What is neurosis
Many people know about neurosis firsthand and have experienced this painful state more than once.
Stress and overwork can cause this negative state, which suppresses all desire to live, be active, and work. The person becomes either too lethargic or irritable. Neurosis is also characterized by severe fatigue, which can manifest itself without obvious reasons. Neurosis is a disease that affects the nervous system. Sometimes it is not visible from the outside, and the patient may appear to be completely healthy. But in fact, at the same time, he may feel fear, panic, irritation, a desire to cry, which may be absolutely independent of external factors. Sometimes neurosis does not manifest itself due to stress or depression, or extreme fatigue at work. Symptoms may appear for other reasons, which lie in physical diseases of the internal organs. Also, neurotic conditions are often suffered by people who have experienced a nervous breakdown or suffered from thyroid diseases at least once in their lives. Neurosis-like conditions do not arise from stress, as experts believe, unlike ordinary neuroses. And psychological factors do not play a special role here. Many believe that the problem lies elsewhere.
Types of neurosis-like conditions
Asthenic syndrome.
This is one of the most common neurosis-like conditions that a person can experience. It does not appear immediately; it develops gradually, increasing and worsening the patient’s well-being. At first, you may experience severe fatigue and a constant desire to lie down, sit down, and rest after minimal exertion. At the same time, emotional instability manifests itself when a person himself cannot control his emotions. After strong irritability comes an apathetic state when you don’t want anything and don’t need anything. A person may distort reality and have an incorrect assessment of current events. Such people have a very difficult time tolerating too bright stimuli, such as strong light, loud sound and unpleasant smell. At night I don’t want to sleep, but during the day I constantly feel sleepy. Even physical aspects such as heart pain and headaches can manifest themselves. Inside there is a feeling of constant anxiety and expectation of bad things, although no real factor contributes to this. All these manifestations become especially aggravated during sudden changes in weather and season.
Obsessive-compulsive syndrome.
It manifests itself as obsessive thoughts, movements, unreasonable fears, which are difficult to get rid of, even thinking logically. At the same time, the patient understands everything and can evaluate his condition as strange and stupid, but physically he cannot cope with it. Some people with a strong will can, by constantly controlling themselves, get rid of obsessive states. But this may not last long, since without proper treatment of the nervous system, everything can come back again. Such conditions are precursors to depression, neuroses and various psychopathic diseases.
Hysterical syndrome.
A person with such a syndrome will behave brightly, and sometimes even too defiantly. He will play to the public, express his emotions and behave demonstratively, drawing considerable attention to himself. His gestures are broad and attention-grabbing. Emotions may include loud laughter, crying, exclamations, and even fainting. In fact, such manifestations have nothing to do with real hysteria, when a person cannot control himself. In fact, this is just an imitation of a seizure. Unfortunately, this syndrome is not very harmless: as a result of these manifestations, deafness and blindness, as well as paralysis, can even develop.
Hypochondriacal syndrome.
The patient may be completely healthy and have no problems other than with the nervous system. And at the same time, he will constantly fear for his well-being, listen anxiously to himself and not find peace during the day, worrying about the slightest pain or unpleasant sensation in the body. At the same time, he is very suspicious and invents many diseases for himself. Most often, such people spend days in hospital queues, visiting all kinds of specialists in order to identify at least one far-fetched ailment. They undergo diagnostics, undergo consultations and constantly complain about their health, although there may be no real reasons for this.
Diagnosis and classification of TR
The first task that must be solved when diagnosing TD is to distinguish anxiety as a normal and proactive response to threatening or stressful influences from the manifestation of TD. Anxiety performs an adaptive signaling function (“signal alarm”) to prepare at the organism level to encounter danger and select a reaction to it: “attack, fight” or “escape, avoidance.” Normally, manifestations of anxiety are short-term (transient) in nature and are well under the control of the individual.
Manifestations of anxiety acquire clinical significance in cases where:
their severity and duration become significant;
symptoms occur in the absence of stress factors;
symptoms disrupt the physical (somatic) and socio-psychological functioning and adaptation of the individual.
The presence of TD is indicated by the fact that the child experiences anxiety more often (for example, on most days of the month and for several months) and experiences it more intensely compared to peers. Excessive anxiety leads to significant disruptions and limitations in a child's life: it is difficult for him to participate in normal activities for his age, attend school, cope with daily school and homework, socialize and make friends, and attend leisure activities and sports clubs. Table 1 presents the differences between anxiety and fears that are acceptable during the individual development of children and their pathological manifestations.
