;
- Classic massage - 10 procedures;
- Physiotherapy - 20 procedures;
- Balance training - 10 procedures;
- Speech therapist - 8 lessons;
- Neuropsychologist - 4 sessions;
- Ergotherapy - 6 procedures;
- Social adaptation - 14 procedures.
To create an optimal course of recovery, each patient undergoes diagnostics, which helps determine the degree of development of the disease, the specificity and complexity of the disorders.
Examination by medical specialists:
- neurologist;
- therapist;
- physiotherapist;
- physical therapy doctor;
- urologist;
- psychologist.
During the diagnostic process the following is carried out:
- clinical blood test studies;
- general blood and urine analysis;
- analysis for the presence of infections;
- ECG;
- chest x-ray;
- x-ray of joints and bones;
- Ultrasound of the kidneys, ureters, bladder, abdominal and pelvic organs.
After completing a course of recovery and adaptation, patients with cerebral palsy use in real life the practical skills of self-care, work and everyday life acquired in our center. They cope with physical and mental tasks more confidently, become more socially active, and cope more easily with difficulties caused by a neurological disease. In reviews of the treatment and rehabilitation of cerebral palsy, our patients and their relatives regularly thank us for our professional work.
Recovery methods
Rehabilitation methods for children with cerebral palsy are varied, they include ongoing treatment, physical therapy and training. Medicines are used as basic therapy, exercises and procedures help develop new skills and consolidate the results. To obtain a pronounced effect, the impact must be complex and targeted, therefore, to prescribe a program, you should contact specialized centers. A doctor in such an institution will be able to observe the patient and, if necessary, adjust rehabilitation.
Causes of cerebral palsy
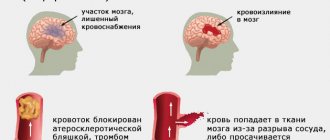
Cerebral palsy occurs after damage to one or more areas of the brain. This disorder occurs during fetal development or in infancy. The causes of the pathology can be considered:
- Injuries, asphyxia during childbirth.
- Infections in the newborn.
- Traumatic brain injuries in infancy.
- Violation of intrauterine development.
- Brain hemorrhages, hypoxia.
- Various complications during pregnancy, especially those resulting in premature birth.
Rehabilitation of children with cerebral palsy can improve the patient's condition. Cerebral palsy is not a hereditary disease and is not passed on from relatives
. Negative manifestations of pathology are aggravated throughout a person’s life in the absence of high-quality regular rehabilitation.
Hydrotherapy
This method is used in the process of pediatric rehabilitation to improve motor abilities and sensory activity. The rehabilitation room has a swimming pool with different depths, it is equipped with parallel bars and other auxiliary elements for therapeutic exercises. All classes are held individually: the therapist works with the child and at the same time teaches one of the parents. This helps improve the child-parent relationship, increase confidence levels and develop new motor abilities.
Classes are held for the purpose of:
- walking training;
- reducing spasticity;
- strengthening and development of muscles and joints.
Cerebral palsy. Part two. Principles of rehabilitation
Authors : Anna Ostroverkhova
(Continued. Read the beginning of the publication about cerebral palsy here.)
It must be said that ideas about the rehabilitation of children with cerebral palsy in the post-Soviet space and in developed countries differ.
We generally believe that treatment for cerebral palsy consists of eliminating the damage that led to the disease. If the cause of cerebral palsy lies in damage to brain tissue, then it is imperative to “help” the brain, trying to “patch” the lesion, prescribing medications containing extracts of the brains of pigs and cows, be sure to “improve” blood circulation and flavor the brain cells with vitamins. Well, physical methods of rehabilitation consist only of improving/developing impaired motor function, and include the appointment of a massage to relieve muscle tone, passive gymnastics, and older children do exercise therapy with an instructor.
Rehabilitation of children under one year old looks something like this: first, the massage therapist actively massages tense muscles (as a rule, this brings pain and discomfort to the child, which makes him scream and strain even more), and then does gymnastics with the child, passively bending/extending his limbs, doing exercises in which the child has a “led” role, i.e. movements are imposed by adults, and do not come from the child. It turns out that the child becomes an object on which various actions are performed.
At the same time, an insane amount of parental effort, time, emotional strength and material costs are spent on such actions.
But if we compare the condition after rehabilitation of our children with cerebral palsy and children with the same initial data in Europe, America or Australia, then, frankly, a suspicion creeps in: it looks like we are doing something wrong. Our model turns out to be less efficient.
The modern rehabilitation model is based on other principles:
- We accept the fact that the area of the brain responsible for certain movements is damaged and, most likely, there is nothing in its place (a cyst with cerebrospinal fluid, for example). We are not trying to "resurrect" these cells by introducing animal brain cells into an anatomical area located at the completely opposite end of the body to improve blood circulation in areas that physically do not exist. We also accept the fact that the cells that remain alive are absolutely functional and there is no need to improve anything in them either, because they were not damaged and remained normal. And these are not just philosophical arguments and conclusions. These are the results of studies that have not proven the effectiveness (and also safety) of nootropics and others like them. NO ONE IN DEVELOPED COUNTRIES USE NOOTROPS FOR TREATING ANYTHING.
