- When is Morton's neuroma surgery performed?
- Diagnosis and preparation for surgery for Morton's neuroma
- How does the surgical treatment of Morton's neuroma proceed at the Gelenk Clinic?
- Which surgeon operates on Morton's neuroma?
- What type of anesthesia is offered to the patient before Morton's neuroma surgery?
- Postoperative period, rehabilitation treatment and aids after surgery for Morton's neuroma
- Will I feel pain after Morton's neuroma surgery?
- What are the conditions of stay at the Gelenk Clinic?
- What should you pay attention to after surgical treatment of Morton's neuroma?
- What is the cost of foot surgery?
- How to make an appointment with a doctor and surgery for Morton's neuroma?
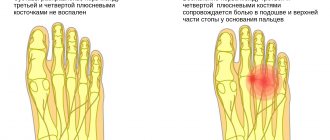
Morton's neuroma (red) as swelling between the metatarsal bones (blue).
Irritation of the nerve (yellow) develops a burning and stabbing pain throughout the area of its supply. © Dr. med. Thomas Schneider Morton's neuroma is a benign thickening of the nerves in the metatarsal area. The consequence of the disease is shooting, burning and stabbing pain in the plantar region, as well as in the toes (metatarsalgia). The pain is so severe that the patient experiences relief and improvement in general condition only when he sits down and takes off his shoes. Thus, when the patient is not wearing shoes, the pain goes away much faster. In addition, characteristic symptoms of Morton's neuroma are tingling or numbness in the toes. Morton's neuroma is a common consequence of transverse flatfoot, sometimes accompanied by hallux valgus. Women suffer from Morton's neuroma much more often than men. The reason for this is most likely due to different fashions for shoes: High heels, as well as shoes with pointed toes, put strong pressure on the front arch of the foot and can provoke the appearance of transverse flat feet. As a result of this pathology, the position of the metatarsal bone changes in the patient and the pressure on the nerves passing along the plantar region of the foot increases.
Morton's neuroma is also diagnosed in men, most often in those who engage in high-volume running sports. Morton's neuroma is often observed between the 3rd and 4th toes, and less commonly between the 2nd and 3rd toes.
send a request
When is Morton's neuroma surgery performed?
In order to correctly assess the patient’s condition and prescribe the correct treatment, Gelenk Clinic specialists will need to provide current MRI results. Based on the MRI images, the doctor determines the degree of need for surgical treatment of Morton's neuroma. If there are certain indications, the patient is prescribed the best surgical technique for him.
In the early stages, treatment of the disease is carried out using conservative methods, namely special insoles and gymnastic exercises for the feet. If the quality of life is significantly limited, and if the patient experiences severe pain despite conservative treatment, the doctor will refer him for surgery. If the thickening is 0.8 cm in size, a nerve-sparing operation (neurolysis) is performed. If the swelling of Morton's neuroma is greater than normal, the nerve is removed through neurectomy.
Treatment of polyneuropathy of the lower extremities
A patient with polyneuropathy of the lower extremities needs to prepare for long and difficult complex treatment. Since it consists not only in relieving symptoms that poison life, but also in eradicating the root cause of the disease.
As a result, the nerve fiber is destroyed, and it will take a long time to restore it. The course of treatment begins with a direct impact on the factor that caused the polyneuropathy, that is, with the relief of the underlying disease or stabilization of the patient’s condition.
For example, if the cause of the disease is diabetes mellitus, then all efforts are initially aimed at reducing blood sugar levels; in case of an infectious type, drug therapy is aimed at fighting the infection, and if the root of the problem is hidden in a deficiency of B vitamins, then it is important to compensate for the deficiency in a timely manner. If the cause of polyneuropathy is disruption of the endocrine system, the doctor prescribes hormonal therapy. But vitamin therapy is more widely used in treatment.
Positive results are demonstrated by those drugs that are aimed at improving blood microcirculation, and therefore nourishing nerve fibers.
Physiotherapeutic techniques, such as electrophoresis, are actively used in treatment. If polyneuropathy of the lower extremities is accompanied by severe pain, the patient must be prescribed painkillers, locally and orally.