All forms of TR are accompanied by changes at four levels.
Emotions: fear, apprehension, embarrassment, shame, helplessness, guilt, sadness, anger.
Thoughts: about possible harm/danger/damage that cannot be dealt with on your own, negative thoughts of an obsessive nature.
Behavior: choice of avoidance strategy (active avoidance of specific situations, places or stimuli, its erased manifestations in the form of uncertainty, indecision, desire for loneliness) and the use of so-called “safety techniques” (recourse to objects and situations that do not allow the development of extremely pronounced fear, with the formation of “rituals”). There may be repeated appeals to adults for comfort and support, and excessive apologies to other people.
Sensations (physiological level): due to an imbalance of autonomic regulation - rapid heartbeat, rapid breathing, increased sweating, headache, dizziness, feeling of lack of air and approaching fainting, cramps and pain in the abdomen, nausea, vomiting, diarrhea, paresthesia (tingling, numbness) in the face or hands, a feeling of unsteadiness or weakness in the legs, a tendency to tremble or tremors, sleep disturbances (difficulty falling asleep, restless sleep, nightmares, insomnia).
One of the key signs of TD is fear, but it should not be equated with anxiety. Anxiety is a combination of emotions, and fear is one of the emotions. Fear, as a normal emotion, is a reaction to an external threat and is adaptive in nature; it warns the individual that the situation may be physically or psychologically dangerous. Fears are characterized by normal age-related evolution (Table 2). Moreover, they can be of a realistic nature (in relation to specific animals, bodily injuries, natural phenomena) and unrealistic, irrational (fear of the dark, mice, monsters, disasters).
Thus, fears as an isolated phenomenon should not be considered as a sign of illness. The help of a specialist is necessary in cases where fears lead to obvious social restrictions: refusal to go outside for fear of meeting a dog or experiencing a panic attack, refusal to attend school.
In the clinical picture of TD, fears are characterized by a stable and non-adaptive nature [9]:
excessive intensity that does not correspond to the situation (quantitative aspect);
unusual content and unusualness of objects that cause fear (qualitative aspect);
inadequate response to the situation;
chronic fear;
inability to reduce or overcome fear;
significant restrictions in everyday life.
Ultimately, manifestations of TD affect all areas of life, significantly worsening the child’s general well-being, school performance, family relationships and friendly contacts, and social activity.
TR include [1, 2]:
TD associated with separation in childhood (separation TD);
selective mutism;
phobic TD of childhood (specific phobias);
social TD of childhood;
generalized TR of childhood;
panic disorder;
agoraphobia.
Two other disorders that were previously classified as TD are obsessive-compulsive disorder and post-traumatic stress disorder. In modern classifications [1, 2], they are considered as separate nosological forms.
Separation TR
Some children experience fear and painful apprehension because, with a real or imagined threat of separation, something bad will happen to them or their loved ones (most often to their parents). The child strives to avoid separation, experiences excessive fear, sadness, and withdraws into himself. On the other hand, there are attacks of rage, crying with the desire to keep a loved one nearby, clinging to him and a categorical refusal to part. The child refuses to be in situations where he may find himself without loved ones: staying away from home at night, visiting friends or relatives, being at home alone, or going to school without parents. After suffering separation from loved ones, children remain depressed, withdrawn and apathetic. They refuse to be alone in the room and ask parents to be present or available.
Separation anxiety usually goes away as children grow up, go to school, and gain confidence. However, for some children, their reaction to actual or expected separation continues to be excessive, which can sometimes continue into the first 1–2 years of school and even beyond. Manifestations of separation anxiety disorder can impede or limit the child’s normal activity, lead to deterioration in school attendance and academic performance, and isolation from peers because he avoids participating in school outings, excursions, games, overnight trips without parents, or other activities. Such children differ from their peers in their lack of independence.
Separation-related TD is most common in children under 12 years of age and decreases in incidence during adolescence. This type of TD affects about 4% of children and 1.5% of adolescents [1, 3, 4]. However, separation anxiety can persist into adulthood.
