A cerebral pituitary adenoma (PPA) is a tumor of the glandular tissue of the brain appendage. The pituitary gland is a significant endocrine gland in the human body, located in the lower part of the brain in the pituitary fossa of the sella turcica. This small organ of the endocrine system, weighing only 0.7 g in an adult, is responsible for its own production of hormones and control over the synthesis of hormones by the thyroid and parathyroid glands, and the genitourinary organs. The pituitary gland is involved in the regulation of water-fat metabolism, is responsible for a person’s height and weight, the development and functioning of internal organs, the onset of labor and lactation, the formation of the reproductive system, etc. It is not for nothing that doctors call this gland a “virtuoso conductor”, controlling the sound of a large orchestra, where the orchestra is our whole organism.
Schematic representation of the location of the tumor.
But, unfortunately, this unique organ, without which a harmonious functional balance in the body is impossible, is not protected from pathological formations or diseases due to hormonal and/or neurogenic disorders. One of the serious diseases is adenoma, in which the glandular, hormonally active epithelium of the pituitary gland of the brain grows pathologically, which can cause disability for the patient.
Anatomy.
Adenomas can be active (AAG) or inactive (NAG). In the first case, the hormonal balance suffers from an excess of secreted pituitary hormones. In the second, the tumor mass irritates, compresses nearby tissues, and the optic nerve is often affected. It is worth noting that greatly increased proportions of the active pathological focus also negatively affect the intracranial tissues located nearby. We suggest you learn about other features of the pathology, including the specifics of treatment, from the article.
Epidemiology: causes, incidence rates
The factor that stimulates the development of a pituitary tumor has not yet been identified, and therefore remains the main subject of research. Experts only voice versions of the probable causes:
- traumatic brain injuries;
- neuroinfection of the brain;
- bad habits;
- pregnancy 3 or more times;
- heredity;
- taking hormonal medications (for example, contraceptives);
- chronic stress;
- arterial hypertension, etc.
The neoplasm is not so rare; in the general structure of brain tumors it accounts for 12.3%-20% of cases. In terms of frequency of occurrence, it ranks 3rd among neuroectodermal neoplasias, second only to glial tumors and meningiomas. The disease is usually benign in nature. However, medical statistics record data on isolated cases of malignant transformation of adenoma with the formation of secondary foci (metastases) in the brain.
The pathological process is more often diagnosed in women (about 2 times more) than in men. Below we present data on the age distribution based on 100% of patients with a clinically confirmed diagnosis. The epidemiological peak occurs at the age of 35-40 years (up to 40%), at 30-35 years the disease is detected in 25% of patients, at 40-50 years - in 25%, 18-35 and over 50 years - 5% each age category.
According to statistics, about 40% of patients have an inactive tumor, which does not secrete excess hormonal substances and does not affect endocrine balance. In approximately 60% of patients, an active formation is identified, characterized by hypersecretion of hormones. About 30% of people become disabled due to the consequences of an aggressive pituitary adenoma.
Indications and contraindications for MRI of the pituitary gland
Please note that MRI of the pituitary gland is not included in MRI of the brain, as it requires a different approach.
It is indicated for patients who have been diagnosed with endocrine disorders of unknown cause, presumably related to the hypothalamic-pituitary system:
- increased levels of pituitary hormones in the blood;
- serious disruption of the menstrual cycle;
- significant deviation from normal height and weight;
- functional disruptions in the functioning of other endocrine glands.
This study is also indicated for:
- suspicion of the presence of a neoplasm in the hypothalamic-pituitary region;
- postoperative observation;
- assessing the effectiveness of conservative treatment of a previously diagnosed tumor.
Contraindications may be absolute - the procedure cannot be performed:
- the body contains metal structures made of ferromagnets that cannot be removed;
- the presence of electronic devices such as a pacemaker, insulin pump, cochlear implant and others;
- inability to maintain a still position during the procedure (claustrophobia, severe pain, unstable mental state);
- pregnancy in the first trimester.