- We recognize the fact that man is a rather lazy creature, which means he will not try to do something for which he is not motivated. You can passively perform some kind of manipulation with a child for as long as you like, but if he is not motivated to perform the movement or it is performed with great protest on the part of the child, then after completing the rehabilitation course this skill is unlikely to be consolidated.
Therefore, we definitely motivate the child to perform the movement (for example, the massage therapist not only skillfully turns the child from his back to his stomach, controlling his legs, but a bright toy is placed next to the child, which he tries to reach, i.e. motivation is created, and already in during the process, an adult can show the child how to perform the movement correctly).
In other words, the child must understand what he is doing and why. And for the purposes of the rehabilitation course, it will not be “decrease in tone in the upper extremities and improve fine motor skills” that will be prescribed, but a specific action that the child must learn to perform. For example, “learn to bring a spoon to your mouth, eat 10 spoons of porridge on your own.” To do this, undoubtedly, you will need to work on your tone and motor skills. But these will all be auxiliary things for a clear purpose and with good motivation.
Rehabilitation uses methods with proven effectiveness (here is a study that helps separate the wheat from the chaff).
In subsequent publications we will examine the main methods separately.
- The rehabilitation program is written individually for a specific child and cannot be the same for children even of the same GMFCS level.
We recognize the fact that no two children with cerebral palsy are alike. Even if the lesion is absolutely the same and the possibilities of movement are also absolutely the same, most likely these will be children with different temperaments and different living conditions. One will live in an apartment building with a ramp, and his priority will be to keep his balance while reaching for the elevator button, or pick up the intercom and open the door, and the other will live in a private house, where it will be important to learn how to keep his balance while walking through his mother’s garden, and climbing the stairs to the second floor of the house, for example.
- You need to work with your child every day. Courses with specialists are very important, but will be ineffective if they are not reinforced every day. Rehabilitation is primarily the work of parents; the task of specialists is to create a program and train parents to perform tasks that they can perform in everyday life without being specialists.
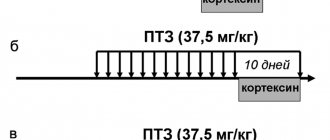
I would like to give an excellent example from the book “Rehabilitation of children with cerebral palsy: a review of modern approaches to help rehabilitation centers” / E. V. Semenova, E. V. Klochkova, A. E. Korshikova-Morozova, A. V. Trukhacheva, E. Yu. Zablotskis. Page 294–297:
“Nastya, a two-year-old girl with spastic diplegia GMFCS II.
Now Nastya is learning to stand at the support and walk along the support. If we assume that the “useful” time of intervention for Nastya is only the time of contact with a specialist, then we will get the following:
The girl will spend 1–2 hours a day doing exercises aimed at improving standing at a support and learning to walk along a support. There may be some other procedures (massage, physiotherapy (electrotherapy), suits, etc.), but, as we have already said, their effectiveness is questionable, so they can not be counted. There may be another 30-40 minutes of standing in the verticalizer. In total we get a maximum of 3 hours. The rest of the time, Nastya will function as she can now, that is, play while sitting on the floor in the W position, crawl on all fours, stand independently at a support, pulling herself up with her arms.
What's the problem? Firstly, if she stays in the “W” position for a long time, Nastya runs the risk of acquiring a specific hip deformity: with internal rotation of the hips and their adduction, the relationship of the head and neck of the femur with the axis of the femoral body is disrupted. Secondly, the girl will not develop balance reactions and rotation of the torso, since in the “W” pose the pelvis is tilted back, the torso is “turned off” from maintaining balance, and rotation is impossible. Thirdly, Nastya risks perpetuating a backward pelvic tilt, which will prevent her from sitting in the correct position - sitting with a “round” back, which, in turn, will limit the use of her hands and the development of reaching and fine motor skills. Finally, the “W” pose will promote plantar flexion in the ankle joint—in a vertical position, this will result in weight bearing on the forefoot. When a girl stands up on her own near a support, she usually “lies” on the support, rests on her toes and hyperextends her knees. This is due to the fact that Nastya often gets up, leaning on the sofa, and the sofa is low and it is convenient to lie down on it, providing herself with maximum support area. In addition, when transitioning from a pose on all fours to a pose standing at a support, the girl pulls herself up with both hands. In this case, flexion patterns are activated and support on the entire foot becomes difficult. When you rely on the forefoot and move the center of gravity forward (support on the sofa!), a biomechanically natural hyperextension occurs in the knee joints. All this leads to the risk of strengthening the support on the forefoot and recurvation of the knee joints, which will significantly affect the subsequent gait pattern.
If we take a new approach to intervention and think about Nastya's daily life as an additional resource for learning movement, developing correct movement patterns, new motor skills and preventing musculoskeletal complications, then we end up with the following strategy:
- It is necessary to limit sitting in the “W” position during the day. At the same time, Nastya needs an acceptable position for independent play on the floor! To do this, you can use a simple and effective device (see figure below).