The occurrence of separation TD reaches its peak in several age periods: upon entering kindergarten, in elementary school at the age of 7 to 9 years, upon entering middle and high school. Boys and girls suffer from separation TD equally often. During adolescence, separation anxiety either persists or arises for the first time (after a stressful event, such as parental divorce, loss of a loved one, moving to a new school, moving).
Selective mutism
Selective mutism —
one of the forms of TD in children, which in some cases has to be differentiated with alalia (developmental dysphasia). Manifests at the age of 2–5 years. The prevalence in the pediatric population is less than 1% [1, 10]. More often, selective mutism occurs in families with bilingualism, when moving to a new place of residence with a different language environment. It occurs during the period of active speech development or upon entering kindergarten, in preparation for school. Selective mutism limits communication capabilities, can distort the child’s mental development, and complicates his social adaptation.
The child stops talking to everyone except a small circle of familiar people. This continues for a long time, up to several months. Despite the preservation of speech, the child consciously refuses verbal communication (and sometimes any communication) in situations that are psychologically traumatic for him (both in a group of children and among adults). At the same time, he not only refuses to speak - he is unable to do so because of the feeling that his speech seems to freeze in the larynx. Gradually, the child learns to anticipate situations that provoke mutism and tries to avoid them.
An important feature is that the majority of patients with selective mutism have manifestations of social TD, and at an early age - separation TD [10]. A number of patients experience a combination of selective mutism with disorders such as speech development disorders, enuresis, encopresis, delayed motor development, autism, and in rare cases, attention deficit hyperactivity disorder. Selective mutism is not currently considered within the framework of oppositional behavior, but oppositional reactions may occur if the child is forced to speak.
Although the first symptoms of selective mutism appear before the age of 5, they may become most noticeable once school starts. Selective mutism causes significant difficulties in children's lives, affecting their academic performance, preventing them from seeking help from teachers and other adults, and preventing them from enjoying social interactions and participating in daily activities with their peers. In older children and adolescents, difficulties in communicating with peers often increase, which serves as a prerequisite for the formation of social and generalized TD or depression.
Specific phobias
Fears are common and expected in childhood, but for some children and adolescents, fears become intense over time and develop into phobias. A phobia is a strong fear that is disproportionate to a specific object or situation, extremely severe anxiety in the absence of immediate danger. Intense fear of certain situations and objects is accompanied by an avoidance response due to the belief that they are dangerous and will cause harm/injury. The most common pathological fears in children are caused by: animals (dogs and birds), insects and spiders, darkness, loud noises (especially those associated with natural phenomena), clowns, people in masks or unusual appearance, injections, diseases, the sight of blood.
Specific phobias manifest from early age to 10 years; they affect 6–9% of children and adolescents, more often girls than boys (in a ratio of 2:1) [1, 3, 4].
Some patients develop a phobia after exposure to a traumatic or frightening event, while others develop fears after observing other people's anxious reactions. Thus, a younger brother often begins to be afraid of a spider if he witnesses how the older brother runs away from the spider in fear and screaming. Phobias are different from ordinary childhood fears and rarely go away on their own. Often, phobias do not decrease, despite explanations and assurances of safety from adults. As a result, the child avoids frightening places or objects, forces parents to check if they are nearby (for example, before going to bed he wants to make sure that there are no spiders in the room), requires parents to stay nearby.
Children avoid parks, playgrounds, recreation areas and other places where there may be insects, refuse walks and nature excursions if they may encounter what they consider dangerous animals (for example, dogs), and protest against visiting medical institutions or doctors. , in particular dentists. As children grow older, phobias do not disappear, but change in content. But teenagers are more likely than younger children to recognize that their fear is disproportionate to the actual danger posed by a particular object or situation. In addition, unlike young children, who have less control over themselves in everyday life, adolescents can independently avoid certain situations and direct confrontations with their fears.
School-age children may experience a fear of school, which manifests itself in the same way as a phobia, and they refuse to attend. In this regard, the term “school phobia” appeared, although as such there is no diagnosis or form of TD with this name. The range of manifestations of school fears can vary from minor complaints about the need to attend classes to hysterics and refusal to go to school in young children, and in adolescents - to frequent absences from classes with subsequent exclusion from school. Children may be afraid of school for many reasons, for example, because they have to be left without parents (as happens with separation anxiety disorder), because of fear of contact with germs (with obsessive-compulsive disorder), because of fear of interactions with peers and teachers (with social TD). In these cases, the child or teenager is actually afraid not of the school itself, but of the events that could happen to them there. Because of this, the term “school phobia” is not accurate.
