What is the sympathetic nervous system
This is part of the autonomic nervous system, which covers the upper lumbar and thoracic spinal cord, mesenteric nodes, cells of the sympathetic border trunk, and solar plexus. In fact, this section of the nervous system is responsible for the vital activity of cells and maintaining the functionality of the whole organism. In this way, a person is provided with an adequate perception of the world and the body’s reaction to the environment. The sympathetic and parasympathetic departments work together and are structural elements of the central nervous system.
What is the hypothalamus?
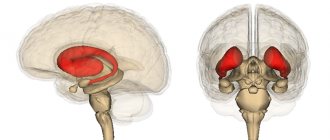
The lower part of the human brain is called the hypothalamus. The shape and structure do not have clearly defined boundaries, smoothly transitioning into the tissues of other brain regions.
Consisting of many small cell nuclear groups (to date, only thirty-two nuclear pairs have been studied), the hypothalamus generates impulses that reach other areas of the brain along special pathways. The formed nerve impulses work to control the respiratory, digestive, and circulatory systems. It is from the uninterrupted operation of the hypothalamus that the body regulates the process of maintaining water-salt balance, normalizes body temperature, and during the hot season and with increased physical activity, active sweating occurs in order to cool the skin and prevent overheating.
In addition to transmitting nerve impulses, the hypothalamus produces releasing factors - hormonal substances. Thanks to their production in the postpartum period, the woman “starts” the production of milk in the glands; childbirth, due to hormonal changes, ensures full contractile movements of the uterus to move the fetus along the birth canal, etc.
The hypothalamus performs its function only due to the close relationship of this part of the brain with the pituitary gland, which is the main organ of the endocrine system and continuously links together the work of the two systems.
The hypothalamus is divided into several zones:
Trophotropic
Located in the near zones of the hypothalamus and maintaining a constant internal environment, it normalizes the functioning of the heart and blood vessels during the rest period, and removes decay products of human activity. The main effect occurs through the parasympathetic department. When this zone is stimulated, the production of sweat and saliva increases, the heart rate slows down, blood pressure decreases, etc.
Ergotropic
Responsible for the ability of the human body, regardless of age, to adapt to changing environmental conditions, carrying out adaptation of the body and implemented through the sympathetic department.
The result of the functioning of the ergotropic system and the influence of the parasympathetic nervous system on cardiac activity: blood pressure, blood glucose levels, increased heart rate, and respiratory function increase. The ergotropic zone is located in the posterior part of the hypothalamus.
The parasympathetic division of the autonomic nervous system controls:
- lacrimation;
- pupil enlargement/decrease;
- production of saliva.
It also affects the functioning of internal organs (bronchopulmonary system, cardiac muscle, gastrointestinal tract, etc.).
Structure
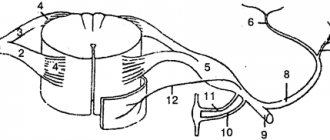
On both sides of the spine there is a sympathetic trunk, which is formed from two symmetrical rows of nerve ganglia. They are connected to each other using special bridges, forming a so-called “chain” with an unpaired coccygeal node at the end. This is an important element of the autonomic nervous system, which is characterized by autonomous operation. To ensure the required physical activity, the design distinguishes the following departments:
- cervical of 3 nodes;
- thoracic, which includes 9-12 nodes;
- area of the lumbar segment of 2-7 nodes;
- sacral, consisting of 4 nodes and one coccygeal.
From these sections, impulses move to the internal organs and support their physiological functionality. The following structural links are distinguished. In the cervical region, the nervous system controls the carotid arteries, in the thoracic region - the pulmonary and cardiac plexuses, and in the peritoneal region - the mesenteric, solar, hypogastric, and aortic plexuses. Thanks to postganglionic fibers (ganglia), there is a direct connection with the spinal nerves.