- To stand upright, a girl needs to stand a lot during the day against a support during games and some activities of daily life. For example, wash your face while standing, and not in your mother’s arms. The support should be at the level of Nastya’s chest - in this case the body will be aligned.
- To learn to move in a vertical position, Nastya needs to walk along a support and be able to move around inside the apartment and outside. That is, the child already needs a properly selected rear-supported walker and the opportunity to walk in it.
- To form proper support on the foot and prevent the recurvation of the knee joint, Nastya needs orthoses for the lower leg and foot. This orthosis must be individually made from a material suitable for foot orthosis! movements such as supporting and transferring weight on the feet, bearing weight on the legs, extending the lower limbs against gravity, transferring weight to one leg. This will require active efforts by a physical rehabilitation specialist and parent training.
If we calculate the time that, if this strategy is followed, can be considered intervention time, it will increase to 5-6 hours a day!
Here is an excellent example of evidence-based rehabilitation of cerebral palsy in Russia.
In conclusion: I do not invent any of my own methods, do not conduct research on drugs and do not sell them. I do not undertake to evaluate the actions of our doctors and parents who choose a different path. I simply translated into Russian studies of methods for treating cerebral palsy according to the rules of evidence-based medicine (with links to these studies), the European consensus on the treatment of children with cerebral palsy, recommendations of large clinics and share them. This article also uses materials from the most powerful advanced rehabilitation specialists in our country, who have amazing success in their work and also rely on the experience and developments of developed countries (an example about the girl Nastya).
If you are not close to the principles of evidence-based medicine, for God’s sake, treat yourself the way you like. I respect everyone’s choice and opinion, but I decided for myself that I cannot participate in a large uncontrolled experiment on other people’s children due to my inner convictions. As soon as a cure for cerebral palsy appears with proven effectiveness and safety, I will be the first to prescribe it to children.
Sincerely, pediatric neurologist Anna Maksimovna Ostroverkhova
(To be continued.)
Source
published 31/10/2018 14:45 updated 01/11/2018 - Child care, hygiene, Growth and development, Treatment methods, Nervous, mental and psychological diseases, Congenital and hereditary diseases, genetics, Neurology and psychiatry, Special children and their families
A virtual reality
This is an artificial world in which a child can identify himself and perform various actions, in other words, this is a real world that obeys the same laws of physics, only in virtual reality.
Artificial intelligence monitors changes that occur in the virtual world and provides the patient with new data and tasks for action. This therapy opens up great possibilities. The system is able to individually adapt to each patient, helping the doctor in the process of patient rehabilitation.
There are more than enough advantages of such virtual therapy, which actually helps patients, including:
- artificial intelligence perfectly adapts to the capabilities and characteristics of each patient, providing exercises that he can do;
- the ability to change the difficulty level of exercises;
- helps to measure the patient’s performance in exercises and use this data to develop further exercises for rehabilitation;
- patients are very happy and friendly about activities in the virtual world, which undoubtedly affects the general condition of the patient;
- in fact, entertainment contributes to patient care.
Cerebral palsy in children: a systematic review of intervention programs
Movement Intervention Programs
By definition, all children with cerebral palsy have motor impairments and have difficulty performing motor-related tasks [255] . The severity of motor impairment in cerebral palsy is decreasing in high-income countries, and comorbid epilepsy and cognitive impairment are becoming less common [2] . Today, three out of four children with cerebral palsy walk independently [2] . These figures are very encouraging. Thus, response to movement intervention programs is more likely than ever, as reductions in brain damage lead to increases in baseline levels of motor, sensory, and perceptual skills and readiness to learn. Accordingly, it is critical to understand the available evidence for the effectiveness of movement intervention programs. There is now a clear division in the evidence base between those methods that work to improve functionality and task performance and those that do not work to achieve those tasks. Evidence from pivotal clinical trials supports the effectiveness of training-based interventions, including action observation training [20, 21] , bimanual training [54–56] , and constraint-induced therapy. movement therapy [46, 62–67] , functional chewing training [137] , goal-directed training [98] , home programs using goal-directed training [112] , mobility training [123, 127] , treadmill training [65, 123, 127] , partial body weight support treadmill training [ 123, 127, 169] and occupational therapy post botulinum toxin [190] (green). Moreover, enrichment with environmental stimulation (green color) is effective for improving task performance [95] . Adapting the environment and tasks to enable their performance through context-related therapy (yellow) [77] is a powerful modulator of effective care. All of these programs have common characteristics: practice of performing real-life tasks and activities using the child's own active movements at high intensity. In this case, the practice is directly aimed at achieving the goal set by the child (or parent, if necessary). The mechanism of action is experience-dependent brain plasticity [256] . Motivation and attention are integral modulators of neuroplasticity, and successful deliberate practice brings pleasure and satisfaction to children, spontaneously creating opportunities for regular practice [256] . In contrast, generic and/or passive motor intervention programs that are structured from the specific to the general produce less results and are sometimes clearly ineffective in improving functionality and movement in children with cerebral palsy. Such programs include craniosacral manual therapy [239–241] , hyperbaric oxygen therapy [234, 235] , neurodevelopmental therapy in its original passive format [108, 129–132] and sensory integration [3] (red).