On the other hand, the causes of school phobia may be difficulties in adapting to the classroom, fear of bad grades, fear of making a mistake or getting reprimanded by the teacher, conflicts with classmates, fear of physical aggression on their part. Some parents, without noticing it themselves, instill in their children a fear of school by overly dramatizing learning problems; they deprive the child of the opportunity to show initiative and independence - they do homework for him or strictly control them, resenting every clumsily written letter. As a result, the child is not so much afraid of school as he is afraid of not meeting the high expectations of his parents. Any of these problems can make a child's school life unbearable. In such cases, not only parents, but also teachers should help him cope with this situation.
Social TR
Social TD manifests itself as intense, accompanied by an avoidance reaction, fear of situations related to social contacts, any forms of behavior in public places, when the child/adolescent thinks that he will do something wrong and will cause a negative assessment and ridicule from others. Such situations include public speaking, answering lessons in front of the class, taking exams, meeting new peers, parties, playing sports, conversations with elders or leaders, including teachers at school, when the child is the center of attention. Some children are only afraid of speaking or performing in public, while others are afraid and avoid a wider range of social situations.
Social TD is observed in 2–7% of children and adolescents, equally often in boys and girls, manifests itself at 7–13 years of age, more often in early adolescence, but can also manifest itself in elementary school [1, 3, 4]. Social TD appears suddenly after suffering stress or develops gradually over time.
Problems associated with social TD: passivity in class (cannot ask questions and answer clearly, read aloud, write on the board, express and defend opinions), poor academic performance, low self-esteem and uncertainty in social situations, difficulties in establishing and maintaining friendships, refusal to go to group events (birthdays, parties). The child cannot eat in the presence of others or use a public toilet. Children become overly shy and often expect things to go wrong when they are surrounded by other children. However, they may be concerned that others are watching them and discussing their behavior.
Social TD goes unnoticed by teachers and parents for a long time, because such children do not want to remain in the public eye and try to be invisible. Therefore, they are only noticed when they start skipping school or getting bad grades.
Adolescents and young adults with social TD are even more self-focused and have low self-esteem. When they start working, due to extreme fear or embarrassment, they may feel awkward when making acquaintances, interacting with colleagues, or interviewing management. They have an increased risk of depression, alcohol or drug use.
Generalized TR
Generalized TD is manifested by excessive anxiety with anticipation of an unfavorable development of a variety of events and circumstances related to the family, the state of one’s own health and those of loved ones, financial situation, friends, school, as well as everyday affairs. A child in such a situation is characterized by a constant search for support from parents and other people in connection with his own fears, avoidance of everything new, especially negative news, uncertain situations, and the possibility of making a mistake. It is also typical to have somatic symptoms, insomnia, irritability, muscle tension, and difficulty concentrating during anxiety.
The manifestation of generalized TD occurs at the age of 10–12 years, it is observed in approximately 1% of adolescents, 2 times more often among girls than among boys [1, 3, 4]. If left untreated, the disease does not disappear until adulthood and leads to a significant deterioration in quality of life.
Patients with generalized TD experience persistent irrational and uncontrollable worry about various aspects of daily life and future events, including minor issues. Young children tend to worry about simple and immediate issues, such as family safety, love and affection from loved ones, and school success. Adolescents show concerns about the health and safety of themselves and their families, academic performance, friendships and relationships with other people, their own punctuality, their future, relationships between parents or family stability, world events (related to nature, climate, environment). environment, politics, crime), etc.
Since patients with generalized TD experience severe somatic symptoms of anxiety, fatigue, irritability, impaired concentration, muscle tension and sleep disturbances, exaggerated, physically debilitating constant and uncontrollable anxiety, this has an extremely negative impact on the quality of life of the child and his family. The behavior of a child in this state is characterized by excessive time spent on completing homework, repeated tedious thinking about situations, repeated and unreasonable compilation of lists, frequent checks (of the progress of current affairs, relationships, health status with the identification of possible illnesses), procrastination in completing tasks, painful focusing of interests on subject of concern. This creates a tense environment around the child, worsens friendships and family relationships due to constant fears and endless requests for support.