It is impossible to completely insure yourself against the disease. But you can try to prevent it using simple precautions. That is, when working with toxic substances, it is imperative to use appropriate protective equipment, take any medications only after consultation and prescription of a doctor, and do not let infectious diseases take their course, preventing them from going into a chronic inflammatory period, when it will no longer be possible to cure the disease and all that remains is to treat it. exacerbations and relieve symptoms. The simplest measures to prevent problems are a balanced diet rich in vitamins, constant physical activity, and avoidance of alcoholic beverages.
Initially, treatment is aimed at eliminating the cause, and then maintenance therapy continues. It is necessary to discontinue medications and eliminate the effects on the body of toxic substances that caused the disease, adjust the diet, supplementing it with the necessary vitamins. Considering that only these measures slow down the course of the disease and reduce complaints, recovery progresses extremely slowly and may be incomplete.
If the cause cannot be stopped, all treatment is reduced to minimizing pain and disability. A rehabilitation specialist and physical therapist will recommend special orthopedic devices.
Tricyclic antidepressants and anticonvulsants are prescribed to relieve neuropathic pain such as burning or pins and needles. Medicines that affect the central nervous system are selected individually for each patient, depending on the state of the body and the patient’s psyche. It is strictly prohibited to prescribe medications on your own, so as not to cause even greater harm.
For demyelinating polyneuropathy of the legs, treatment based on immunomodulators is often used. Plasmapheresis or intravenous administration of immunoglobulins is recommended for acute inflammatory demyelination.
For chronic myelin dysfunction, plasma exchange or intravenous administration of immunoglobulin, corticosteroids or metabolic inhibitors is prescribed.
Of the entire list of vitamin preparations, preference is given to vitamins B1 and B12, which are also called thiamine and cyanocobalamin. The substances improve the level of transmission of excitation throughout the nerve fiber, which significantly reduces the manifestations of the disease, and also additionally protects the nerves from the effects of active radicals. They are prescribed over a long course in the form of injections administered intramuscularly.
Even if the treatment was successful and all or most of the nerve fibers were restored, it is too early to relax. It is necessary to carry out a long course of rehabilitation therapy, since with polyneuropathy, the muscles first suffer, losing tone. Therefore, long-term work aimed at restoring mobility is necessary; the help of several specialists may be required at once.
During rehabilitation after an illness, massage is mandatory. It repeatedly improves blood supply, restores mobility and elasticity to muscle tissue, and improves metabolic processes.
A similar effect is provided by various physiotherapeutic techniques. They also improve microcirculation, reduce pain and restore muscle cells. Physiotherapy for polyneuropathy of the lower extremities is most useful, so it is not recommended to neglect it.
In cases of severe injuries where complete recovery is not possible, the assistance of an occupational therapist may be required. Occupational therapy is action therapy. The specialist helps facilitate the patient’s process of adaptation to a state of limited movement, develops a new algorithm of movements necessary to perform everyday activities.
Due to the uniqueness of each case, the scheme of rehabilitation measures is developed individually and depends on the patient’s condition. Rehabilitation may include vitamin therapy, long-term work with psychologists, diet therapy and other techniques, depending on the specific situation.
Treatment of polyneuropathy of the lower extremities must begin immediately, without delay. As soon as alarming symptoms appear, you should consult a doctor - without timely treatment, there is a high risk of complications in the form of paralysis, disruption of the cardiovascular and respiratory systems. Timely treatment will help reduce the likelihood of complications to a minimum and maintain full functionality. Don’t forget about restorative therapy, it is this that will consolidate the effect obtained from the treatment.
Diagnosis and preparation for surgery for Morton's neuroma
Clinical examination of Morton's Neuroma using a provocative test (Mulder test): A foot specialist diagnoses the disease by compressing the heads of the metatarsal bones and simultaneously palpating the intermetatarsal spaces, which causes pressing pain. © joint-surgeon
Alternative Causes of Forefoot Pain
- Inflammation of the joint located between the bones of the metatarsal and proximal phalanges
- Nerve damage
- Stress (stress fractures) of the metatarsals
- Changes in soft tissue structure, including scars, warts and tumors
- Incorrect weight distribution, as in the case of severe flat feet
Before starting treatment for Morton's neuroma, the doctor conducts a full clinical and imaging diagnosis, which includes a preliminary conversation, physical examination, and MRI with contrast. During magnetic resonance imaging, the patient is in the “lying on his stomach” position, and during the x-ray in the “standing position”. In order to determine how the pressure is distributed under the plantar part of the foot, a podometric study (pedobarography) is carried out at the Gelenk Clinic. Based on the results obtained, the doctor discusses the upcoming operation with the patient.