These results make sense when viewed through the lens of neuroplasticity. Passive movement experience, obtained through the manipulation of a specialist or caring adult, does not require the child to initiate problem solving or activate motor skills. There are also several complementary interventions that can enhance the positive effects of goal-focused movement training when used together. These are electrical stimulation [65, 92–94] , hydrotherapy [108, 110, 111] , taping [159–164] , transcranial direct brain stimulation [101, 166–168] and serious games in virtual reality mode [33–47] ( yellow, weak positive evidence). These types of interventions require further research as children find play interventions to be satisfying and normalizing. Also, in terms of comfort, children preferred electrical stimulation to an ankle orthosis [93] . In addition, children are more patient with taping than with traditional types of orthoses, which often cause discomfort and dissatisfaction or dissatisfaction with the cosmetic effect [73, 140] . Other benefits of these complementary interventions include cardiorespiratory fitness and social integration, the importance of which should not be underestimated. Therapy using a special suit (“astronaut suit”) in addition to motor training did not provide greater benefit [156,157] . Some children experienced respiratory failure, overheating, and peripheral cyanosis. These symptoms resolved when the suit was removed (yellow color, weak negative evidence) [156,157] . Therefore, therapy using such suits is not recommended as a first-line or individual program. This type of intervention must be closely supervised [156,157] . However, it is important to understand that for some families the process and routine of putting on a suit can mean active practice and therefore a more intensive program of assistance, and this can produce positive results. We know that intensive, targeted movement training is effective and works with different forms of assistance [98] . The theory that transcranial direct brain stimulation enhances the effect of motor training through additional targeted stimulation of the motor cortex is logical and requires further research [166–168] .
Existing studies of complementary and alternative intervention programs for children with cerebral palsy have sought to improve motor skills. Research suggests the effectiveness of acupuncture [227, 228] and animal-assisted therapy [102] (yellow, weak positive evidence). In contrast, conductive pedagogy [231, 232] , massage [238] , reflexology [243] , Vojta therapy [244–246] and yoga [248] are not likely to be effective in developing motor skills (yellow, weak negative evidence). In moderate quality studies, craniosacral manual therapy [239–241] and hyperbaric oxygen therapy [ 234] showed no improvement in motor skills between groups and produced serious side effects (red). Proponents of conductive pedagogy may argue that since this approach is holistic, it is inaccurate to analyze it in terms of individual indicators. But these are the motor results that published clinical trials showed. In this regard, it is important to remember that conductive pedagogy can be beneficial for the development of social skills and quality of life [231] . Manual interventions, including massage (green) [237] , craniosacral manual therapy [241] and reflexology [243] (yellow, weak positive evidence), appear to help manage constipation. Massage also helps relieve pain [3] (yellow, weak positive evidence), while yoga has not shown the same results [248] (yellow, weak negative evidence). However, yoga helped improve alertness, muscle flexibility, and balance (yellow, weak positive evidence) [248] .
Working with tone
In 85% of children with cerebral palsy, the main type of motor disorder is spasticity, and in 7% - dyskinesia (including dystonia or athetosis) [2] . Many children have a mixed type of disorders [2] . Spasticity and dystonia cause involuntary movements and changes in body position, which affect motor control and can cause pain. Our review found that the following pharmacological agents and neurosurgical procedures are effective in reducing spasticity: botulinum toxin therapy [185] , intrathecal baclofen [175, 176] , diazepam [3] and selective dorsal rhizotomy [209] (green). Dantrolene [3] and tizanidine [3] are also likely to produce results (yellow). Adjuvant local injections of alcohol appear to reduce spasticity [3] (yellow, weak positive evidence). Local injections of phenol can also reduce spasticity, but for a very short time, and they often cause side effects (yellow, weak negative evidence) [195] . Fewer studies have examined management of dystonia due to its low prevalence and difficulty of identification. Possibly effective pharmacologic treatments for reducing dystonia include local botulinum toxin injections [3] , oral gabapentin [193] , intrathecal baclofen pump administration [177] (yellow, weak positive evidence), and oral trihexyphenidyl. These medications can reduce dystonic and athetotic involuntary movements and increase social participation. But for some children, the side effects of these drugs may outweigh the benefits (yellow, weak negative evidence) [177,196] . Prescribing pharmacological drugs requires as much creativity as a scientific approach, especially for children with cerebral palsy who have underlying, comorbid medical conditions. For example, a child with a combination of dystonia and epilepsy may be better off taking one drug that targets the symptoms of both disorders, such as gabapentin, rather than two different drugs.
In addition, botulinum toxin therapy [187] , intrathecal baclofen [179, 180] and gabapentin [179] have been shown to reduce pain (yellow, weak positive evidence), further supporting attempts to use these drugs in clinical practice. Although their effect on dystonia is not their primary mechanism, numerous other benefits may make these drugs an acceptable intervention for children and parents.
Deep brain stimulation is showing promising results for children with dystonia, which causes pain and severely limits participation in daily life, but this intervention requires further research [177, 198].