Relative contraindications, when the question of the possibility of performing MRI is decided individually, are:
- childhood;
- weight more than 130 kg;
- the presence of foreign bodies and implants in the area under study.
In addition, there are contraindications for the use of contrast agents:
- pregnancy at any stage;
- renal failure;
- uncompensated diabetes mellitus;
- allergic reactions to contrast in the past.
If a patient is diagnosed with bronchial asthma, the question of the possibility of using contrast is decided individually.
Classification of pituitary adenomas of the brain
The pituitary focus is formed in the anterior lobe of the gland (adenohypophysis), which makes up the bulk of the organ (70%). The disease develops when one cell mutates; as a result, it escapes immune surveillance and falls out of the physiological rhythm. Subsequently, through repeated division of the progenitor cell, an abnormal proliferation is formed, consisting of a group of identical (monoclonal) cells. This is an adenoma; this is the most common development mechanism. However, in rare cases, the lesion may initially originate from one cell clone, and after relapse, from another.
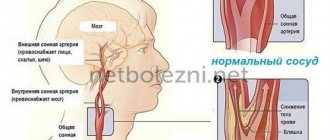
Pathological formations are distinguished by activity, size, histology, nature of distribution, type of secreted hormones. We have already found out what type of activity adenomas have - hormonally active and hormonally inactive. The growth of defective tissue is characterized by an aggressiveness parameter: a tumor can be non-aggressive (small and not prone to growth) and aggressive when it reaches large sizes and invades neighboring structures (arteries, veins, nerve branches, etc.).
Large adenoma after removal.
Based on the size of pituitary adenomas, there are the following types:
- microadenomas (less than 1 cm in diameter);
- mesoadenomas (1-3 cm);
- large (3-6 cm);
- giant adenomas (more than 6 cm in size).
According to their distribution, AGGM are divided into:
- endosellar (within the pituitary fossa);
- endoextrasellar (extending beyond the sella landmarks), which extend:
► suprasellar – into the cranial cavity;
► laterosellar – into the cavernous sinus or under the dura mater;
► infrasellar – grow down towards the sphenoid sinus/nasopharynx;
► antesellar – affect the ethmoidal labyrinth and/or orbit;
► retrosellar – into the posterior cranial fossa and/or under Blumenbach’s clivus.
According to histological characteristics, adenomas are given names:
- chromophobe - neoplasia formed by pale, poorly contoured adenohypophyseal chromophobe cells (a common type, represented by NAG);
- acidophilic (eosinophilic) – tumors created by alpha cells with a well-developed synthetic apparatus;
- basophilic (mucoid) – neoplastic formations developing from basophilic (beta cells) adenocytes (the rarest tumor).
Among hormonally active adenomas there are:
- prolactinomas – actively secrete prolactin (the most common type);
- somatotropinomas – produce growth hormone in excess; corticotropinomas – stimulate the production of adrenocorticotropin;
- gonadotropinomas – enhance the synthesis of human chorionic gonadotropin;
- thyrotropinomas – produce a large release of TSH, or thyroid-stimulating hormone;
- combined (polyhormonal) – secrete 2 or more hormones.
How to identify
Symptoms of a pituitary cyst are nonspecific and it is impossible to determine the presence of a neoplasm from them. Most often, patients complain of headaches resembling hemicrania (migraine), when the pain is localized on one side of the head.
Migraine is not associated with physical activity, overwork, or lack of sleep. Cephalgia appears suddenly, even against the background of complete well-being. The accuracy of vision gradually decreases, and the lateral fields of vision may fall out. Large cysts can lead to complete loss of vision. Decreased vision or loss of visual fields is caused by the anatomical proximity of the optic nerve and the pituitary gland.
A pituitary cyst is accompanied by other nonspecific symptoms:
- Sleep disturbance, irritability, emotional lability, anxiety, fatigue when performing simple work.
