The concept of pathological reflex
When the main neuron of the brain or neural pathways are damaged, pathological reflexes occur. They are manifested by new connections between external stimuli and the body’s response to them, which cannot be called the norm. This means that the human body reacts inadequately to physical contact, compared to a normal person without pathologies.
Such reflexes indicate any mental or neurological diseases in a person. In children, many reflexes are considered normal (extensor-plantar, grasping, sucking), while in adults the same ones are considered a pathology. At the age of two years, all reflexes are caused by an immature nervous system. Both conditioned and unconditioned reflexes can be pathological. The former manifest themselves as an inadequate response to a stimulus, fixed in memory in the past. The latter are biologically unusual for a given age or situation.
Types of reflexes studied
Today, modern medicine has proposed the following classification of pathological reflexes:
- upper limb reflexes;
- reflexes of the lower extremities;
- oral reflexes.
Neurological examination of the upper extremities
Pathological reflexes of the upper extremities include the following:
- Rossolimo (manifests itself when struck at the ends of bent 2-4 fingers).
- Zhukovsky (can be diagnosed by striking the center of the palm in response to bending the fingers).
- Bekhterev (for diagnosis it is necessary to hit the patient on the outside of the back of the hand).
- Jacobson-Lask (used at the time of studying the carporadial reflex, in which reflex flexion of all fingers of the hand occurs).
Reflexes of this etiology can appear in infancy and continue to develop until the child is 2-3 years of age. Their manifestation during this age period is not considered a deviation from the norm, and therefore is a cause for concern.
If these reflexes are present in children 4-6 years of age, then we can assume the development of pathological processes in the central nervous system.
In this case, it is mandatory to conduct an examination by a neurologist and prescribe clinical and laboratory tests to establish and confirm the alleged diagnosis.
Neurological examination of the lower extremities
Pathological reflexes of the lower extremities include the following:
- Babinsky (it is possible to identify if there is an irritant on the sole of the foot. To do this, you will need to run a hammer or toothpick from the bottom of the heel to the toes themselves).
- Oppenheim (for diagnosis you will need to run your hand along the front of the lower leg).
- Gordon (may appear when the calf muscle on the leg tightens).
- Schaeffer (diagnosed by pressing on the Achilles tendon).
- Rossolimo (to establish, you will need to hit the tips of 2-3 fingers located on the foot with a hammer).
- Zhukovsky . As in the case of pathological reflexes of the upper extremities, its diagnosis will require a light blow to the middle of the patient's foot.
- Ankylosing spondylitis No. 1 (a blow is carried out on the outer part of the foot in the area of 4-5 toes).
- Bekhterev No. 2 (to establish, you will need to make a moderate blow to the heel itself).
- Chaddock (manifests itself with a streak type of irritation of the skin of the lateral part of the foot, as well as slightly below the outer side of the ankle). The direction must be kept from the heel to the toes. Pathology will be indicated by flexion of the first big toe.
- Inferior Bekhterev-Mendel reflex . To diagnose, you will need to place the patient on his back and quickly tap with a special hammer on the back of the foot in the area of 3-4 toes. Pathological disorders will be indicated by flexion of the sole in the area of 2-5 toes.
- Binga (diagnosed when the foot is tingled with the back of a needle). A positive response will be the flexion of the first toe.
Oral reflexes
Pathological reflexes of the oral muscles usually include the following:
- Proboscis symptom (can be diagnosed by lightly tapping the lips with a hammer). To do this, the doctor asks the patient to close his eyes, after which he places his index finger on the lips and makes light blows on it. A positive reaction will be manifested in contractile movements of the orbicularis oris muscle, and the lips will also be pulled forward.
- If such a reaction appears only when a finger touches the patient’s lips, then one should assume the development of the Karchikyan .
- Sucking (for diagnosis, rough irritations are made along the edges of closed lips). The diagnosis will be confirmed by a reaction in the form of involuntary swallowing or sucking movements of the patient.
- Nasolabial (manifested by lightly tapping hammers on the back of the nose).