In the wake of work on spasticity, research is now actively focusing on better understanding the pathophysiology, histochemistry, and muscle structure of cerebral palsy [257] . Research shows that children with cerebral palsy have increased levels of pro-inflammatory cytokines and genes in the extracellular matrix of skeletal muscle, coupled with increased levels of intramuscular collagen and decreased ribosomal production [258] . New understanding of these pathophysiological muscle changes has led some clinicians to call for reconsideration of the use of botulinum toxin, which causes therapeutic weakness and potential muscle fibrosis [259] . It is still unknown whether the observed atrophy and replacement proliferation of fat and connective tissue in the muscles of children with cerebral palsy are a direct consequence of botulinum therapy, the result of accelerated side effects, or whether these changes are natural in cerebral palsy. We anticipate that, over time, further research into muscle pathology will change program recommendations and, more importantly, lead to the discovery of new interventions.
Sensory Integration
This therapy takes place in a special room – a snoezelen. The room is a multi-sensory environment designed to either stimulate or suppress the patient's core senses through music, various scents, colors, images and other sensory objects.
The environment is controlled, the patient is left to his own devices and has the right to manage his own time and enjoy the environment around him. In such a room, all 5 human senses can be active. The environment can be adjusted and adapted to a specific patient, which has a very effective effect on rehabilitation as a whole.
Sensory integration has the following goals:
- relaxation, pleasure and rest without the interference of the patient’s intellect and expectations from surrounding people, there are no failures in the environment;
- treatment of psychosomatic disorders;
- reduction of aggression, stress and depressive mood;
- activation of all human senses (vision, touch, hearing, taste, smell);
- increased concentration;
- the ability for people with disabilities to respond to stimuli in the created environment or, conversely, to limit the patient from certain ones;
- helps the patient understand and recognize his body in a specific space, improve the coordination of the body in movement in relation to the created environment and space;
- reduction of self-stimulation.
The ultimate goal of being in such an environment is complete sensory integration and the development of the ability of the central nervous system to respond to sensory information, process it and transmit it to the brain through the senses for the body's further response to surrounding objects and environment. This therapy is suitable for both children and adults.
Rehabilitation and habilitation for cerebral palsy
After collecting anamnesis, complaints and assessing the patient’s condition, specialists draw up a treatment plan. A rehabilitation doctor supervises the patient and resolves issues regarding the course of rehabilitation:
- selection of types and quantities of rehabilitation measures,
- the need for surgical intervention,
- selection of technical means of rehabilitation (crutches, wheelchair, lifting mechanisms for the bathroom or bed, household items, etc.),
- necessity and selection of orthotics,
- solving communication problems and a socialization plan for the patient.
A team of specialists jointly draws up a course of rehabilitation, determines the perioral goals and objectives of rehabilitation and habilitation, also together with the parents and, if possible, the child himself. These may be goals aimed at increasing the child’s mobility, teaching daily skills and self-care, social integration, and preventing recurrence and further complications of the condition. Parents and loved ones are taught care skills and ways to help develop the child’s independence for the successful rehabilitation and habilitation of a child with cerebral palsy.
Rehabilitation of cerebral palsy is carried out in several areas.
Functional approach
Depending on the severity of the disease, the child learns physical skills. At the first level of GMFS, the patient trains to maintain balance, shift weight, turn, and perfect familiar movements. The child also learns to roller skate, bike, climb, run, and so on.
In more severe cases, children learn to control the movements of their arms and legs, improve the quality of walking and other movements available to the patient. At the fourth level of GMFS cerebral palsy, the child is taught to support his head, sit independently, give signals of fatigue, and be aware of his body and position in space.
Children learn to maintain and change posture, manipulate objects to achieve everyday and play goals, and learn movements of varying degrees of complexity.
Additional Methods
Before physical exercise, muscle spasms are relieved using manual therapy, massage, and botulinum toxin (Botox) injections. This makes it easier to control your muscles during exercise.
If necessary, orthoses are made - medical devices that the patient wears to support and modify the muscular and skeletal system. These are corsets, orthoses, splints, bandages, orthopedic aids for shoes, insoles, removable devices.
Biofeedback (biofeedback)
With the help of computer technology, the patient sees information about the state of physical processes and learns to purposefully control them.
Kinesio taping
Special tapes called kinesio tapes are glued to certain areas of the body. Tapes improve muscle functioning (relaxation and tension), support joints, and relieve pain. Tapes are not a replacement for orthopedic products.
Physiotherapy, including functional myostimulation and transcutaneous electrical stimulation of the spinal cord
Diagnosis of sensory integration - identifying a malfunction in the organization of sensory signals, thanks to which the brain provides effective reactions of the body and shapes emotions and behavior. Classes with a speech therapist and psychologist.
Bobath method
This method of neurodevelopmental treatment was named after its creators, Bertha and Karel Bobath. The approach to treating patients with cerebral palsy is based on knowledge and development of the nervous system and its pathologies:
- sensory-motor;
- emotional and social development of young children;
- perceptual;
The program is completely individualized and applied exclusively by the hands of a therapist. The focus is on natural sensory nutritional feedback and musculoskeletal control training.