- Dizziness, tinnitus.
- Autonomic disorders: shortness of breath, hyperhidrosis, loss of appetite, diarrhea or diarrhea, feeling of strong heartbeat and interruptions in its rhythm.
Sometimes patients complain of fever. However, temperature and a cyst in the pituitary gland are unrelated symptoms.
Rathke's pouch cyst, for example, is asymptomatic throughout life. It is usually found during a post-mortem autopsy. The first symptoms of a pouch cyst appear when the size of the cyst increases. Thus, 70% of patients report severe headaches, 50% of patients complain of decreased visual accuracy.
Rathke's cyst may be accompanied by endocrinological symptoms:
- Hypopituitarism is damage to pituitary tissue with subsequent loss of gland function and failure of peripheral endocrine organs. In other words, with this pathology the amount of hormones released decreases.
- Hyperprolactinemia is an increase in prolactin in the blood plasma. The pathology is accompanied by reproductive dysfunction, psychological personality changes, sexual and metabolic disorders.
- Water and electrolyte disturbances. Swelling forms, disruptions in the functioning of the heart appear, its work increases or slows down, muscle spasms, drowsiness or lethargy occur.
Rathke's disease can become malignant, that is, acquire the characteristics of a malignant tumor. This leads to increased intracranial pressure, bilateral blindness and often to the development of diabetes insipidus.
Clinical manifestations of the tumor
Many symptoms, as they themselves emphasize, are not taken seriously by patients at first. Ailments are often associated with banal overwork or, for example, stress. Indeed, manifestations can be nonspecific and veiled for a long time - 2-3 years or more. Note that the nature and intensity of symptoms depend on the degree of aggression, type, location, volume and many other characteristics of the adenoma. The neoplasm clinic consists of 3 symptomatic groups.
- Neurological signs:
- headache (most patients experience it);
- impaired innervation of the eye muscles, which causes oculomotor disorders;
- pain along the branches of the trigeminal nerve;
- symptoms of hypothalmic syndrome (VSD reactions, mental imbalance, memory problems, fixation amnesia, insomnia, impaired volitional activity, etc.);
- manifestations of occlusive-hydrocephalic syndrome as a result of blockade of the outflow of cerebrospinal fluid at the level of the interventricular foramen (impaired consciousness, sleep, headache attacks when moving the head, etc.).
- Ophthalmological symptoms of the neural type:
- noticeable discrepancy in visual acuity of one eye from the other;
- gradual loss of vision;
- disappearance of the upper fields of perception in both eyes;
- loss of the visual field of the nasal or temporal areas;
- atrophic changes in the fundus (determined by an ophthalmologist).
- Endocrine manifestations depending on hormone production:
- hyperprolactinemia - discharge of colostrum from the breast, amenorrhea, oligomenorrhea, infertility, polycystic ovary syndrome, endometriosis, decreased libido, hair growth, spontaneous abortions, problems with potency in men, gynecomastia, low quality sperm for conception, etc.;
- hypersomatotropism - an increase in the size of the distal limbs, brow ridges, nose, lower jaw, cheekbones or internal organs, hoarseness and deepening of the voice, muscle dystrophy, trophic changes in the joints, myalgia, gigantism, obesity, etc.;
- Itsenko-Cushing syndrome (hypercortisolism) - dysplastic obesity, dermatoses, osteoporosis of bones, fractures of the spine and ribs, dysfunction of the reproductive organs, hypertension, pyelonephritis, stretch marks, immunodeficiency states, encephalopathy;
- symptoms of hyperthyroidism - increased irritability, restless sleep, changeable mood and anxiety, weight loss, trembling hands, hyperhidrosis, irregular heart rhythm, high appetite, intestinal disorders.
Approximately 50% of people develop symptomatic (secondary) diabetes as a result of a pituitary adenoma. 56% are diagnosed with loss of visual function. To one degree or another, almost everyone experiences symptoms classic for pituitary hyperplasia of the brain: headache (more than 80%), psycho-emotional, metabolic, cardiovascular disorders.