- Marinescu-Radovici palmar-chin symptom is caused by exposure to a rough irritant on the skin of the palm above the thumb itself. The pathological reaction will manifest itself in the form of pulling up the skin of the chin (contractile movements of the mental muscle).
- Glabellar (diagnosed by lightly tapping the central area of the eyebrows). A positive reaction will consist of percussion in the area of the glabella. With each such blow, the person will twitch and close his eyebrows. The manifestation of this reflex indicates the presence of lesions in the frontal lobe of the brain.
- Protective (manifests itself at the time of paralysis). In this case, the patient begins to experience involuntary motor acts in the paralyzed part of the limb (this will be the body’s reaction to various irritating factors from the external environment).
- An example of a protective reflex is the Bekhterev-Marie-Foy symptom (consists in bending the toes of a paralyzed limb in response to irritation). Flexion and extension of the leg in the hip and knee joints may also occur.
- Grasping reflex (manifests itself as a result of extensive damage to the frontal lobe). Metabolic and vascular pathologies can also provoke the disease.
- The chewing reflex can be diagnosed by slightly irritating the fingertips of the hand or by simply touching the palm of the back of a hammer. A positive reaction will manifest itself in a sharp grasping movement of the object that acted as a direct irritant.
Causes
Pathological reflexes can result from brain lesions and pathologies of the central nervous system, such as:
- damage to the cerebral cortex by infections, spinal cord diseases, tumors;
- hypoxia - brain functions are not performed due to lack of oxygen;
- stroke – damage to the blood vessels of the brain;
- Cerebral palsy (cerebral palsy) is a congenital pathology in which the reflexes of newborns do not fade over time, but develop;
- hypertension;
- paralysis;
- coma state;
- consequences of injuries.
Any diseases of the nervous system, damage to neural connections, or diseases of the brain can cause incorrect, unhealthy reflexes.
Possible causes of PR
The etiological factors of the occurrence of pathological reflexes are usually classified as exogenous and endogenous causes that provoke the development of a certain disease.
Exogenous causes:
- these include standard neurotropic;
- nonspecific (can affect both the central nervous system and other internal organs);
- pathogenic viruses;
- microorganisms that negatively affect the body;
- plant toxins;
- microbial toxins;
- chemicals;
- conscientious influence;
- conditioned reflexes.
Endogenous causes are divided into primary and secondary. Primary causes include ischemia, various head and back injuries, swelling of brain tissue, and genetic predisposition.
Secondary ones include those that exist in the nervous system itself under the influence of primary ones and, as a result, become the main cause of the development of pathological processes in the body:
- neuronal disorder;
- certain changes in neurotransmitters;
- change of neuron genome;
- disturbances in interneuronal transmission;
- changes in nervous trophism;
- excessive neuronal activity;
- pathological determination;
- GPUV;
- the presence of antibodies to brain tissue.
Classification of pathological reflexes
Pathological reflexes are divided into the following groups:
- Reflexes of the upper limbs. This group includes pathological carpal reflexes, an unhealthy response to external stimuli of the upper extremities. May manifest as involuntary grasping and holding of an object. They occur when the skin of the palms at the base of the fingers is irritated.
- Reflexes of the lower extremities. These include pathological foot reflexes, reactions to tapping with a hammer in the form of flexion or extension of the phalanges of the toes, and flexion of the foot.
- Reflexes of the oral muscles are pathological contractions of the facial muscles.
Pathological reflexes
Loss of reflexes (or weakening of them if the lesion is incomplete);
Common to any type of paresis or paralysis is a decrease in muscle strength.
Peripheral paralysis (flaccid, atrophic)
This type of paralysis is characterized by the following symptoms:
2. atony or hypotonia of muscles. Atonic muscles feel flabby and sluggish to the touch, passive movements are excessive, joints are “loose.” This state of the muscles gives reason to call peripheral paralysis flaccid;
3. muscle atrophy occurs as a result of disconnection from the anterior horn cell, from where neurotrophic impulses flow through the motor nerve fiber to the muscle, stimulating the normal metabolism of muscle tissue. The presence of muscle atrophy determines another definition of peripheral paralysis - as atrophic. With peripheral paralysis, fibrillar twitching can be observed in atrophic muscles - rapid contractions of individual muscle fibers or their bundles (fascicular twitching). These symptoms usually accompany those peripheral paresis that are the result of a chronic progressive process in the cells of peripheral motor neurons (in the anterior horns of the spinal cord or the motor nuclei of the cranial nerves).