The principles of treatment are:
- learning to sense movement;
- motor pattern training;
- facilitating the natural movement pattern and inhibiting pathology;
- setting goals, taking into account the stage at which motor ability is, the age and abilities of the child, always occurs in close connection with the family;
- assistance in the development of normal motor skills of the child;
The success of achieving goals affects the development of the child’s fine motor skills and speech. Close cooperation with the family is a must.
Treatment conditions for patients with cerebral palsy in Moscow
The number of disabled people diagnosed with cerebral palsy is growing every year, which is largely due to improved quality of diagnosis and tracking system for patients with pathologies of the central nervous system. Timely detection of this type of violation significantly increases the patient’s chances of successfully combating the limitations that this disease dictates. Today, relatives and representatives of such patients often seek help abroad, but modern rehabilitation centers in Russia are not inferior in the quality of treatment for childhood cerebral palsy.
In Moscow, for the purposes of sanatorium treatment and rehabilitation of patients with cerebral palsy, both time-tested mechanical systems and innovative robotic complexes are used to restore movement functions. In addition, every year, as a rule, brings new technical discoveries, including those related to the global Internet network, which can significantly expand the capabilities of patients with a high degree of disability.
Staying in a rehabilitation sanatorium for a cerebral palsy treatment program includes adherence to the correct regimen of physical activity and rest, nutrition, rehabilitation activities and procedures, as well as sociocultural adaptation (creative events, visiting exhibitions, theaters, etc.).
PADOVAN method
This method is also called neurofunctional reorganization of the brain. It is based on the human neurological system, on neuralgia of the development of speech, walking, thought processes, on neuroplasticity of the brain and development through the formation of new synapses.
During a PADOVAN session, several methods are combined: occupational therapy, physiotherapy and logotherapy. Exercises are used for the upper and lower extremities to promote speech learning, coordination of body movements, swallowing and breathing.
The method is effective in treating children:
- with developmental delays;
- with dyslexia;
- with learning problems (reading, numeracy and writing;
- with attention disorders;
- with the presence of hyperactivity.
Medicines
Medicines are used mainly at a younger age, when problems with muscle tone are observed. Next, the drugs are prescribed as maintenance therapy to eliminate complications. Psychological disorders are also treated.
The doctor may prescribe the following medications:
- to stimulate muscle tone: Mydocalm, Baclofen, Dysport;
- medications to improve cerebral circulation: Piracetam, Lucetam, Biotredin;
- vitamins and mineral supplements to strengthen the body.
The doctor adjusts the dosage according to the child’s condition and the effectiveness of the therapy. Taking medications without a doctor's prescription is not recommended.
Additional rehabilitation methods
Free rehabilitation of children with cerebral palsy through government programs should include all of the above methods. But there are a number of treatments that are widely practiced in private centers, along with standard treatments.
Balneotherapy or hydrotherapy
The technique is often used in sanatoriums. Its essence is taking baths with the addition of various minerals. They penetrate the skin and have a positive effect on the entire body. Warm water itself relaxes and calms the child. Children with cerebral palsy are most often prescribed the following types of therapeutic baths:
- chloride;
- hydrogen sulfide;
- iodine-bromine;
- nitrogen;
- pearl;
- oxygen
Often, underwater massage and shower massage are used in complex treatment. Mud therapy gives good results. Applications are applied to the neck-collar area, in the area of the hands and feet. In cases of stunted growth, mud applications are made in the lumbar region to stimulate the adrenal glands.
Swimming with dolphins
Swimming in a pool with dolphins (dolphin therapy) has become popular in recent decades. This technique combines a number of positive effects:
- swimming relaxes and at the same time strengthens muscles, relieves spasms, and hardens;
- contact with dolphins improves nerve conduction and tactile sensitivity;
- children receive positive emotions, which has a good effect on the further course of treatment.
Prices for dolphin therapy are high; not every city has dolphinariums or specialists who provide such treatment. There is no authoritative scientific evidence of the effectiveness of the technique, which is why many doctors do not take it seriously. But parents of children who have undergone dolphin therapy speak very positively about it
Hippotherapy as a method of rehabilitation
There is another type of therapy based on the child’s contact with animals. This time horses act as “therapists”. When riding a horse, a lot of muscles of the human body are used, so it is recommended to combat hyperkinesis, muscle spasms, and contractures. In addition, horses arouse great interest in children, positive emotions, and stimulate communication and discovery of the world.
Author's methods
There are several recognized proprietary rehabilitation methods that are used in many centers along with classical treatment methods. Here are some of them:
- Voight method, or Voight therapy. Its basis is the impact on certain areas of the body with pressure of varying strength. This stimulates the nervous system, which ultimately leads to increased movement.
- Bobath method. It consists of developing a natural motor stereotype in the child. In this case, special, individually selected body styling is used. Children are taught to sense movements and move independently in ways that are as close to natural as possible.
- Bloom's method. The basis of the technique is a deep biomechanical effect on skeletal muscles.
In fact, there are many more original treatment methods. You should consult your doctor about the possibility of using one or another additional method of rehabilitation.