Symptoms
As a rule, cystic formation is not accompanied by severe symptoms. Manifestations disturbing the patient were recorded only in 6% of all cases. They appear when the diameter of the tumor exceeds ten centimeters.
The most common signs of the disease:
- Headache attacks;
- Frequent dizziness;
- Impaired visual abilities: blurred vision, complicated movement of the eyeballs, blurred vision;
- Burning, cutting pain in the eyes;
- General deterioration in health.
In addition to the manifestations described above, a neoplasm in the pituitary gland may be accompanied by the development of the following pathologies:
- Diabetes insipidus;
- Disturbances in the functioning of the organs of the reproductive system;
- Hypothyroidism;
- Adrenal insufficiency.
Methods for diagnosing pathology
Specialists adhere to a unified diagnostic scheme if a person suspects this diagnosis, which includes:
- examination by a neurologist, endocrinologist, ophthalmologist, ENT doctor;
- carrying out laboratory tests - general blood and urine tests, blood biochemistry, blood tests for sugar and hormone concentrations (prolactin, IGF-1, corticotropin, TSH-T3-T4, hydrocortisone, female/male sex hormones);
- heart examination using an ECG machine, ultrasound of internal organs;
- ultrasound examination of the vessels of the veins of the lower extremities;
- X-ray of the skull bones (craniography);
- computed tomography of the brain, in some cases there is an additional need for MRI.
MRI.
Note that the specificity of collecting and studying biological material for hormones is that conclusions are not drawn after the first examination. To ensure the reliability of the hormonal picture, dynamic observation is necessary, that is, you will need to donate blood for research repeatedly at certain intervals.
What are the possible complications?
hydrocephalus of the brain;
- violation of intracranial pressure;
- complete loss of vision;
- hemorrhage into the cyst;
- development of pituitary adenoma;
- degeneration into a malignant neoplasm.
To prevent the serious consequences of pituitary cysts, it is necessary to control any changes in hormonal levels. Protect your head from mechanical stress and injury. Be examined by a neurologist at least once a year.
Avoid professional activities with toxic substances and exposure to radiation. It is necessary to stop smoking and drinking alcohol. Avoid heavy physical activity.
Review your diet and use more low-carb foods. In this way, you can maintain the health and normal functioning of the brain.
A developing disease - a pituitary cyst - has an extremely negative impact on all neighboring tissues of the pituitary gland and the development of complications in the centers that are located here. The most dangerous of them are: hydrocephalus, increased intracranial pressure, development of blindness, and various types of bleeding.
Principles of disease treatment
Let’s make a reservation right away: with this diagnosis, the patient needs highly qualified medical care and constant monitoring. Therefore, there is no need to rely on chance, believing that the tumor will resolve and everything will pass. The outbreak cannot go away on its own! In the absence of adequate therapy, the danger of becoming disabled with irreversible functional impairment is too great, and deaths from the consequences also occur.
Depending on the severity of the clinical picture, patients are recommended to solve the problem surgically and/or conservative methods. Basic therapy procedures include:
- neurosurgery
- removal of adenoma by transnasal access (through the nose) under endoscopic control or transcranial method (standard craniotomy is performed in the frontal part) under the control of a fluoroscope and microscope;
90% of patients are operated on transnasally, 10% require transcranial ectomy. The latter tactic is used for massive tumors (more than 3 cm), asymmetric growth of newly formed tissue, extension of the lesion beyond the sella, and tumors with secondary nodes.
- treatment with medications
- the use of drugs from a number of dopamine receptor agonists, peptide-containing agents, targeted drugs for hormone correction; - radiotherapy (radiation treatment)
– proton therapy, remote gamma therapy using the Gamma Knife system; - Combination treatment
– the program course combines several of these therapeutic tactics.