Structure of the sympathetic nerve[edit | edit code]
Efferent sympathetic neurons exit the spinal cord to the paravertebral trunk (sympathetic ganglia are located parallel to the spine). Ganglia are a collection of contacts (synapses) between neurons that exit the spinal cord (the first, or preganglionic, neuron), and nerve cells, the processes of which are sent to the periphery (the second, or postganglionic, neuron). Neurons contact organ cells at the postganglionic synapse. In addition, there are first neurons that transmit signals to other neurons in organs, as well as neurons that approach the spinal cord without switching.
Mediators of the sympathetic nervous system[edit | edit code]
The transmission of a nerve impulse at the synapse between the first and second neurons is carried out through acetylcholine (the principle of cholinergic transmission), and at the synapse of the second neuron - through norepinephrine (B). The second sympathetic neuron can have more than one contact with a cell and form more than one synapse; it branches, and each branch makes contact with several cells. In the area of these synapses, thickenings formed by contacts of nerve endings with cells are located one after another in the form of a chain. Thus, upon excitation, many cells of the organ are activated, despite the fact that the action of norepinephrine released from the second neuron is limited to the synapse. Excitation transmitted along the first neuron via acetylcholine to the adrenal glands leads to the release of adrenaline, which is distributed by the blood throughout the body (A).
Functions
The sympathetic system is an integral part of human anatomy, located closer to the spine, and is responsible for the proper functioning of internal organs. Controls the flow of blood through vessels and arteries, filling their branches with vital oxygen. Among the additional functions of this peripheral structure, doctors highlight:
- increasing the physiological abilities of muscles;
- decrease in the absorption and secretory capacity of the gastrointestinal tract;
- increased blood sugar and cholesterol;
- regulation of metabolic processes, metabolism;
- providing increased strength, frequency and rhythm of the heart;
- the flow of nerve impulses to the fibers of the spinal cord;
- dilated pupils;
- innervation of the lower extremities;
- increased blood pressure;
- release of fatty acids;
- decreased tone of smooth muscle fibers;
- adrenaline rush in the blood;
- increased sweating;
- stimulation of sensitive centers;
- dilation of the bronchi of the respiratory system;
- decreased saliva production.
Hormones and receptors
The sympathetic nervous system produces three main molecules - acetylcholine, epinephrine and norepinephrine. Acetylcholine plays a major role in the synaptic transmission of electrochemical signals from presynaptic neurons. Norepinephrine is more common as a neurotransmitter released by postsynaptic neurons and binds to specific receptors on effector cells.
Examples of effector cells include cells that line glands, cardiac or skeletal muscle cells, etc. The responses that SNS can mediate are derived from different types of receptors for these molecules in different cells. For example, when the α1 adrenergic receptor is activated, it leads to vasoconstriction. However, α2 receptors are more closely associated with the central nervous system and the regulation of hormones such as insulin and glucagon to provide fuel for muscle activity.
Another set of receptors, called β1, β2, and β3 receptors, are involved in the release of fatty acids from adipose tissue and modulation of cardiac output and heart rate. Among them, the β2 receptor has been extensively studied and has various functions, ranging from endocrine secretion to altering the metabolic state of the body and the interaction of the central nervous system with the immune system.
Sympathetic and parasympathetic nervous system
The interaction of both structures supports the vital functions of the whole organism; dysfunction of one of the departments leads to serious diseases of the respiratory, cardiovascular, and musculoskeletal systems. The effect is exerted through nerve tissues consisting of fibers that provide excitability of impulses and their redirection to internal organs. If one of the diseases predominates, the choice of high-quality medications is made by the doctor.
