Causes of headaches during breastfeeding
Headaches are not an independent symptom, but a manifestation of a number of disorders. These may be factors such as hormonal imbalance, vitamin deficiency, as well as pathologies of individual organs and systems. During breastfeeding, tension headaches and migraines often occur, as well as those associated with changes in hormonal levels.
Tension headaches
Main article: Tension headache
This type of headache is often associated with stress, lack of sleep, and nervous tension. It is described as a sensation of squeezing the head in the form of a hoop, without additional symptoms such as nausea, increased sensitivity to light, and others. Tension headaches can be acute or chronic, but often go away after normalizing your sleep and rest schedule, as well as replenishing vitamin and mineral deficiencies.
Migraine
Migraine is one of the common types of headaches. It occurs independently and is not associated with pathologies of other organs and systems. Before an attack of pain, a migraine aura often appears, which is a complex of characteristic symptoms:
- increased sensitivity to bright light, lacrimation;
- increased reaction to loud sounds;
- nausea, dizziness, appearance of dark circles in the field of vision;
- rapid pulse.
Migraines often worsen in women during breastfeeding. The main reasons are sleep disturbances, hormonal changes, and increased anxiety. Specific potent drugs are used for treatment, but they are not recommended for use during breastfeeding. To improve your well-being, you can massage your neck and head, provide yourself with rest and use relaxing essential oils.
Other reasons
Headaches during breastfeeding are a consequence of the general condition of the body. They can occur for many reasons:
- increased levels of certain hormones in the blood;
- increased anxiety;
- lack of sleep, frequent awakenings at night;
- tension in the muscles of the neck and back.
It is important to understand that chronic spinal diseases may worsen during breastfeeding. During pregnancy and then when caring for a child, the load on the lumbar region increases, and problems in the cervical and thoracic regions may also arise. This affects the blood supply to the brain and can cause severe pain.
Pregnancy, breastfeeding, migraine: is there a connection?
According to clinical studies, in 70% of women suffering from migraines, attacks become less frequent, milder, or even disappear completely during pregnancy.
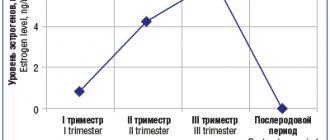
It's all about estrogen levels: it has been proven that low levels of this hormone in the blood can provoke migraine attacks in people who are genetically predisposed to it. Estrogen levels vary throughout the menstrual cycle, and decrease most before the onset of menstruation; Therefore, for many of us, migraine is a familiar companion to PMS. Ten out of a hundred women with migraine also experience menstrual migraine - a special form of migraine that occurs exclusively 2 days before the start of menstruation and the first 3 days after.
During pregnancy, estrogen levels peak and stabilize, so most women who suffer from migraines forget about them for nine months. And yet, up to 28% of pregnant women continue to experience attacks, and it is during pregnancy that the so-called migraine aura may first appear.
What is an aura during migraine?Migraine aura is a special neurological disorder that occurs in the period before a migraine attack. But there are also more frightening symptoms: numbness and tingling that spread from the face to the arm or vice versa. For some people, these migraine sensations are normal, but if they appear for the first time, especially during pregnancy, you should urgently consult a doctor for stroke and other conditions requiring medical attention. |
After childbirth, natural estrogen fluctuations are restored, so often migraines that were absent during pregnancy return during breastfeeding. In addition, the birth of a baby is not only a great joy, but also sleepless nights, missed breakfasts, fatigue and a lot of anxiety. Unfortunately, all this can lead to more frequent and worsening migraine attacks.
Diagnostic methods
Comprehensive diagnosis is an important stage for prescribing competent treatment. It is important to determine what caused the headaches in order to select effective and safe medications. The doctor may prescribe the following stages of examination:
- general and biochemical blood tests;
- determination of hormone levels in the blood;
- diagnostics of the condition of the heart and blood vessels (pressure measurement, electrocardiography, Dopplerography of the vessels of the neck and head);
- radiography of the thoracic and cervical spine;
- MRI, CT as necessary.
At the Clinical Brain Institute, you can undergo a full examination to determine the cause of headaches during breastfeeding. In our center, diagnostics are carried out using modern equipment, which allows us to obtain the most accurate results.
Medicines
During breastfeeding, all medications pass into breast milk to one degree or another, so be sure to consult your doctor before taking them.