The doctor may not use surgery, but recommend observation of a person diagnosed with pituitary adenoma in the absence of focal neurological and ophthalmological disorders and the tumor is hormonally inactive. Such a patient is managed by a neurosurgeon in close collaboration with an endocrinologist and an ophthalmologist. The patient is systematically examined (1-2 times a year), sent for MRI/CT, eye and neurological examinations, and measurement of hormones in the blood. In parallel with this, the person undergoes courses of targeted maintenance therapy.
Since surgery is the leading method of treating pituitary adenoma, we will briefly highlight the course of the surgical process of endoscopic surgery.
How reliable is MRI?
There is not a single characteristic MRI sign that could be used for a reliable differential diagnosis of Rathke's pouch cysts and other cystic formations of the sellar or suprasellar region. Simple cysts may be indistinguishable from arachnoid or epidermoid cysts. More complex ones may be difficult to distinguish from craniopharyngiomas or pituitary adenomas.
Cystic pituitary adenomas may resemble the former in the absence of a solid contrast-enhancing component on MRI. Features such as the presence of a fluid-liquid level, a hypointense rim on T2-weighted images, internal septa, and a location lateral to the midline are more often consistent with pituitary adenomas, while the presence of an intracystic nodule may be more often associated with the research topic.
Due to the significant variability in CT and MRI findings, preoperative diagnosis requires a combination of clinical, biochemical, and radiographic findings. Differential diagnosis is very important because the treatment and surgical approach differ significantly from those for other possible pathologies. If you are in doubt about the diagnosis, you can get a second opinion with an MRI of the pituitary gland.
Transnasal surgery to remove pituitary adenoma of the brain
This is a minimally invasive procedure that does not require a craniotomy and does not leave behind any cosmetic defects. It is most often performed under local anesthesia; the surgeon’s main instrument will be an endoscope. A neurosurgeon removes a brain tumor through the nose using an optical device. How is all this done?
- The patient is in a sitting or semi-sitting position during the procedure. A thin endoscope tube (no more than 4 mm in diameter), equipped with a video camera at the end, is carefully inserted into the nasal cavity.
- The real-time image of the lesion and adjacent structures will be transmitted to the intraoperative monitor. As the endoscopic probe advances, the surgeon performs a series of sequential manipulations to get to the part of the brain of interest.
- First, the nasal mucosa is separated to expose and open the anterior wall. The thin bony septum is then cut. Behind it is the desired element - the sella turcica. A small hole is made in the bottom of the sella turcica by separating a small fragment of the bone.
- Next, using microsurgical instruments placed in the channel of the endoscope tube, pathological tissues are gradually chipped off through the access created by the surgeon until the tumor is completely eliminated.
- At the final stage, the hole created in the bottom of the saddle is covered with a bone fragment, which is fixed with special glue. The nasal passages are thoroughly treated with antiseptics, but not tamponed.
The patient is activated in the early period – already on the first day after low-traumatic neurosurgery. About 3-4 days later, you will be discharged from the hospital; then you will need to undergo a special rehabilitation course (antibiotic therapy, physiotherapy, etc.). Despite undergoing surgery to excise a pituitary adenoma, some patients will be asked to additionally adhere to hormone replacement therapy.
The risks of intra- and postoperative complications during the endoscopic procedure are reduced to a minimum – 1%-2%. For comparison, negative reactions of various types after transcranial resection of AGGM occur in approximately 6-10 people. out of 100 operated patients.
After a transnasal session, most people experience difficulty in nasal breathing and discomfort in the nasopharynx for some time. The reason is the necessary intraoperative destruction of individual structures of the nose, resulting in painful symptoms. Discomfort in the nasopharyngeal area is usually not regarded as a complication if it does not intensify and does not last long (up to 1-1.5 months).
The final assessment of the effect of the operation is possible only after 6 months using MRI images and the results of hormonal tests. In general, with timely and correct diagnosis and surgical intervention, high-quality rehabilitation, the prognosis is favorable.