- System minus 60 by Ekaterina Mirimanova for weight loss
- Treatment of diabetes mellitus with folk remedies - diet. Diabetes mellitus - folk remedies for treatment
- Canadian men's haircut (PHOTO)
Any person should understand the purpose of each department, what functions it provides to maintain health. The table below describes both systems, how they can manifest themselves, and what effect they can have on the body as a whole:
| Nervous sympathetic structure | Parasympathetic nervous structure | |
| Department name | Functions for the body | Functions for the body |
| Cervical region | Dilated pupils, decreased salivation | Constriction of pupils, control of saliva secretion |
| Thoracic region | Bronchial dilatation, decreased appetite, increased heart rate | Narrowing of the bronchi, decreased heart rate, increased digestion |
| Lumbar | Inhibition of intestinal motility, production of adrenaline | Possibility of gallbladder stimulation |
| Sacral section | Bladder relaxation | Bladder contraction |
Intuition failed
Since the classic work of the British physiologist Walter Gaskell, it was believed that parasympathetic innervation is carried out by long cranial nerves (oculomotor, facial, glossopharyngeal and - main - vagus), originating in the nuclei of the midbrain and diencephalon and regulating the functioning of the eyes and nasal mucosa , glands and internal organs to the lower parts of the colon, as well as the sacral splanchnic nerves, which begin in the nuclei of the lateral horns of the sacral spinal cord and regulate the functioning of the pelvic organs.
The reason for this was some features of the sacral nerves. Anatomically, they are less branched than the sympathetic nerves of the thoracic and lumbar regions, their ganglia are located further from the spine, and they innervate internal organs that are not reached by the branches of the vagus nerve. Physiologically, the sacral nerves act on some organs in the opposite way to the thoracic and lumbar. And, finally, the organs pharmacologically innervated by them are sensitive to blockers of postganglionic acetylcholine receptors.
Classical idea of the structure of the sympathetic (red) and parasympathetic (blue) nervous systems
Anatomy of the Human Body, Henry Gray, 1918 / Wikimedia Commons
Share
The validity of classifying the sacral splanchnic nerves as a parasympathetic system has already been questioned, since the fibers of the cranial nerves extend from the central nervous system dorsally (from the back), and the sacral splanchnic nerves - ventrally (from the chest and abdomen), like sympathetic fibers. This, in turn, indicates different sources of their development in the embryonic period. However, this did not lead to the rewriting of textbooks.
Differences between the sympathetic and parasympathetic nervous systems
Sympathetic nerves and parasympathetic fibers can be located in a complex, but at the same time they provide different effects on the body. Before contacting your doctor for advice, it is recommended to find out the differences between the sympathetic and parasympathetic systems in structure, location and functionality in order to approximately understand the potential focus of pathology:
- Sympathetic nerves are located locally, while parasympathetic fibers are more discrete.
- Preganglionic sympathetic fibers are short and small, and parasympathetic fibers are often elongated.
- The nerve endings of the sympathetic are adrenergic, while the parasympathetic are cholinergic.
- The sympathetic system is characterized by white and gray connecting branches, but these are absent in the parasympathetic nervous system.
Upper cervical knot
, ganglion cervicale superius, is the largest node of the sympathetic trunk (diagram, paragraph 11).
The node has a spindle-shaped shape, its length is ≥2 cm
, and its thickness is ~0.5
cm
.