Exercise therapy
Therapeutic exercises help restore lost functions, normalize tone and prevent muscle wasting. It is recommended to perform exercises from an early age - this will help you quickly cope with weak tone and restore self-care.
The following program is recommended:
- physical exercises with a trainer - to develop a specific muscle group;
- kinesitherapy - “treatment with movement” and constant physical activity;
- mechanotherapy – performing approaches on specialized simulators in rehabilitation centers.
The main feature of the rehabilitation of children with cerebral palsy is that the effect appears only with systematic training. That is why you need to fully follow all the doctor’s recommendations and engage in physical therapy.
Diagnosis and consequences
Rehabilitation for cerebral palsy requires a systematic, competent approach. Diagnosis is of paramount importance.
It is necessary to differentiate between cerebral palsy and other neurological disorders. Incorrect treatment can cause undesirable consequences.
A comprehensive assessment of the patient’s condition allows us to accurately determine the nature and degree of development of deviations.
Typical clinical consequences of the disease include:
- Impaired mental function.
- Changes in muscle tone, hyperkinesis.
- Impaired hearing, vision, speech.
- Changes in the skeleton.
- Deformations, tissue contractures.
- Impaired motor activity and coordination.
- Decreased mobility.
- Problems with digestion, breathing, urination.
Rehabilitation of children with cerebral palsy using individual rehabilitation programs will help effectively combat the described health problems. The child gets a chance for full-fledged educational and social activities.
Neurostimulation
This method uses weak currents to stimulate neurons in the brain and spinal cord. This makes it possible to reduce the activity of inhibition in cerebral structures and resume motor activity. Using this method, it is possible to cope with chronic pain and paresthesias, which often arise as complications of cerebral palsy.
The decision to perform neurostimulation is made by the doctor based on the child’s condition. Such therapy is considered successful if it helps eliminate half of all complications.
Physiotherapy
Physiotherapeutic treatment is used as a complement to primary therapy; such procedures strengthen the body. They increase tissue regeneration, activate blood flow in muscles, bones and joints, improving cellular nutrition.
Modern methods of treating cerebral palsy include sessions of the following procedures:
- electrical stimulation;
- magnetic therapy;
- warming up;
- light therapy
Treatment is carried out in courses of 10-15 sessions. You need to visit the office strictly on schedule and not skip physical therapy. A referral can be obtained from a pediatrician or a specialized rehabilitation center.
Is a cure possible?
A complete cure of cerebral palsy, which means the normalization of all impaired functions, primarily motor, is impossible. As a result of exposure to unfavorable factors, some of the child’s brain cells die irrevocably, while another part of the cells are damaged to a lesser extent and cannot perform their function well. Some of the cells do not suffer or are minimally damaged, and therefore can compensate for the functions of dead cells due to the plasticity of the child’s nervous tissue.
Therefore, the main goal of rehabilitation measures is to create optimal conditions for supporting and improving the functioning of damaged areas of the brain, bringing the skills of a patient with cerebral palsy as close as possible to the age norm, step by step moving from more severe disorders to less severe ones.
Our many years of experience in the surgical treatment of patients with cerebral palsy shows that even severe movement disorders in children cannot be regarded as a hopeless situation, and in this case it is possible to achieve satisfactory and even good compensation for impaired functions with properly organized and systematically carried out conservative therapy in combination with timely surgical treatment .
Visit to a psychologist
Working with a psychologist is an important support for a child, which will help with social adaptation. The doctor conducts conversations and finds out what worries the patient in the first place. Game techniques, trainings and questionnaires are used. The program is selected individually according to leading methods for children with cerebral palsy.
During rehabilitation, the emphasis is on physical activity, but without overcoming psychological problems and barriers, it will be difficult for the child to return to social life. Only an integrated approach will consolidate the results obtained.
Treatment methods for children with cerebral palsy
Adaptive physical education
The purpose of the exercises is to develop coordination, expand range of motion, improve motor functions, and strengthen muscles. Instructors teach children to hold their heads up, crawl, kneel, take their first steps, roll over, and sit up. It is important to prevent incorrect postures.
Healing Fitness
A set of procedures: hardening, massage, gradual stretching, fixing the arms and legs in the correct position, their smooth flexion and extension. The procedures improve blood circulation and relieve spasms.
AFC and exercise therapy classes help the child become more independent and resilient. The program is selected individually, depending on the form of the disease. Thus, with muscle atony, the emphasis is on maintaining balance, and spastic diplegia requires continuous movements.
Orthopedic products
Fixing splints, support walkers, soft and rigid SVOSH orthoses, derotational cuffs and special suits allow you to develop the correct motor stereotype. These drugs activate the compensatory mechanisms of the nervous system, which leads to the development of new movements.
Bicycles with safety belts, locking elements and two brakes: parking and hand brakes have been developed for children with cerebral palsy. The height of the bike's back, saddle and side support can be adjusted.
Surgical intervention
To fix the skeleton in the desired position, surgeons resort to bone lengthening or tendon grafting. In case of severe muscle spasticity, leading to the formation of contractures and constant pain, it is necessary to interrupt the pathological impulse coming from the spinal cord. Then the patient is prescribed a spinal rhizotomy.