If the headache is unbearable, it is better to give preference to paracetamol, since its concentration in milk is minimal, and it can be used by a nursing mother regardless of feeding time. Ibuprofen may also be considered to control high-intensity attacks. There is evidence that ibuprofen in small quantities can pass into breast milk without any negative consequences for the health of the infant, however, if it is used frequently (more than 2 times a week), we can talk about stopping breastfeeding. Aspirin is strictly contraindicated (contraindicated in children under 15 years of age; it should also not be used during breastfeeding).
If a headache significantly interferes with your normal life, you need to consult a doctor who will select effective and safest medications for the child to prevent attacks. This is, for example, propranolol. But only a doctor should prescribe medications, taking into account the circumstances of your disease and contraindications!
You can learn more about medications approved for nursing mothers on the LactMed website.
For those who are interested in delving deeper into this topic
There is a recording of the broadcast with our neurologist Daria Zakharovna Korobkova. See the post on our Instagram account “Broadcast recording: migraine during pregnancy and breastfeeding.”
Subscribe to our Instagram to read the latest materials about the diagnosis and treatment of headaches!
Treatment of headaches
To relieve pain, you can use simple painkillers that are safe for children: paracetamol, ibuprofen, ketoprofen. Potent drugs are contraindicated because they can pass into milk. There are also ways to relieve pain without using drugs:
- provide yourself with rest, try to establish a sleep schedule;
- take a warm bath with the addition of sea salt and herbal infusions;
- apply a few drops of essential oils (lavender, mint, eucalyptus) to the area behind the ears;
- massage your neck and head.
The doctor will prescribe complex treatment for back diseases and circulatory disorders after breastfeeding is completed. During this period, it is important to avoid stress and follow general recommendations.
What to do if a mother has a fever while breastfeeding
Experts say that most medications are not suitable for use during lactation. It must be remembered that a nursing mother can take any medications, including antipyretics, only as prescribed by a doctor. The use of antipyretic drugs is advisable only when the temperature rises above 38 0C. Lower temperatures are an adequate response of the body to the virus and do not require medical intervention.
If the temperature rises and a nursing mother needs help in the form of taking medications, it is recommended to take antipyretics, which include ibuprofen and paracetamol, during breastfeeding.
Prevention methods
The first months of a child’s life are a huge responsibility and stress. At this time, the mother’s body experiences heavy stress, to which it reacts with a prolonged headache. However, if you follow several recommendations from doctors, you can avoid deterioration in health and other dangerous consequences:
- use pillows and other feeding devices - they relieve stress on the spine;
- eat well, take complexes of vitamins and microelements if necessary;
- take time for walks - a sufficient amount of oxygen is necessary to nourish brain cells;
- Avoid stress and allow yourself periodic rest.
At the Clinical Brain Institute, you can undergo a complete examination, which will allow you to quickly and accurately determine the cause of your headaches. The doctors of our center are specialists of a narrow and broad profile with many years of experience in treating various diseases. The effectiveness of therapy will depend on the timely use of prescribed medications, as well as on the implementation of additional recommendations, including adherence to diet and regular exercise.
Clinical Brain Institute Rating: 5/5 — 1 votes
Share article on social networks
Use of medications during breastfeeding
It happens that during lactation a woman gets sick. And she needs to choose medications that would help fight the disease and not harm the child. It should be borne in mind that a wide range of antiviral drugs are absolutely not suitable for treating a nursing woman.
After all, not only useful substances are transmitted with mother’s milk, but also medications that a woman takes, and as you know, not all drugs are suitable for babies. There are also medications that can reduce milk production or stop it altogether. Therefore, when prescribing drugs, the risk for the baby and the benefit for the mother are always taken into account.
The degree of adverse effect of the drug on the infant’s body is determined by the following factors:
- toxicity of the drug;
- the true amount of the drug entering the child’s body (it depends on the dose, concentration of the drug in breast milk and on the amount of milk consumed by the child);
- the peculiarity of the drug’s effect on the child’s internal organs;
- the duration of removal of the medicine from the child’s body (this depends on the maturity of the enzyme systems, the maturation of the baby’s liver and kidney function);
- duration of medication taken by a nursing mother;
- the child’s individual sensitivity to this drug;
- risk of developing allergic reactions.