It is located in front of the transverse processes of the II-III cervical vertebrae. In front of the node are the carotid artery (indicated in red in the diagram). The vagus nerve is located lateral to the node, and the longus capitis muscle is located behind it. The following branches containing postganglionic nerve fibers arise from the superior cervical ganglion: (1) Gray communicating rami, rr. communicantes grisei, connect the upper cervical ganglion with the first three (sometimes with the fourth) cervical spinal nerves (diagram, paragraph 3). (2) Internal carotid nerve, n. caroticus internus, goes from the upper pole of the upper cervical ganglion to the artery of the same name (diagram, item 5) and along the internal carotid artery forms the internal carotid plexus, plexus caroticus internus (diagram, item 10). Together with the internal carotid artery, this plexus enters the carotid canal of the skull and then into the cranial cavity. In the carotid canal, the carotid-tympanic nerves extend from the internal carotid plexus to the mucous membrane of the middle ear. After the internal carotid artery leaves the canal, the deep petrosal nerve, n. petrosus profundus, is separated from the internal carotid plexus. It passes through the fibrocartilage of the foramen lacerum and enters the pterygoid canal of the sphenoid bone, where it joins the greater petrosal nerve to form the nerve of the pterygoid canal, n. canalis pterygoidei (diagram, item 9). This nerve, entering the pterygopalatine fossa, joins the pterygopalatine ganglion (diagram, item 8). Having passed through the pterygopalatine ganglion without synaptic switchings (in transit), sympathetic nerve fibers along the pterygopalatine nerves enter the maxillary nerve (diagram, item 7) and spread as part of its branches; carrying out sympathetic innervation of blood vessels, tissues, glands, mucous membrane of the oral cavity and nasal cavity, conjunctiva of the lower eyelid and facial skin. The part of the internal carotid plexus located in the cavernous sinus is often called the cavernous plexus, plexus cavernosus (diagram, paragraph 6). Sympathetic fibers enter the orbit in the form of the periarterial plexus of the ophthalmic artery, a branch of the internal carotid artery. The sympathetic root, radix sympathicus, branches off from the ophthalmic plexus to the ciliary ganglion. The fibers of this root pass in transit through the ciliary ganglion and, as part of the short ciliary nerves, reach the eyeball. Sympathetic fibers innervate the blood vessels of the eye and the muscle that dilates the pupil. In the cranial cavity, the internal carotid plexus continues into the perivascular plexuses of the branches of the internal carotid artery. (3) External carotid nerves, nn. carotici externi, are 2-3 stems heading to the external carotid artery. Along its course, they form the external carotid plexus, plexus caroticus externus. This plexus spreads along the branches of the artery of the same name, innervating blood vessels, glands, smooth muscle fibers, as well as tissues of the head organs. The internal and external carotid plexuses connect at the common carotid artery, where the common carotid plexus, plexus caroticus communis, is located. (4) Jugular nerve, n. jugularis, rises along the wall of the internal jugular vein to the jugular foramen, where it divides into branches going to the superior and inferior nodes of the vagus nerve, to the inferior node of the glossopharyngeal nerve and to the hypoglossal nerve. Due to this, sympathetic fibers are distributed as part of the branches of the IX, X and XII pairs of cranial nerves; laryngopharyngeal branches, rr. laryngopharyngei (laryngo-pharyngeales), participate in the formation of the laryngopharyngeal plexus, innervate (sympathetic innervation) blood vessels, the mucous membrane of the pharynx and larynx, muscles and other tissues. Thus, postganglionic nerve fibers extending from the superior cervical ganglion provide sympathetic innervation to the tissues and organs of the head and neck. (5) Superior cervical cardiac nerve, n. cardiacus cervicalis superior, descends parallel to the sympathetic trunk anterior to the prevertebral plate of the cervical fascia (diagram, item 12). The right nerve passes along the brachiocephalic trunk and enters the deep part of the cardiac plexus on the posterior surface of the aortic arch. The left superior cervical cardiac nerve is adjacent to the left common carotid artery and descends into the superficial part of the cardiac plexus, located between the aortic arch and the bifurcation of the pulmonary trunk. Middle cervical ganglion
, ganglion cervicale medium, non-permanent, located anterior to the transverse process of the VI cervical vertebra, behind the inferior thyroid artery (diagram, item 13).
The dimensions of the node do not exceed 5 mm
.
The middle cervical node is connected to the upper cervical node by one internodal branch, and to the cervicothoracic (stellate) node - by two, rarely three internodal branches. One of these branches passes in front of the subclavian artery, the other behind, forming the subclavian loop, ansa subclavia. The following branches depart from the middle cervical ganglion: (1) Gray connecting branches to the V and VI (sometimes to VII) cervical spinal nerves (see diagram, not indicated by numbers). (2) Middle cervical cardiac nerve, n. cardiacus cervicalis medius (diagram, paragraph 14). It runs parallel and lateral to the superior cervical cardiac nerve. The right middle cervical cardiac nerve is located along the brachiocephalic trunk, and the left is located along the left common carotid artery. Both nerves enter the deep part of the cardiac plexus; (3) One or two small nerves from the middle cervical ganglion participate in the formation of the common carotid plexus and the plexus of the inferior thyroid artery, innervating the thyroid and parathyroid glands. In the absence of the middle cervical ganglion, all of the named branches arise from the internodal branches at the level of the transverse process of the VI cervical vertebra, and postnodal fibers enter these branches from the cervicothoracic ganglion. Cervicothoracic (stellate) node
, ganglion cervicothoracicum, lies at the level of the neck of the first rib behind the subclavian artery, at the point where the vertebral artery departs from it (diagram, paragraph 15).