If the patient’s health condition does not prevent surgical treatment, the operating doctor tells the patient in detail about the course of the operation and also explains possible complications. In addition, you will be referred to an appointment with an anesthesiologist, who will re-analyze the results of the studies and determine whether your condition allows the administration of anesthetics. As a rule, Morton's neuroma surgery takes place the next day after agreement with the operating surgeon and anesthesiologist.
Symptoms
Pain in the legs can indicate various diseases, but the symptoms of leg myositis are specific:
- myositis of the thigh, leg or foot appears unexpectedly, often in the morning after sleep;
- pain in the leg muscles is aching in nature, but worsens when moving or touching;
- the muscles are tense, there are compactions in places;
- if the cause of inflammation is a leg injury, suppuration may develop in the myositis area;
- weakness in the leg muscles, difficulty walking.
How does the surgical treatment of Morton's neuroma proceed at the Gelenk Clinic?
Surgery makes sense if conservative treatment, for example, orthopedic insoles, special shoes with butterfly soles, foot exercises, as well as injections of local anesthetics and self-massage do not help relieve pain for a long time. Gelenk Clinic mainly uses two treatment methods: nerve-sparing neurolysis and nerve removal. Each operation lasts about 30 minutes.
Ventral view of the foot: Morton's neuroma is located between the 2nd and 3rd toes. Most often, pathology occurs between the 3rd and 4th fingers. © Viewmedica
Nerve-sparing minimally invasive surgery for Morton's neuroma
Mechanical pressure on the plantar area of the foot leads to pinched nerves. Due to nerve irritation, the connective tissue sheath of the plantar nerve swells and forms scar tissue. There is an accumulation of fluid.
As a result of the swelling, ischemia occurs and the nerves of the foot are no longer supplied with nutrients. Because of this, the patient develops such characteristic complaints as a feeling of numbness, shooting pain and itching (pins and needles) in the foot. Relieving mechanical pressure on the nerve may relieve these symptoms to a certain extent.
The optimal treatment for many compression syndromes (eg, carpal tunnel syndrome) is nerve decompression. If the Morton's neuroma is less than 0.8 cm in size, nerve-sparing surgery is performed
Using the technique of stress relief and, if necessary, decompression of the nerve by repositioning the metatarsal bone, the specialists of our clinic have been achieving excellent results for several years. In particular, Gelenk Clinic has a good record in preventing relapses. Recurrence of the pathology is more likely after nerve amputation (neurectomy), since this operation does not correct the original violation of the arch of the foot. Despite this, neurectomy is the standard treatment for Morton's neuralgia. Too often, for Morton's neuralgia, the plantar nerve is removed without first testing the effectiveness of nerve-sparing treatment.
Advantages of nerve-sparing surgery:
Nerve-sparing endoscopic treatment of Morton's neuroma with a superior approach instead of the conventional plantar approach has the following advantages:
- less scarring and therefore little irritation of the foot nerves
- the risk of hematomas is reduced
- preservation of the plantar nerve, which after complications will stop hurting and return to its original functions
- reduction in relapse rate: due to the reappearance of painful swelling, relapse is not uncommon
- decreased tendency to form painful scars in the area of the metatarsal nerves
Neuroctomy - removal of the inflamed nerve
During this surgery, diseased nerve tissue from the tibial nerve is removed. At the Gelenk Clinic, neurectomy is performed in cases of severe swelling of Morton's neuroma. That is why this surgical treatment requires a preliminary MRI examination, which helps doctors determine the size of the disease. Since slice-by-slice images obtained using magnetic resonance imaging sometimes do not provide complete information about the size and location of Morton's neuroma, the exact technique is chosen directly during surgery after analyzing and examining the thickening.
With surgical access to Morton's neuroma through the head of the metatarsal bone, decompression can be relatively performed, that is, the degree of compression can be reduced. This method of treatment is an appropriate accompanying surgical procedure, since reducing compression reduces the likelihood of relapse, that is, secondary rupture of the stump of the damaged nerve, resulting in swelling of the connective tissue. Surgery for Morton's neuroma with a superior approach avoids scarring on the sole of the foot. This speeds up the wound healing process, and the patient can resume putting weight on the foot a little earlier.