Drug treatment of cerebral palsy
Aimed at relieving a specific symptom. Thus, when cerebral palsy is combined with epilepsy, the doctor prescribes anticonvulsants, when muscle tone increases, antispastic drugs, and for chronic pain, antispasmodic drugs. Drug therapy may include nootropics, metabolic drugs (glycine, ATP, amino acids), neostigmine, antidepressants, tranquilizers, antipsychotics. All medications are taken strictly according to a doctor's prescription.
Physiotherapy
The most famous methods are electrical stimulation of nerves and muscles, therapeutic electrophoresis, mud and hydrotherapy, and thermal procedures. Immersion in warm water relaxes muscles, relieves pain, and reduces the severity of hyperkinesis. Doctors often prescribe oxygen, radon, turpentine and iodine-bromine baths, herbal baths with pine needles or valerian.
Animal-assisted therapy
Restoration through contact with animals. The most common methods are hippotherapy, canistherapy and dolphin therapy. The session is conducted by two specialists: an instructor and a psychotherapist. Tactile sensations stimulate brain structures. This expands the patient’s range of speech and motor skills. The psychological component is also important: the positive emotions that a child receives during classes with horses, dogs or dolphins.
Speech therapy
Speech disorders are observed in at least 65% of children diagnosed with cerebral palsy. Dysarthria is a pronunciation disorder due to defects in the speech apparatus. Alalia is the absence or underdevelopment of speech due to organic damage to the speech areas of the cerebral cortex. Dysarthria is the most common. Alalia is difficult to diagnose and correct.
Teachers correct speech, help develop breathing, voice and diction, teach children to understand words, facial expressions and gestures.
The speech pathologist begins the lesson by relaxing the facial muscles and articulatory apparatus. Next comes articulation and breathing exercises, voice development, and work on pronunciation of sounds. The next stage is expanding your vocabulary.
Psychological help
The sessions include exercises on attention and memory, perception of objects, color discrimination, and development of fine motor skills. Role-playing games allow you to control emotions and form ideas about people’s relationships.
Psychologists help children work through emotional trauma, accept their physical defect, and learn to love and respect themselves.
ART therapy
Includes drawing, modeling from clay or dough, music, dancing. A release of emotions, stress relief and concentration on the process - all this reduces anxiety, improves memory and thinking.
All these methods of treating cerebral palsy should be used simultaneously and regularly.
Forecasts
Rehabilitation of cerebral palsy depends on the form of the disease and the degree of brain damage. Usually, when therapy is carried out from an early age, the prognosis is relatively favorable - most disorders can be compensated for by primary school age. With a mild form of pathology, the manifestations of cerebral palsy will be almost invisible.
If you delay therapy and do not follow the doctor’s recommendations, the prognosis will be unfavorable. This is a child’s mental retardation and serious dysfunction of the musculoskeletal system. In case of cerebral palsy, parents and children are required to take a responsible approach and implement a rehabilitation program.
Modern rehabilitation
The rehabilitation program is based on an analysis of the problems and needs of the little patient. The foundation of the program is physical training aimed at restoring the movements and activity of children with cerebral palsy.
The main driving force behind a child's development is curiosity. Therefore, we try to conduct classes in a playful way, and reduce the number of mechanical repetitions, the meaning of which is unclear to the child, to a minimum. We believe, and practice confirms, that a positive attitude contributes to a deeper assimilation of new movements.
The foundation of the rehabilitation program for cerebral palsy is the Voight method, which activates and improves motor functions of a reflex nature - crawling, rolling over. In addition, we actively use the methods of Castillo Morales, PNF, manual therapy, “Balance”, RDA.
If a person with cerebral palsy faces problems of lack of strength and physical endurance, lack of balance and coordination of movements, then we conduct part of the classes on the Galileo vibration platform. These exercises save time and greatly facilitate the labor-intensive rehabilitation process. Plus, they are fun, since most children really like the vibration.
Stretching activities are also carried out on the Galileo platform. The effect of such activities comes faster and lasts longer:
- Muscle spasticity decreases;
- Increases strength and performance;
- Improves balance and coordination;
- Volume and muscle mass increase;
- The speed and quality of walking increases;
- The musculoskeletal system is strengthened.
The vibration platform can be rented for a while, so that young patients can practice at home and be able to consolidate the results.
Not all rehabilitation techniques are like play. But the use of some of them, for example Vojta therapy, is especially justified at the age of up to 18 months. Vojta therapy helps to develop an excellent sensorimotor base, sufficient for building other types of therapy - speech therapy, defectology, occupational therapy, functional integration.
All rehabilitation programs are developed strictly individually, based on the physiological state of the patient. With us you can undergo both individual procedures (classes using Vojta or on the Galileo platform) and comprehensive rehabilitation. In addition, our specialists can always come to your home to adjust your exercise program.
Since parents are full members of the rehabilitation team, we always actively share our knowledge with them. By teaching parents therapy methods, we help them gain a wealth of knowledge that will allow them to continue the process of rehabilitation of cerebral palsy at home and consolidate the results achieved.