The negative impact of ongoing constant worry becomes more obvious the older the child gets. Parents, teachers, and other adults notice that the teenager is different from his peers, spends a lot of time doing tasks ineffectively, appears stressed and exhausted, and refuses to participate in recreational activities or spend time with friends out of fear of failure. Over time, constant anxiety and detachment from friends and common activities with them increase the feeling of one’s own inferiority and predispose to depression.
Panic disorder, agoraphobia
Panic disorder - repeated and developing unexpectedly, without connection with any reason or situation, attacks of extreme anxiety (panic), which quickly reach a peak, are accompanied by threatening, in the patient's opinion, somatic symptoms (chill-like trembling, shortness of breath, palpitations, pain or discomfort in the chest, dizziness, nausea, profuse sweating, numbness, paresthesia, feeling of powerlessness), fear of death or madness. A panic attack is a sudden outburst of intense fear and discomfort that peaks and subsides within a few minutes. Following a panic attack for at least one month, the patient experiences anxiety about the occurrence of new attacks, he is afraid that something irreparable will happen to him due to a panic attack (losing control of himself, going crazy, dying), changing his behavior, to avoid a repeat panic attack (for example, avoiding physical activity).
In addition to panic disorder, many children and adolescents may develop agoraphobia, although the two conditions can exist independently of each other. Agoraphobia is characterized by intense anxiety and fear of real or perceived situations that may trigger a panic attack, and avoidance of such situations. Children are frightened by being in places from which it is difficult to get out quickly: public transport, open spaces (markets, bridges, parking lots), closed spaces (shops, cinemas, theatres), queues or crowds of people, they are afraid of being alone outside the home. Fear is associated with places from which it is difficult to escape and where it is impossible to get quick help. Therefore, children avoid as much as possible places and situations in which panic attacks have previously occurred; indoors they try to take seats near the aisle or closer to the exit; they try to maintain contact with security staff; they carry medications with them; they wear loose clothing that does not restrict movement; and they avoid physical abuse. exercise, any activity that activates the body.
Most often, panic disorder and agoraphobia manifest in young adulthood, but sometimes at 13–15 years of age. They affect approximately 2% of adolescents, girls are 2 times more likely than boys [1, 3, 4].
Problems associated with panic disorder and agoraphobia include low self-esteem, decreased independence, poor performance and absenteeism at school, refusal to travel and travel, difficulties in relationships with peers and family members, fear of separation from parents, transitions from home to school, disorders sleep, risk of depression and alcohol or drug use.
Pathogenetic mechanisms of TR
Previously, the term “childhood neurosis” was used in relation to TD. However, this concept is not entirely correct, since it means that the child’s emotional difficulties stem from unconscious internal psychological conflicts [7]. According to modern concepts, the development of TD occurs through the interaction of biological, psychological and environmental factors [8]. Risk factors include parental anxiety, child temperament with a tendency to withdraw, traumatic/negative/stressful life events, and parenting style [8].
Since various childhood TDs often occur in familial cases, much attention is paid to the study of hereditary predisposition and genetic mechanisms of TD. Neurobiological mechanisms (heredity and early brain damage caused by perinatal pathology) can lead to dysfunction of a number of brain structures and neurotransmitter systems [4]. The GABAergic, noradrenergic and serotonergic systems are considered key in the pathophysiology of TR and the mechanisms of action of anxiolytic drugs. It is assumed that further study of the neurobiological mechanisms of TD, including the use of functional neuroimaging methods, will make it possible to clarify the fundamental mechanisms of anxiety, the role of dysfunction of various brain regions, and to substantiate rational approaches to the treatment of TD.
When assessing environmental factors, it should be taken into account that to ensure the vital functions of a child’s body, many nutrients are needed, among which vitamins, macro- and microelements play an important role. Increased anxiety, irritability, emotional lability and fatigue can signal the body about metabolic disorders due to a deficiency of vitamins (especially group B) and minerals (in particular, magnesium, zinc). It is known that an increased need for vitamins and minerals at the usual level of their intake occurs in children during periods of the most intensive growth, under the influence of significant physical or psycho-emotional stress, and various stressful situations. The need for these nutrients also increases significantly in children with TD. A deficiency of vitamins, macro- and microelements in the body can be associated not only with high costs, but also with their low content in consumed food products and water. Therefore, in the process of examining patients with TR, attention should be paid to the completeness of their nutrition, which is determined not only by the energy value of food and the balance of the diet in proteins, fats and carbohydrates, but also by the provision of vitamins, macro- and microelements.