Causes of development, manifestations and therapy of plantar aponeurosis
Plantar aponeurosis is a foot condition that is common among those who spend a lot of time on their feet. Both medications and surgery are used for treatment. It all depends on the severity of the disease and the factors associated with it. It is for this reason that it is worth paying attention to the various manifestations of pain.
Description of the disease
Any pain should not be ignored. The thing is that this is how the body sends us signals that something is wrong with it. And if you ignore such signals and do not consult a doctor, you can become disabled forever.
In the case of plantar aponeurosis, inflammation occurs at the junction of the heel bone and toes. Initially, the first symptoms may be mistaken for flat feet,
however, if treatment is not started, the situation will only get worse. As a result, the pain in the heel area will only intensify. This will be especially noticeable in the morning. Moreover, throughout the day the pain will remind you of itself, if at all, it will not be so strong. Exceptions are cases when there is a load on the legs with increasing pain.
Main causes of the disease
When talking about the causes of the disease, we should not forget about the risk factors that contribute to the onset of the disease. So, in the case of aponeurosis of the sole, it all starts with such a common phenomenon among athletes as a sprain
. This is especially true for those that support the arch of the foot. The following categories of people may experience this disease:
- long-distance trekkers, such as hikers or race walkers;
- often organize long-distance races;
- those who are overweight;
- those who often wear tight or uncomfortable shoes;
- if there is shortening of the Achilles tendon;
- suffering from hypertonicity of the calf muscle.
The risk group for developing this pathology includes people aged 40 to 60 years and older. This disease is most often observed in women, while men, on the contrary, are practically protected from it.
In addition to runners, those who actively engage in aerobics or dance sports can get aponeurosis of the sole. It is for this reason that it is best for all those who strive to lead a healthy lifestyle to be attentive to their health, especially the stress on their legs.
The risk group also includes people of certain professions. Among them:
- factory workers;
- teachers;
- sellers;
- workers and specialists whose occupation requires them to be on their feet for long periods of time.
Main symptoms of the disease
The main symptom by which the appearance and development of a disease such as plantar aponeurosis can be determined is pain in the heel area. It is by this sign that the disease can be diagnosed almost at its very beginning. Moreover, in the absence of the necessary treatment, the pain will spread to the entire foot, turning walking into real torture. Very often, in advanced cases, inflammation occurs in the second leg.
The peculiarity of the disease is that by periodically allowing the legs to rest, the pain becomes less acute. This is precisely the danger of aponeurosis, since it can masquerade as ordinary fatigue and a person does not seek medical help for a long time.
Possible complications
When talking about the disease, it is worth telling about what complications may arise if you delay in seeing a doctor. These include:
- chronic pain syndrome - occurs if the patient uses the peculiarity of the disease and gives rest, thereby reducing the level of pain, as if getting used to it;
- Various diseases associated with the feet may occur;
- When the disease is advanced, inflammation can spread from the feet to the legs, thighs, and even the back.
How is it diagnosed?
For diagnosis, you should contact a professional and not self-medicate. The best way to determine the disease and its severity is to use MRI, CT or X-ray. With their help, the doctor will be able to see what is happening in the foot. The pain will be the result of plantar aponeurosis or another cause. For example, pain can be caused by injuries in the form of a crack due to an impact, a sprain or a pinched nerve.
How to treat
To achieve healing, you must strictly follow all the doctor’s recommendations. However, traditional medicine can also be used to help pharmacological drugs. They will not only allow you to get rid of the disease faster, but will also enhance the effect of medications.
For treatment, you can make compresses. To do this, you need to take a black radish, grind it on a grater, and then apply the resulting pulp to the heel, wrapping it in a plastic bag and bandaging it or putting on a warm sock. It is good to do such compresses at night. The recommended number of procedures is 5.
A compress of raw potatoes, grated, will help a lot. Here everything is done in the same way as in the radish recipe. Number of recommended procedures – 7.
A compress made from cabbage leaves and honey will help. Take fresh cabbage leaves. They need to be coated with honey and applied to the heel. After this, the foot should be wrapped in cellophane and bandaged or put on a warm sock. Repeat the procedure 8 times at night.
A good solution to relieve pain can be foot baths using sea or table salt: 3 teaspoons per 1 liter of warm water. 20 minutes is enough to achieve a positive effect.
You can use iodine baths.