Central (spastic) paralysis
Its symptoms differ sharply from those of peripheral paralysis. The main features of central paralysis are:
1. increased tendon reflexes from paralyzed limbs (hyperreflexia);
2. increased muscle tone (hypertension) or muscle spasticity, which determines another name for central paralysis - spastic. The muscles are tense, dense to the touch; during passive movements, a clear resistance is felt, which is sometimes difficult to overcome, a “jackknife” symptom.
3. the appearance of pathological reflexes are very important and permanent symptoms of central paralysis. Of particular importance are pathological reflexes on the foot, observed in cases where the lower limb is affected. The most sensitive symptoms are Babinsky, Rossolimo and Bekhterev. Other pathological reflexes are less constant. Pathological reflexes in the hands are usually weakly expressed. Pathological reflexes on the face (mainly the group of “oral automatism” reflexes) are characteristic of central paralysis or paresis of the facial muscles innervated by cranial nerves and indicate bilateral supranuclear damage to the corticonuclear pathway in the cortical, subcortical or brainstem regions.
Methods for studying movements.
Just one external examination of the patient can provide certain information and reveal one or another defect in the state of muscles and motor function. Muscle atrophy, contractures of the limbs, and a certain posture of the patient can be established. During conversation, paresis of facial muscles, speech and phonation disturbances were revealed.
Then reflexes are examined, of which a person normally has a huge number. Reflexes are divided into unconditioned, i.e. innate reactions of the body to certain irritations and conditioned ones , i.e. those reflexes that are developed in a person during his individual life experiences. Depending on the location of the reflex, all unconditioned reflexes can be divided into:
- superficial (skin reflexes and reflexes from mucous membranes),
- deep (tendinous, periostatic, articular),
- distant (light, auditory, olfactory),
- from internal organs.
Those that are distinguished by significant constancy deserve the greatest attention. Therefore, we will limit ourselves to considering those reflexes that are studied in neurological practice; these necessarily include superficial and deep unconditioned reflexes.
Superficial reflexes are caused by the application of line irritation to the skin and mucous membranes.
Reflexes from the mucous membranes: Pharyngeal and palatine (with a spatula to the back wall of the pharynx and to the velum, respectively; in response, a gag reflex with the pharyngeal and lifting of the velum with the palatine).
Skin reflexes: abdominal upper, middle and lower.
Deep reflexes: Tendon reflexes are tested by striking the muscle tendon with a neurological hammer.
On the hands - this is the carporadial reflex and reflexes from the biceps and triceps muscles;
On the legs - from the quadriceps tendon (patella) and the Achilles tendon (Achilles reflex). A necessary condition is voluntary muscle relaxation in the person being studied.
Reflexes can change as follows:
-to decrease or be lost;
-increase;
-pervert.
In addition, pathological reflexes may appear, i.e. reflexes that are not normally evoked.
A symmetrical decrease in reflexes, like an increase, is not yet a sign of a disease of the nervous system. Abdominal reflexes sometimes cannot be evoked when the abdominal wall is flabby. An extreme manifestation of increased tendon reflexes are the so-called clonus.
Clonus is a rhythmic contraction of a muscle as a result of stretching of its tendon. The most common clonus are the patella and Achilles tendon. Clonus on the hands is rare; hand clonus is more common. If a symmetrical decrease or increase in tendon reflexes is not always a sign of organic diseases of the nervous system, then uneven reflexes (anisoreflexia) indicate an organic disease.
To assess the degree of paresis, i.e. The degree of preserved muscle strength is measured using the Barre test (upper and lower) and the Buddha test.