Causes of neuroses
The causes of neuroses can manifest themselves in childhood, when a birth injury occurred or an illness suffered in infancy. There can be several reasons for the manifestation of neuroses:
- Diseases of the nerves and psyche. This could be epilepsy with periodic seizures, schizophrenia, etc. A patient with such health problems is constantly treated and monitored by his doctor.
- Pathologies of brain development. These may be congenital disorders or acquired due to injury.
- Chronic infectious diseases. They, like nothing else, expose the nervous system to constant attacks. After all, when there are disturbances in the body, all functions suffer, making a lot of effort to get rid of the constant irritant.
- Diseases of the heart, blood vessels, gastrointestinal tract.
- Early drinking and smoking in adolescence. Often those people who in childhood indulged in alcohol and smoked around the corners of the school then suffer throughout their lives from neurotic attacks and unstable states of the nervous system, since it was disrupted during its most important period of development.
Causes
The true causes of neurosis are still unknown. Previously, it was considered a disease caused by the fast pace of life and intellectual overload. It has now been proven that the determining factor in the development of the disorder is not the multiplicity of episodes and the strength of the traumatic factor, but its subjective significance for the person.
External situations that can provoke neurosis vary from person to person. They are determined by the patient's value system. Any situation under certain conditions can become the basis for the development of a neurotic disorder. What matters is not the stressful situation itself, but its incorrect assessment from the point of view of the destruction of personal well-being in the present or future.
Neuroses often develop in people with certain psychophysiological characteristics. The disorder most often develops in people with the following personality traits:
- increased suspiciousness;
- demonstrativeness;
- rigidity;
- emotionality;
- subdepression.
High emotional lability in women leads to a higher likelihood of developing neurosis twice as often as in men. Hereditary predisposition to this disease is due to the inheritance of certain personality traits. Hormonal changes in the body, such as puberty and menopause, increase the risk of developing neurosis.
Symptoms
The symptoms of all neurotic conditions and stable neuroses are very similar, since they all manifest themselves in a similar way.
This may be emotional instability, when the mood “jumps” from plus to minus and vice versa. It is always strange to observe this in adults, which indicates the presence of a problem that needs to be treated with medication. Manifestation of anxiety, when everything is outwardly good and calm, irritability towards surrounding people and circumstances indicate a disorder of the nervous system. It becomes difficult for adults to control not only their internal feelings, but even their behavior, as unjustified aggression increasingly begins to manifest itself and take its place in life. These include fears, suspiciousness about health, the desire to cry for no reason. Physical symptoms include problems with the intestinal tract, constipation and diarrhea with a normal healthy diet. Reluctance to eat food, insomnia during night rest, daytime apathy and lethargy, vomiting, changes in pulse and blood pressure disturbances may also occur. It is not necessary to have all of these symptoms for a clear diagnosis to be made. It is enough to have several in intense manifestation.
Complex of reasons
Neurosis-like syndrome often appears in childhood. The cause may be prenatal developmental disorders, illnesses and injuries suffered at an early age. When the disease appears at a later age, the reasons may be different.
The most common are the following:
- the presence of mental and neurological diseases (schizophrenia, epilepsy, etc.), while the patient is regularly observed and treated by a local psychiatrist;
- the presence of organic pathology of the brain (relatively minor disturbances in the structure and functioning of some parts of the brain);
- presence of chronic infections;
- the presence of somatic diseases (cardiovascular system, liver and gallbladder, gastrointestinal tract);
- the presence of chronic diseases of an allergic nature.
These conditions appear as a result of abnormalities in the functioning of the hypothalamic-limbic structures of the brain (caused by the above diseases), and as a result, a disorder of the neurodynamics of the cerebral cortex develops.
Children's reasons
In children, a neurosis-like syndrome begins to manifest itself in the age range from 2 to 7 years.
The appearance of the syndrome in childhood can occur for various reasons. These include:
- pathologies of intrauterine development, negative influences during pregnancy (alcohol, drugs, smoking);
- diseases of the nervous system of various origins (infectious, traumatic);
- somatic disorders (chronic infectious inflammation, diseases of the gastrointestinal tract, cardiovascular system);
- hereditary pathologies of various parts of the brain.