To do this, take 3 liters of hot water and dissolve 4 tablespoons in it. Yoda. The procedure should be carried out before bed for 20 minutes. Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Which surgeon operates on Morton's neuroma?
One of the features of the Gelenk Clinic is the trusting relationship between doctors and patients. That is why your attending physician will take care of you from the first examination until the operation itself. This way you will have a specialist whom you can contact at any time convenient for you. The Gelenk Clinic's highly qualified experts in the field of foot and ankle surgery are Dr. Thomas Schneider and Dr. Martin Rinio. Also, Dr. Schneider and Dr. Rinio are certified specialists who are annually audited by the independent German Association of Foot and Ankle Surgeons (German DAF) for advanced training, diagnostics and quality of operative activities. That is why the Gelenk Clinic Orthopedic Medical Center has the honor of being called the Specialized Center for Foot and Ankle Surgery (ZFS).
What type of anesthesia is offered to the patient before surgery?
Typically, surgical treatment of Morton's neuroma is performed under general anesthesia. If the patient refuses this method for personal reasons, there is the possibility of using spinal anesthesia. To do this, the surgeon injects an anesthetic into the spinal canal of the lumbar spine. In this case, the patient is fully conscious. What type of anesthesia is most suitable for the patient is determined during a conversation with the anesthesiologist. Our anesthesiologists are true masters of their craft, who during your appointment will offer you the best method that meets all the indicators of previous examinations.
Will I feel pain after Morton's neuroma surgery?
Every operation is associated with some pain—and Morton's neuroma surgery is no exception. As a rule, we try to reduce pain after Morton's neuroma surgery to a minimum. That is why pain treatment begins already during the operation. In most cases, the anesthesiologist will administer a special injection that will numb the foot for about 30 hours. After this, the pain decreases significantly and the patient’s treatment continues with conventional medications. The main thing for us is to ensure a painless postoperative period.
general description
Plantar nerve disease (plantar nerve neuropathy, Morton's metatarsalgia) (G57.6) is a pain syndrome in the forefoot caused by compression of the branches of the plantar nerve by perineural fibroma or other factors.
| 1 - deep transverse metatarsal ligament of the III and IV fingers; 2 - 4th plantar digital nerve; 3 - lateral plantar nerve; 4 - medial plantar nerve |
It is more common in women aged 40–50 years, and has a one-sided pain pattern.
Biomechanical obstacles leading to irritation and compression of the plantar nerve can be caused by foot trauma (30%), wearing tight high-heeled shoes (70%), prolonged squatting (50%), and transverse flat feet (50%).
What are the conditions of stay at the Gelenk Clinic?
Private ward at the Gelenk Clinic in Gundelfingen, Germany.
© joint-surgeon During your stay at the Gelenk Clinic, you are usually in a separate room, which has a shower and toilet. In addition, we provide towels, bathrobes and slippers. You can also use a safe and minibar. All rooms are equipped with TV. You only need to take medications, comfortable clothes and nightwear with you. Patient care is provided around the clock. The medical staff and physiotherapists at Gelenk Clinic will always answer all your questions. Generally, the length of hospital stay is 3 days. Your relatives can stay at a nearby hotel. Our staff will be happy to take care of your room reservation.
What should you pay attention to after surgical treatment of Morton's neuroma?
Immediately after surgery, the foot should be elevated. To avoid pain and swelling, apply a cooling compress to the foot. After about 10 days, the stitches are removed. After this you can take a shower again.
You also receive special shoes that take the load off the forefoot and transfer the body weight to the heel. If you are planning long walks, you should also take elbow crutches. Prevention of thrombosis during the impossibility of full weight bearing on the foot is necessary. This will prevent dangerous blood clots from forming. Physiotherapy and lymphatic drainage prevent muscle loss and swelling of the forefoot. The duration of forefoot swelling often depends on the age of the patient.
- Inpatient treatment: 2 days
- Recommended length of stay in the clinic: 5-6 days
- When can you fly home: 3 days after surgery
- When is it recommended to buy a return ticket: 5 days after surgical treatment
- When is it permissible to shower: after 10 days
- Length of stay on sick leave: 5 days
- When is it recommended to remove stitches: after 10 days
- Outpatient physical therapy
- When can you drive again: in 4-5 weeks
- Sports activity: at least 6 weeks after surgery
Diabetic neuropathy
Symptoms of Diabetic Neuropathy
Depending on which part of the nervous system is most affected, the symptoms of diabetic neuropathy may vary.