The stellate node is formed by the fusion of the lower cervical node with the first thoracic node. The cervicothoracic node is flattened in the anteroposterior direction, has an irregular (stellate) shape, its diameter on average is ~8 mm
. The following branches extend from the node: (1) Gray connecting branches, rr. communicantes grisei, which go to the VI, VII, VIII cervical spinal nerves. (2) Several branches, including from the subclavian loop, forming the subclavian plexus, plexus subclavius (subclavia), continuing to the vessels of the upper limb. Together with the branches of the subclavian artery, the sympathetic fibers of this plexus reach the thyroid gland, parathyroid glands, organs of the upper and anterior mediastinum, and also innervate the branches of the subclavian artery; (3) Several branches joining the vagus nerve and its branches, as well as the phrenic nerve; (4) Vertebral nerve, n. vertebralis, approaching the vertebral artery and participating in the formation of the sympathetic vertebral plexus, plexus vertebralis. Almost always, at the entry point of the vertebral artery into the opening of the transverse process of the VI cervical vertebra, along the course of the vertebral nerve, a small vertebral ganglion, ganglion vertebrate, is found. The vertebral plexus innervates the vessels of the brain and spinal cord and their membranes; (5) Lower cervical cardiac nerve, n. cardiacus cervicalis inferior, passing on the right behind the brachiocephalic trunk, and on the left - behind the aorta (diagram, paragraph 16). The right and left nerves enter the deep part of the cardiac plexus.
See: Neurology: Dictionary, Neurology: Internet Resources.
| LIBRARY = LIBRARY Human Physiology = Human Physiology, Human Anatomy = Human Anatomy, Human Biochemistry = Human Biochemistry, Human Psychology = Human Psychology, Medicine = Medicine, Mathematics = Mathematics, Chemistry = Chemistry, Physics = Physics, General Scientific Literature = General Science Lexis. Click here to access any source in the site's library! Click here and receive access to the any reference of the library! “I AM LEARNED. . . N E D O U C H A ?” T E S T V A S H E G O I N T E L L E C T A Premise : The effectiveness of the development of any branch of knowledge is determined by the degree of compliance with the methodology of knowledge - the knowable entity. |
Error? Click here and fix it! Search on the site E-mail of the author (author)
What diseases are associated with the sympathetic system?
With increased excitability of the sympathetic nerves, nervous conditions develop that cannot always be eliminated by self-hypnosis. Unpleasant symptoms are reminiscent of themselves already in the primary form of the pathology and require immediate medical attention. The doctor recommends to beware of the following diagnoses and to consult your doctor in time for effective treatment:
- reflex sympathetic dystrophy syndrome;
- peripheral autonomic failure;
- Raynaud's phenomenon;
- nocturnal enuresis.
Treatment
If the sympathetic nerves are excited, it is necessary to contact the attending physician and promptly begin intensive therapy that can stabilize the general condition of the clinical patient. Pathology can occur under the influence of provoking factors, which must first be identified and eliminated. In order not to bring the situation to a critical limit, and to obtain a positive treatment result, it is recommended to pay attention to the following pharmacological groups:
- benzodiazepine tranquilizers (Phenazepam, Alprazolam);
- neuroleptics (Thioridazine, Periciazine, Azaleptin);
- antidepressants (Amitriptyline, Trazodone, Escitalopram, Maprotiline, Fluvoxamine);
- anticonvulsants (Carbamazepine, Pregabalin).