VD with somatoform disorders
With somatoform dysfunction, the patient sincerely considers his problem to be some kind of physical, somatic ailment. He doesn’t just think so, but actually “feels” pain, heaviness, discomfort in various parts and organs of the body. He looks for (but does not find) various serious illnesses. The patient undergoes the same examinations and tests many times. However, as a rule, there are no significant changes in them that would indicate a disruption in the functioning of the organs. Ultimately, an inattentive doctor may attribute the patient’s complaints to hypochondria.
However, a full diagnosis in this case should include a full examination of the ANS (autonomic nervous system): a thermal imager and analysis of heart rate variability. With VD, there are no disorders directly in the organs, but the functioning of the ANS, which controls blood circulation, metabolism, heat exchange, and most importantly, the activity of all internal organs, is disrupted. In this regard, a patient with VD may indeed experience such somatic symptoms.
General poor health, local discomfort in the organs, tension in one or another part of the spine during VD indicate functional stress in a specific vegetative node. A thermal imager image will show a deviation in the operation of the unit due to a failure of the temperature regime in this area. Since the ANS is responsible for heat exchange (thermoregulation), a thermal imager is one of the most effective ways to diagnose its problem areas.
Thus, when a person diagnosed with VD “hurts,” the “illness” is not imaginary. However, only a full diagnosis of the VNS will help to detect it, which should be carried out after a general examination has been carried out and a conditional diagnosis of “completely healthy” has been made. Next we will see what symptoms indicate the need to undergo such an examination.
Vegetative crisis
Autonomic crisis (panic attack) is a series of clinical manifestations characteristic of emotional disorders and disorders of the autonomic nervous system, depending on the predominance of sympathetic and/or parasympathetic innervation. The obligatory presence of anxiety, a feeling of fear (even fear for one’s life), although there is no visible threat, fear of going crazy, harming loved ones or oneself.
Vegetative crises are divided into:
- hyperventilation crisis - rapid breathing, feeling of lack of air, difficulty breathing. Fear of loss of consciousness or death. There is also tension in the muscles of the forearm and hand, legs and feet. It is important to note that the attack may end in fainting
; - vagotonic crisis - rapid heartbeat, difficulty breathing, sweating, arterial hypotension, redness of the facial skin, disruption of the gastrointestinal tract, and can also result in fainting. A crisis can be provoked by being in a stuffy room, during fasting, intense exercise, or anxiety;
- mixed crises combine the above symptoms, which can appear in turn.
It is important to carry out differential diagnosis with somatic diseases: hypo-, hyperthyroidism, diabetes mellitus, pheochromocytoma, heart rhythm and conduction disorders, gastritis, peptic ulcer, epilepsy, neuroendocrine tumors.
Autonomic dysreflexia
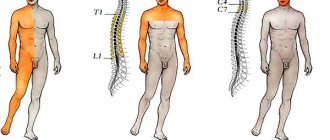
Autonomic dysreflexia is a serious complication affecting more than 50% of patients with spinal cord injury above the 6th thoracic region. In a disorder of the autonomic nervous system, irritation below the level of the spinal cord lesion is the source of severe vasoconstriction, causing paroxysmal hypertension.
Manifestations
An exacerbation of blood pressure may present with one or more of the following symptoms:
- A sudden and significant increase in systolic and diastolic blood pressure above the patient's normal level, usually associated with bradycardia.
- Throbbing headache.
- Significant sweating above the level of the lesion, especially on the face, neck and shoulders (rarely below the level of the lesion).
- Goose bumps above and below the level of the lesion.
- Blurred vision, spots in the field of vision.
- Hyperemia and swelling of the nasal mucosa, a feeling of nasal congestion.
- Bad feeling, fear, anxiety due to an impending insurmountable physical problem.
- Minimal or no symptoms of hypertension despite increased blood pressure.
- Cardiovascular signs (arrhythmias, extrasystoles).
Symptoms may be minimal or even absent despite the hypertensive state.
Causes
Autonomic dysreflexia has many potential causes. To eliminate an attack, it is necessary to conduct a diagnosis aimed at identifying a specific causative factor. The most common reasons:
- urinary tract infections;
- cystoscopy, urodynamic study, incorrect catheterization;
- inflammation of the testicles or their depression;
- expansion of the full colon during constipation;
- intestinal obstruction;
- gallstones;
- stomach ulcers or inflammation of the stomach lining;
- haemorrhoids;
- appendicitis or other abdominal pathology, trauma;
- menstruation;
- pregnancy, especially childbirth;
- vaginitis;
- sexual intercourse, orgasm;
- ejaculation;
- deep thrombosis;
- pulmonary embolism;
- frostbite;
- tight clothes, shoes;
- burns (including sunburn);
- fracture or other injury;
- surgical or diagnostic procedures;
- pain;
- osteochondrosis;
- temperature fluctuations;
- any painful or irritating sensations below the level of injury;
- drugs, large amounts of alcohol, etc.