With peripheral polyneuropathy, a complex of sensory and motor disorders develops, most pronounced in the extremities. In this case, diabetic neuropathy of the lower extremities occurs. The disease is manifested by numbness, burning, tingling of the skin, as well as pain in the feet, fingers and toes, and short-term muscle cramps. With peripheral diabetic neuropathy, increased sensitivity to even light touch may develop, as well as insensitivity to temperature stimuli. These symptoms are usually worse at night, and even the mere touch of a blanket to the skin causes pain. Diabetic neuropathy may cause muscle weakness and weakening and loss of reflexes. This leads to impaired coordination of movement and changes in gait. The debilitating pain of peripheral diabetic neuropathy can cause loss of appetite, weight loss, insomnia, and even lead to depression.
In later stages of development of peripheral diabetic neuropathy, the patient may develop toe deformities, foot ulcers, and collapsed arches. Very often, peripheral diabetic neuropathy becomes a precursor to the neuropathic form of diabetic foot syndrome.
Autonomic diabetic neuropathy can occur in different forms and is characterized by dysfunction of both individual organs and entire systems.
The cardiovascular form of autonomic diabetic neuropathy can develop in diabetes mellitus within the first five years. It manifests itself:
- arrhythmia - disturbance of heart rhythm;
- rapid heartbeat;
- severe weakness when trying to stand up, associated with a decrease in blood pressure when lying down;
- by reducing the pain sensitivity of the heart, even a heart attack can be painless.
With the gastrointestinal form of autonomic diabetic neuropathy, the patient experiences various pathologies in the digestive system: impaired swallowing, stomach cramps leading to vomiting. Since the gastric sphincters in a patient with diabetic neuropathy are relaxed, this causes frequent heartburn and belching. In addition, in a patient with a gastrointestinal form of diabetic neuropathy, the motor-evacuation function of the stomach is impaired. Intestinal motility may decrease, and then the patient experiences chronic constipation. With accelerated peristalsis, a person suffers from diarrhea (up to 20 times a day, most often at night). But the food has time to be absorbed, so the person does not lose weight. Patients with diabetic neuropathy have an increased risk of cholelithiasis and gallbladder dyskinesia. From the liver, the development of fatty hepatosis is possible.
The urogenital form of autonomic diabetic neuropathy is usually accompanied by urinary incontinence or urinary retention. Patients with diabetes may develop infections such as cystitis and pyelonephritis. In men with diabetic neuropathy, erectile dysfunction is observed, in women - anorgasmia, vaginal dryness.
Sudomotor disorders in diabetic neuropathy are accompanied by disruption of the sweat glands. First, the patient experiences severe sweating, especially at night and on the upper half of the body. The feet and face sweat profusely, and the patient develops a pronounced blush on his cheeks. Over time, due to capillary spasm, the sweat glands begin to produce insufficient sweat, and the skin becomes dry. It develops spots with a large amount of melanin or lack of it. The protective function of the skin in diabetic neuropathy is impaired, and inflammation develops at the site of even minor injury. This can lead to the development of gangrene and non-traumatic amputation of the limbs.
The respiratory form of diabetic neuropathy can occur with hyperventilation and decreased surfactant production.
With diabetic neuropathy, asymptomatic hypoglycemia, symptomatic hemeralopia, diplopia, progressive exhaustion, and thermoregulation disorders can often develop.
What is the cost of foot surgery?
In addition to the cost of surgical treatment for Morton's neuroma, it is worth considering the additional costs for diagnostics, doctor's appointments and aids (eg elbow crutches), amounting to approximately 1,500 to 2,00 euros. If you plan to undergo outpatient physical therapy treatment after surgery, we will be happy to provide you with an estimate of the costs. Information regarding the cost of hotel accommodation and possible additional treatment at a rehabilitation center can be found on the corresponding website.
How to make an appointment with a doctor and surgery for Morton's neuroma?
First of all, to determine the size of Morton's neuroma, as well as to diagnose possible other diseases, foot specialists in Germany will need current MRI images of the foot and X-ray results. Once we receive all the necessary documents, within 1-2 business days we will email you information for patients, as well as a preliminary cost estimate for treatment of Morton's neuroma.
Foreign patients can make an appointment for Morton's neuroma surgery in a short time. We will be happy to assist in obtaining a visa after the advance payment indicated in the estimate has been received into our account. If a visa is not issued, the amount received is returned to you in full.