How do neurosis-like conditions differ from neuroses?
Despite the fact that both neurosis-like conditions and neuroses are very similar to each other in manifestations and symptoms, they still differ.
And the differences lie in the reason for their appearance, since this is the whole point. Neuroses usually affect the nervous system after it has been completely exhausted by frequent blows to it, stressful situations and great physical and nervous strain. All moments and factors that exhaust a person and force him to work for wear, both physically and mentally, contribute to the manifestation of neuroses. After all, because of this, an anxious state appears, a violation of the autonomic system, and so on. Neurosis-like conditions usually do not manifest themselves due to psychological disorders. They do not have stress or problematic nervous breakdowns at their root. They usually appear due to internal organic diseases that can be established from the moment of development in the womb. It could even be a mild form of cerebral disorder, which gives rise to all the different types of syndromes during the life and functioning of the human body after birth. Sometimes neurosis-like conditions can be acquired and manifest themselves against the background of severe diseases that have an infectious nature and a chronic form.
Treatment methods
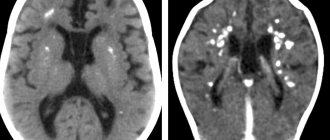
In order to effectively cure neurosis or a neurosis-like condition, you should avoid as much as possible everything that injures the nervous system and psyche. To begin with, a comprehensive diagnosis is carried out, which includes tomography, consultation with a neurologist, electroencephalogram, as well as examination by many specialists, such as a cardiologist, gastroenterologist and others. This is necessary in order to understand the true cause of the disease and find out whether it lies in diseases of other organs. Neuroses are treated with medication. They take sedatives, also those that affect blood pressure and normalize it. In addition to medications, physical procedures are necessary, without which general treatment may become ineffective. This is electrosleep, physiotherapy in the form of electrophoresis. Neurosis can be cured with the help of psychotherapy, in contrast to neurotic conditions, where treatment should all be aimed at physiology. It is definitely worth including therapeutic exercises, since without sports it is impossible to get rid of many problems even with the nervous system, not to mention diseases of the body. You shouldn’t overload yourself: you should follow the correct regime so that your rest is complete and constant. You should also eat healthy and forget about snacking. Sometimes it makes sense to go to a sanatorium for treatment, changing the environment, which will be very useful for the nervous system. It is advisable to protect yourself from stress and, if possible, quit an annoying job, change your social circle and forever forget about bad habits, which, like nothing else, negatively affect the nerves.
Treatment
Psychotherapy has become the leading method in the treatment of neuroses. Its main task is to change the patient’s attitude towards the traumatic factor he has encountered. Drug therapy plays a supporting role. Patients are prescribed antidepressants, anxiolytics and mild tranquilizers.
If there is a suspicion of neurosis, the patient should immediately consult a doctor so that therapy can be started as early as possible. Timely initiation of therapy leads to a significant improvement in the patient’s condition.
The influence of sport on the body during neurosis
There are many cases when people with neurosis are simply afraid to create sports activities for themselves, so as not to cause frightening symptoms and aggravate the course of the disease.
Usually they are frightened by physical signs, such as an accelerated pulse, rapid breathing, sweating, which in fact is a common occurrence in sports even in completely healthy people. But those who suffer from obsessions often mistake natural manifestations for signs of panic syndrome. Therefore, sport becomes a forbidden activity for neurotics. In fact, such a judgment is extremely wrong. Indeed, due to the absence of the slightest load, the body becomes weak and sluggish, the muscles lose their shape, and the nervous system becomes more vulnerable to various kinds of stress. Naturally, not every sport is beneficial for neurotics. Difficult, dangerous and overly active sports activities can damage the psyche and regularly create traumatic situations. The body will quickly wear out and be subject to stress. Therefore, it is worth engaging in such varieties that do not pose any danger, are simple and enjoyable loads. This includes cycling, skiing and skating, playing tennis, slow running, and also swimming and aerobics with a light program.
You shouldn’t immediately rush into big sports and overload yourself with exorbitant activities. This will only make the condition worse. To begin with, you can generally do ordinary exercises, but do the exercises every day so that a positive habit is developed, and the body can quickly feel the comfort of such a lifestyle.