Treatment
The procedure for treating an episode of autonomic dysreflexia begins with repositioning the patient using orthostatic blood pressure lowering. The next important condition is to relax the tight parts of clothing and remove compression products. The goal is to relieve symptoms and prevent complications associated with uncontrolled hypertension.
Pharmacological treatment:
- Nifedipine (Cordipine) is a calcium channel blocker that selectively inhibits the penetration of calcium ions through the cell membrane of the heart muscle and through the membrane of vascular smooth muscle without changing the concentration of calcium in the blood serum.
- Nitrates (nitroglycerin, isosorbide dinitrate) are drugs that relax vascular smooth muscle, with a vasodilator effect on peripheral arteries and veins.
- Terazosin is a long-acting drug that selectively blocks alpha-1 adrenergic receptors. Selective alpha-1 blockade causes relaxation of vascular smooth muscle.
- Prazosin is a selective alpha-adrenergic receptor antagonist that reduces total peripheral resistance associated with sympathetic activity.
- Captopril is a specific angiotensin-converting enzyme (ACE) inhibitor that blocks the renin-angiotensin-aldosterone system and causes a decrease in peripheral arterial resistance without changing cardiac output.
ANS disorders caused by trauma
The most serious damage in this regard is above the T6 segment. When the sympathetic is activated, for example by filling the bladder, due to vasoconstriction in the gastrointestinal tract, blood pressure increases significantly due to afferent fibers. Because the disorder blocks efferent innervation, high blood pressure persists because the vessels in the gastrointestinal tract cannot relax. In fact, this is a long-term “centralization of blood circulation”, which is also a reaction to stress.
In addition to affecting the ANS, spinal cord injury above T6 may also present with various forms of respiratory impairment. This serious disorder is a reason for young men to delay military service.
As a result of generalized vasodilation caused by a disorder of the spinal cord in the thoracic region, neurogenic shock occurs. The most commonly injured system due to impact is the sympathetic or thoracolumbar system, most commonly during injuries around T5; vascular tone is lost in the gastrointestinal tract. This reduces venous return and relatively reduces the volume of circulating blood. Tissues are hyperperfused, compensatory mechanisms are activated, but sympathetic mechanisms cannot be involved. Shock develops.
RVNS is a condition that requires a specialized treatment approach. Home treatment and traditional methods can only be used as an addition to therapy, exclusively with the permission of a doctor.
Diagnostic methods
Riddles of body temperature
Photo: taborov/Depositphotos
— How can we determine that a disease is associated specifically with a malfunction in the autonomic nervous system?
This is where thermal imaging diagnostics comes to our aid - scanning infrared radiation from the surface of the body. This diagnostic method was very popular throughout the world in the 1970s and 1980s. With its help, you can determine the temperature at any point on the surface of the body with a very high degree of accuracy (up to one hundredth of a degree).
— Doesn’t a healthy person have a universal temperature of 36.6?
No. Different parts of the body have different temperatures. For example, the temperature of the surface of the palm should normally be slightly less than the surface of the shoulder, while the temperature of the corresponding parts of the right and left halves of the body should be the same. The dysfunction of internal organs and blood vessels directly affects the body surface temperature.
By the way, if the difference between the temperature of different parts of a person’s body is more than 0.8 degrees, then this is a sign of illness.
— Why is thermal imaging diagnostics so rarely used these days?
The fact is that they tried to decipher thermal imaging images (images) from an anatomical position. For example, if the picture showed a change in temperature in the liver area, then it was believed that there were some problems there. However, it turned out that this interpretation is not very accurate, so thermal imaging diagnostics gradually lost popularity. But I was able to prove that the error was not caused by the image itself, but by the incorrect algorithm for decoding it.
— And which algorithm is correct?
I have been conducting clinical research in this area for many years and decided to figure out what exactly is causing the change in body surface temperature during illness. It is known that the general body temperature is determined by blood circulation, but the local temperature of the body surface clearly depends on the activity of local structures. Of all the structures of the metamer, only autonomic nerve cells have constant background activity and, accordingly, the temperature on a particular area of the body surface depends on the state of the autonomic nodes.
Thus, thermal imaging diagnostics makes it possible to test the state of the autonomic nervous system. My experience shows that by comparing the patient’s complaints with the results of this examination, you can get a personal portrait of the disease. The body itself gives clues to what is happening by changing the temperature in different areas of the body surface. The main thing is to interpret it correctly.
Heart study
Photo: megafilm / freepik.com
- What other methods for diagnosing vegetative dystonia do you use?
We are conducting a study on heart rate variability. To do this, a cardiac rhythmogram is recorded for 10 minutes, but it is not needed at all to analyze the condition of the heart. The main goal of the study is to evaluate how the autonomic nervous system controls it. To do this, we conduct the study when the patient is lying down, and then when he is standing. Normally, when a person gets up, his pulse should increase sharply (10-12 beats per minute more), and then after 15-30 beats return to its original value. If the changes in pulse that occur at the moment when a person gets up do not fall within the normal range, this is a sign of a disruption in the functioning of the autonomic system.