Pathological reflexes of the oral muscles:
- naso-labial reflex or Astvatsaturov reflex - tapping with a hammer on the back of the nose, in response, contraction of the orbicularis oris muscle (pulling the lips forward);
- proboscis reflex - hitting the upper or lower lip with a hammer;
- sucking reflex - line irritation of the lips in response to sucking movements;
- distance-oral - when the hammer approaches the lips, a “proboscis” stretching of the lips occurs;
- palmar-chin reflex (Marinescu - Radovici) - line irritation of the skin of the palm in response to contraction of the muscles of the chin.
These reflexes are rarely observed in healthy adults; Normally observed in newborns and infants.
Pathological reflexes from the upper extremities:
- Rossolimo reflex - blow to the ends of bent 2-4 fingers;
- Zhukovsky reflex - a blow to the middle of the palm in response to bending the fingers;
- Bekhterev's reflex - a blow to the outer side of the back of the hand;
- Jacobson-Lask reflex - when studying the carporadial reflex - the fingers of the hand reflexively bend.
Pathological reflexes from the lower extremities:
- Babinsky reflex - caused by irritation of the sole from bottom to top towards the fingers with the handle of a hammer;
- Oppenheim reflex - runs your hand along the front surface of the lower leg;
- Gordon reflex - contraction of the calf muscle;
- Schaeffer reflex - compression of the Achilles tendon;
- Rossolimo reflex - blow to the tips of the 2-5 toes;
- Zhukovsky reflex - blow to the middle of the foot;
- Bekhterev reflex 1 - on the outside of the foot in the area of 4-5 toes;
- Bekhtereva 2 - blow to the heel.
To assess the patient's movement function, it is necessary to examine coordination. Loss of coordination or ataxia is one of the commonly observed motor disorders. Strength and tone of the muscles of the limbs can be completely preserved, but the clarity and accuracy of the movements is impaired. For coordination studies use:
- Romberg's pose - when the patient stands with his legs together, arms extended forward and eyes closed;
- complicated Romberg position - the patient is asked to stand with one leg in front of the other or stand on one leg;
- finger - nasal test;
—heel-knee test;
—gait - asking the patient to walk.
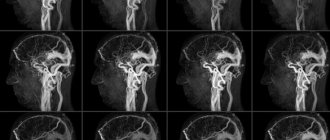
Foot reflexes
Extensor reflexes of the foot are an early manifestation of damage to the nervous system. The pathological Babinski reflex is most often tested in neurology. It is a sign of upper motor neuron syndrome. Belongs to the group of reflexes of the lower extremities. It manifests itself as follows: a stroking movement along the outer edge of the foot leads to extension of the big toe. May be accompanied by fanning out all the toes. In the absence of pathology, such irritation of the foot leads to involuntary flexion of the big toe or all the toes. Movements should be light and not cause pain. The reason for the formation of the Babinski reflex is the slow conduction of stimulation along the motor channels and impaired excitation of segments of the spinal cord. In children under one and a half years of age, the manifestation of the Babinski reflex is considered normal; then, with the formation of gait and vertical body position, it should disappear.
A similar effect can occur with other effects on receptors:
- Oppenheim reflex - extension of the finger occurs when pressing and moving from top to bottom with the thumb in the area of the tibia;
- Gordon's reflex - when the calf muscle is compressed;
- Schaeffer reflex - when the Achilles tendon is compressed.
Pathological flexion reflexes of the foot:
- Rossolimo reflex - when exposed to abrupt blows of the hammer or fingertips on the inner surface of the phalanges, rapid flexion of the II-V toes occurs;
- ankylosing spondylitis reflex - the same reaction occurs when lightly tapping the outer surface of the foot in the area of the metatarsal bones;
- Zhukovsky reflex - manifests itself when struck in the center of the foot, at the base of the toes.
Rossolimo reflex
The main foot flexion reflex is the Rossolimo reflex (deep digital reflex). It is caused by abrupt blows applied by the doctor’s fingers to the pads of the terminal phalanges of the patient’s 2-5 toes. The answer is manifested in the “nodding” of the toes - their rapid plantar flexion (Fig. 1.4.8).