Due to sometimes long flights, we try to keep the time between the first examination and surgery to a minimum. During outpatient and inpatient treatment of Morton's neuroma, you will be able to use the services of qualified medical personnel who speak several foreign languages (eg English, Russian, Spanish, Portuguese). Payment for a translator (for example, into Arabic) is carried out separately. We also organize transfers, we can book a hotel room, and we will tell you how to spend time in Germany for you and your relatives.
send a request
Causes of neuralgia of the feet
The following conditions may cause nerve pain in one or both legs.
Baxter's neuropathy
Baxter's neuropathy
is a form of pinched nerve caused by compression of the lateral calcaneal nerve, which is located just under the base of the arch of the foot. Risk factors include:
- plantar fasciitis - inflammation of the plantar fascia, the part of the foot that connects the heel bone to the toes
- obesity
- heel spur
- flat feet
Morton's neuroma
Morton's neuroma involves thickened tissue that compresses the nerves between the toes. The patient may notice pain in the bottom of the foot, which gets worse when walking, especially in high heels. The pain may go away with rest or after removing shoes. The pain may be burning, stabbing or tingling, or may feel like an electric shock, and may also radiate to the back of the foot, causing cramps. Some patients also experience numbness between their toes. Common causes of Morton's neuroma are:
- wearing tight shoes
- wearing high heels
- joint inflammation
- thickening of the foot ligaments
- injuries to the front of the legs, for example from sports
- lipomas are lumps under the skin that contain excessive growth of fat cells
Tarsal tunnel syndrome
Tarsal tunnel syndrome (tarsal tunnel syndrome) causes foot pain due to compression of the posterior tibial nerve, which runs down the back of the leg, or the plantar nerves in the feet. Doctors don't know how common this condition is because it is often underdiagnosed. The syndrome is more common in women.
Symptoms of tarsal tunnel syndrome:
- sharp, shooting pain in the inner ankle and along the foot
- numbness on the underside of the foot
- pain when bending and moving the foot
- tingling or burning sensation
Symptoms may be worse at night, when walking or standing, or after exercise. The pain often improves with rest.
Tarsal tunnel syndrome can occur as a result of:
- wearing ill-fitting shoes
- leg injuries
- development of postoperative scars
- varicose veins
- ganglion cyst
- lipomas
Peripheral neuropathy
Peripheral neuropathy
is a general term for numbness, tingling, and burning in the toes, feet, and fingers. Symptoms may worsen at night. In addition, peripheral neuropathy can cause nonspecific symptoms that make it difficult to move your legs and perform basic activities. Researchers do not fully understand why some people develop peripheral neuropathy and others do not. However, scientists have identified conditions that increase the likelihood of developing peripheral neuropathy. These conditions include:
- infections
- deficiency of nutrients such as B12
- alcohol consumption
- diabetes
- some inherited diseases, such as Charcot-Marie-Tooth disease, which causes loss of muscle tissue
- Guillain-Barré syndrome, a condition that causes rapid muscle weakness
Diabetic neuropathy
Both type 1 and type 2 diabetes can cause neuralgia in the toes and feet. Diabetic neuropathy affects more than 90% of people with diabetes. Typically, nerve pain first affects the toes and surrounding areas and can then slowly spread to the rest of the foot and up the legs.
Symptoms of diabetic neuropathy include:
- tingling, burning, sharp or shooting pain in the toes or feet
- electric shock sensation in these areas
- pain that usually gets worse at night, causing sleep disturbances
- pain when touching the skin
Scientists are not sure of the exact reasons. Some theories point to changes in the blood vessels, metabolism, immune system, or the body's sodium and calcium channels. Some factors increase the risk of developing neuropathy:
- elderly age
- having diabetes for a longer period
- alcohol consumption
- use of tobacco products
Sciatica
Sciatica occurs when the sciatic nerve, the longest and widest nerve, is damaged or compressed. The sciatic nerve runs from the lower back, through the buttocks and down the legs, ending just below the knee. The most common cause of sciatica is a herniated or bulging disc in the spine. While sciatica tends to affect the back, hips, and upper legs first, the pain can spread down the legs to the feet and toes. Symptoms of sciatica include:
- back pain on one side
- pain or burning in the buttocks
- weakness in legs
- leg and foot pain