In terms of diagnostic value, the Rossolimo reflex is not inferior to the Babinsky reflex. However, the Rossolimo reflex usually occurs by the end of the second week of damage to the central motor neuron, while Babinski's symptom is caused already in the first hours. There are a number of ways to induce this reflex, for example, hitting the flesh of the sole with a hammer (Zhukovsky-Kornilov reflex), tapping with a hammer on the lateral surface of the dorsum of the foot at the base of the 3-4 metatarsal bones (Bekhterev-Mendel reflex), etc.
In a similar way, a similar reflex can be studied on the hand. However, in this case, being bilateral, it can also be caused in practically healthy people. A unilateral sign should be regarded as a pyramidal symptom.
Oral automaticity reflexes
Oral automatism is the reaction of the oral muscles to a stimulus, manifested by their involuntary movement. Pathological reflexes of this kind are observed in the following manifestations:
- The nasolabial reflex, which occurs when the base of the nose is tapped with a hammer, is manifested by stretching the lips. The same effect can occur when approaching the mouth (distance-oral reflex) or when lightly hitting the lower or upper lip - oral reflex.
- Palmomental reflex, or Marinescu-Radovic reflex. The stroke movements in the area of the thumb from the side of the palm cause a reaction of the facial muscles and cause the chin to move.
Such reactions are considered normal only for infants; their presence in adults is pathological.
Oral automaticity reflexes
There are also reflexes of oral automatism - automatic involuntary movements carried out mainly by the orbicularis oris muscle and masticatory muscles in response to mechanical irritation of various parts of the face or palmar surface of the hand.
Proboscis reflex
Teymik's proboscis reflex is caused by hitting the upper lip with a hammer at the level of the gums. The answer is protrusion of the lips, sometimes combined with movement of the lower jaw.
Astvatsaturov reflex
Astvatsaturov's nasolabial reflex is caused by tapping the root of the nose with a hammer. The answer is a movement of the lips, reminiscent of a baby's sucking movement, and a blinking movement of the eyelids.
Palmomental reflex
The Marinescu-Rodovich palmomental reflex is caused by line irritation of the palmar surface of the hand, similar to how the plantar reflex is examined. The answer is bilateral contraction of the mentalis muscle. Material from the site https://wiki-med.com
These reflexes are observed in pseudobulbar syndrome, i.e., with bilateral damage to the corticonuclear pathways or projection motor cortex.
Grasp reflex
The reflex is examined while the patient's attention is diverted. When touching the palmar surface of the hand or fingers with any object, the patient involuntarily clenches his hand into a fist, grasping and holding the object tightly.
The grasping reflex usually occurs with lesions in the frontal lobe of the brain. It can be not only hetero-, but also homolateral, and sometimes even bilateral. In some cases, it takes on the character of an automatic obsessive grasping - the patient grabs an object that appears next to him, in his field of vision. A combination of the grasping reflex and the proboscis reflex is possible (Stern's symptom).
Category: Reflexes
On this page there is material on the following topics:
clinical significance of the grasp reflex
symptoms of Babinski and Rossolimo
pathological reflexes in neurology
pathological reflexes Rossolimo
Synkinesis and defensive reflexes
Synkinesis are reflexes characterized by paired movements of the limbs. Pathological reflexes of this kind include:
- global synkinesia (when the arm is bent, the leg is extended or vice versa);
- imitation: involuntary repetition of movements of an unhealthy (paralyzed) limb after the movements of a healthy one;
- coordinator: spontaneous movements of an unhealthy limb.
Synkinesis automatically occurs during active movements. For example, when moving a healthy arm or leg, a spontaneous muscle contraction occurs in a paralyzed limb, a flexion movement of the arm occurs, and an extension movement of the legs occurs.
Protective reflexes arise when a paralyzed limb is irritated and are manifested by its involuntary movement. An irritant can be, for example, a needle prick. Such reactions are also called spinal automatisms. Protective reflexes include the Marie-Foy-Bekhtereva symptom - flexion of the toes leads to involuntary flexion of the leg at the knee and hip joint.
Defensive reflexes
Protective reflexes can also be pathological - involuntary uncontrolled complex tonic movements of a paralyzed limb in response to one or another irritation of the skin of the limb or deep tissues. These reflexes are usually evoked on the legs, which has significant diagnostic value. At the same time, due to loss of sensitivity, irritation may not even be felt by the patient.
Methods of induction: irritation of the skin with a streaking movement of a needle, pricking, pinching, dorsal flexion of the foot, etc. When the limb is extended, a typical response occurs: flexion of the leg at the ankle, knee and hip joints (triple shortening). The extensor reflex is caused on a bent limb - its extension in the above joints. A step reflex is possible - bending one leg and straightening the other leg.
Protective reflexes are especially pronounced when the spinal cord is compressed, for example with extramedullary tumors. Protective reflexes can also be evoked spontaneously, under the influence of irritation from the pressure of the heel on the bed, a distended bladder, etc., and lead first to stabilization of the flexion of the legs, and then to their flexion contracture.
Tonic reflexes
Normally, tonic reflexes appear in children from birth to three months. Their continued manifestation even in the fifth month of life may indicate that the child has cerebral palsy. With cerebral palsy, congenital motor automatisms do not fade away, but continue to develop. These include pathological tonic reflexes:
- Labyrinthine tonic reflex. It is checked in two positions - on the back and on the stomach - and manifests itself depending on the location of the child’s head in space. In children with cerebral palsy, it is expressed in increased tone of the extensor muscles when lying on the back and flexor muscles when the child lies on the stomach.
- Symmetrical cervical tonic reflex. In cerebral palsy, it is manifested by the influence of head movements on the tone of the muscles of the limbs.
- Asymmetrical cervical tonic reflex. It manifests itself as increased muscle tone in the limbs when turning the head to the side. On the side where the face is turned, the extensor muscles are activated, and on the side of the back of the head, the flexor muscles.
With cerebral palsy, a combination of tonic reflexes is possible, which reflects the severity of the disease.
Tendon reflexes
Tendon reflexes are normally caused by hitting the tendon with a hammer. They are divided into several types:
- Biceps tendon reflex. In response to a hammer blow on it, the arm bends at the elbow joint.
- Triceps tendon reflex. The arm is bent at the elbow joint, and upon impact, extension occurs.
- Knee reflex. The blow falls on the quadriceps femoris muscle, under the kneecap. The result is extension of the leg at the knee joint.
Pathological tendon reflexes manifest themselves in the absence of a reaction to hammer blows. They can occur with paralysis, coma, or spinal cord injuries.
Pathological reflexes of the upper and lower extremities. Reflexes of oral automaticity.
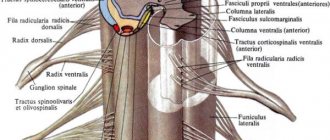
Pathological reflexes . Pathological reflexes appear when the pyramidal tract is damaged, when spinal automatisms are disrupted. Pathological reflexes, depending on the reflex response, are divided into extension and flexion.
Extensor pathological reflexes in the lower extremities
. The most important is the Babinski reflex - extension of the first toe when the skin of the outer edge of the sole is irritated by strokes; in children under 2–2.5 years old it is a physiological reflex. Oppenheim reflex - extension of the first toe in response to running the fingers along the crest of the tibia down to the ankle joint. Gordon's reflex - slow extension of the first toe and fan-shaped divergence of the other toes when the calf muscles are compressed. Schaefer reflex - extension of the first toe when the heel tendon is compressed.
Flexion pathological reflexes in the lower extremities
. The most important reflex is the Rossolimo reflex - flexion of the toes during a quick tangential blow to the pads of the toes. Ankylosing spondylitis-Mendelian reflex - flexion of the toes when hitting the dorsal surface with a hammer. The Zhukovsky reflex is the flexion of the toes when a hammer hits the plantar surface directly under the toes. Ankylosing spondylitis reflex - flexion of the toes when hitting the plantar surface of the heel with a hammer. It should be borne in mind that the Babinski reflex appears with acute damage to the pyramidal system, for example with hemiplegia in the case of cerebral stroke, and the Rossolimo reflex is a later manifestation of spastic paralysis or paresis.
Pathological flexion reflexes in the upper limbs
. The Tremner reflex is the flexion of the fingers in response to rapid tangential stimulation with the fingers examining the palmar surface of the terminal phalanges of the patient’s II-IV fingers. The Jacobson-Weasel reflex is a combined flexion of the forearm and fingers in response to a blow with a hammer on the styloid process of the radius. The Zhukovsky reflex is the flexion of the fingers of the hand when hitting the palmar surface with a hammer. Carpal-digital ankylosing spondylitis reflex - flexion of the fingers when percussing the back of the hand with a hammer.
Pathological protective, or spinal automatism, reflexes in the upper and lower extremities
– involuntary shortening or lengthening of a paralyzed limb during injection, pinching, cooling with ether or proprioceptive stimulation according to the Bekhterev-Marie-Foy method, when the examiner performs a sharp active flexion of the toes. Protective reflexes are often of a flexion nature (involuntary flexion of the leg at the ankle, knee and hip joints). The extensor protective reflex is characterized by involuntary extension of the leg at the hip and knee joints and plantar flexion of the foot. Cross protective reflexes - flexion of the irritated leg and extension of the other - are usually observed with combined damage to the pyramidal and extrapyramidal tracts, mainly at the level of the spinal cord. When describing protective reflexes, the form of the reflex response, the reflexogenic zone, is noted. area of evocation of the reflex and intensity of the stimulus.
Cervical tonic reflexes
arise in response to irritations associated with changes in the position of the head in relation to the body. Magnus-Klein reflex - when the head is turned, the extensor tone in the muscles of the arm and leg, towards which the head is turned with the chin, increases, and the flexor tone in the muscles of the opposite limbs; flexion of the head causes an increase in flexor tone, and extension of the head - extensor tone in the muscles of the limbs.
Gordon reflex
– delay of the lower leg in the extension position while inducing the knee reflex.
Foot phenomenon (Westphalian)
– “freezing” of the foot during passive dorsiflexion.
The Foix-Thevenard tibia phenomenon
is incomplete extension of the tibia at the knee joint in a patient lying on his stomach after the tibia has been held in extreme flexion for some time; manifestation of extrapyramidal rigidity.
Janiszewski's grasp reflex
on the upper limbs - involuntary grasping of objects in contact with the palm; on the lower extremities - increased flexion of the fingers and toes when moving or other irritation of the sole. The distant grasping reflex is an attempt to grasp an object shown at a distance. It is observed with damage to the frontal lobe.
An expression of a sharp increase in tendon reflexes is clonus
, manifested by a series of rapid rhythmic contractions of a muscle or group of muscles in response to their stretching. Foot clonus is caused by the patient lying on his back. The examiner bends the patient's leg at the hip and knee joints, holds it with one hand, and with the other grabs the foot and, after maximum plantar flexion, jerks the foot into dorsiflexion. In response, rhythmic clonic movements of the foot occur while the heel tendon is stretched. Clonus of the patella is caused by a patient lying on his back with straightened legs: fingers I and II grasp the apex of the patella, pull it up, then sharply shift it in the distal direction and hold it in this position; in response, there is a series of rhythmic contractions and relaxations of the quadriceps femoris muscle and twitching of the patella.
Synkinesis
- a reflex friendly movement of a limb or other part of the body, accompanying the voluntary movement of another limb (part of the body). Pathological synkinesis is divided into global, imitation and coordinator.
Global, or spastic, is called pathological synkinesis in the form of increased flexion contracture in a paralyzed arm and extension contracture in a paralyzed leg when trying to move paralyzed limbs or during active movements with healthy limbs, tension in the muscles of the trunk and neck, when coughing or sneezing. Imitative synkinesis is the involuntary repetition by paralyzed limbs of voluntary movements of healthy limbs on the other side of the body. Coordinator synkinesis manifests itself in the form of additional movements performed by paretic limbs in the process of a complex purposeful motor act.
Is treatment possible?
Pathological reflexes in neurology themselves are not treated, since this is not a separate disease, but only a symptom of some mental disorder. They indicate problems with the functioning of the brain and nervous system. Therefore, it is necessary, first of all, to look for the reason for their appearance. Only after a doctor has made a diagnosis can we talk about specific treatment, because it is necessary to treat the cause itself, and not its manifestations. Pathological reflexes can only help in determining the disease and its severity.