Cardiometasympathetic system
The metasympathetic autonomic nervous system, as mentioned, consists of several divisions.
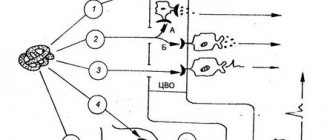
The ganglion system of the heart is already quite well studied, so we can look at how it works. Protection of the heart occurs due to reflex cycles that have a “base” in the intramural ganglia.
- MNS
- Localization of enteral NS
- Microstructure and functional organization
- Parasites, viruses and the central nervous system
- Peripheral department
- What side effect do we get?
- Autonomic ganglia
- Enterometasympathetic system
- What is a synapse?
- Intrauterine development of the central nervous system
- Functions of the metasympathetic division of the ANS
- Features of the structure of the PNS
- Law of Opposites
- Life is change
Thanks to the work of G.I. Kositsky, we know about one very interesting reflex. Stretching of the right atrium always affects the functioning of the right ventricle. He works harder. The same thing happens in the left side of the heart.
When the aorta is stretched, the contractility of both ventricles reflexively decreases. These effects occur through the metasympathetic nervous system. The Goltz reflex occurs when, when struck in the abdomen, the heart may stop contracting for a while. The reaction is associated with the activation of the abdominal nerve, with its afferent part.
The heart rate also decreases under other influences. The Aschner-Dagini reflex is the reaction of the heart when pressure is applied to the eyes. Cardiac arrest also occurs when the vagus nerve is irritated. But with subsequent irritation of the nerve, this effect goes away.
Cardiac reflexes are designed to maintain blood filling of the arteries at a single constant level. The autonomy of the nervous intracardiac system proves the ability of the heart to survive after transplantation. Although all of the cardiac major nerves have been cut, the organ continues to contract.
- Magazine archive /
- 2013 /
Metasympathetic nervous system and its role in the implementation of bladder functions
Berdichevsky B.A., Berdichevsky V.B.
Department of Faculty Surgery with a course of urology (Head – Prof. B.K. Gibert) State Educational Institution of Higher Professional Education “Tyumen State Medical Academy”, Tyumen
The full text of the article is available in the Doctor's Library
Literature
1. Lopatkin N.A., Salyukov R.V. Urological rehabilitation of patients with traumatic disease of the spinal cord. In the book: Materials of the plenum of the board of the Russian Island of Urologists. Kislovodsk; 2011: 60–67. 2. Pushkar D.Yu., Kasyan G.R., Kolontarev K.B. Unified terminology and the initial stage of examination of a neurourological patient. In the book: Materials of the plenum of the board of the Russian Island of Urologists. Kislovodsk; 2011: 15–18. 3. Alyaev Yu.G., Grigoryan V.A., Gadzhieva Z.K. Urinary disorders M.: Litterra, 2006. 160 p. 4. Laurent O.B. Etiology, pathogenesis, diagnosis of urinary incontinence. In the book: Materials of the plenum of the board of the Russian Island of Urologists. Yaroslavl; 2001: 21–41. 5. Krivoborodov G.G. Botulinum toxin type A in the treatment of urinary dysfunction in neurological patients. In the book: Materials of the plenum of the board of the Russian Island of Urologists. Kislovodsk; 2011: 11–13. 6. Borisov V.V., Akarachkova E.S. Shvarkov S.B. The significance of dysfunction of the autonomic nervous system in idiopathic overactive bladder in women. Urology 2012;1:33–37. 7. Salyukov R.V., Bushkov F.A., Penkov E.M. and others. Neurogenic dysfunction of the bladder with a high level of spinal cord injury. In the book: Materials of the plenum of the board of the Russian Island of Urologists. Kislovodsk; 2011: 157–158. 8. Nozdrachev A.D. Physiology of the nervous system. L., 1983. 9. Nozdrachev A.D., Sotnikov O.S. Metasympathetic system of the brain. In the book: Reports of the Academy of Sciences. 2006;409:707–709. 10. Tishevsky I.A. Anatomy of the central nervous system. Chelyabinsk: Publishing house of SUSU, 2000. 131 p. 11. Pokrovsky M.V., Korotko G.F. Human physiology. In 2 vols. M.: Medicine 1997. 12. Human physiology. Ed. acad. RAMS A. Agadzhanyan and prof. V. I. Tsirkina. M.: Medical book. 2003. 13. Lopatkin N.A. Guide to urology in 3 volumes. M.: Medicine, 1998. 14. Apolikhin O.I., Sivkov A.V., Romikh V.V. Urodynamic effects of high doses of M-anticholinergic in patients with detrusor overactivity due to neuropathy. In the book: Materials of the plenum of the board of the Russian Island of Urologists. Kislovodsk; 2011: 73–74. 15. Vishnevsky A.A., Livshits A.V. Electrical stimulation of the bladder. M.: Medicine 1973. 160 p. 16. Innervation of the bladder and its disorders (according to Muller) https://myneur.ru /13/13 3/13 3 /20. 17. Stohrer M., Blok B., Castro-Diaz D. et al. Guidelines on Neurogenic Lower Urinary Tract Dysfunction. European Association of Urology 2010. 18. Abrams P, Cardozo L, Fall M et al. The standardization of terminology of lower urinary tract function: Report from the Standardization Sub-committee of the International Continence Society. Neurourol Urodyn. 2002; 21(2): 167–178. 19. Mazo E.B., Krivoborodov G.G. Overactive bladder M.: Veche, 2003;75. 20. Al-Shukri S.H., Kuzmin I.V. Detrusor overactivity and urge urinary incontinence: a manual for doctors. St. Petersburg, 2001: 40 p. Medicine 1973;160 p. 21. Gadzhieva Z.K. Urinary disorders: a guide / Ed. SOUTH. Alyaeva. M.: Geotar-Media, 2010:176. 22. Appell RA Overactive bladder in special patient populations. Rev Urol. 2003; 5(Suppl. 8):S.37–41. 23. Wyndaele JJ, Castro D, Madersbacher H et al. Neurologic urinary and faecal incontinence. In: Abrams P, Cardozo L, Khoury S, Wein A, eds. Incontinence. Plymouth: Health Publications. 2005: 1061–1062. 24. Bradley WE, Timm GW, Scott FB Innervation of the detrusor muscle and urethra. Urol Clin North Am. 1974; 1 (1): 3–27. 25. Burns AS, Rivas DA, Ditunno JF The management of neurogenic bladder and sexual dysfunction after spinal cord injury. Spine (Phila Pa 1976). 2001; 26 (24 Suppl): S. 129–136. 26. Davidov M.I. Neurogenic acute urinary retention. In the book: Materials of the plenum of the board of the Russian Island of Urologists. Kislovodsk; 2011: 57–60. 27. Kuprin V.N., Belova A.N. Neurourology. Guide for doctors. M.: Antidor, 2005:464 p. 28. Madersbacher H., Wyndaele J. J., Igawa Y. et al. Conservative management in neuropathic urinary incontinence. In: Incontinence, 2nd edn. Abrams P., Khoury S., Wein A., eds. Plymouth: Health Publication. 2002;697–754. 29. Morozov V.I., Akhunzyanov A.A., Bilyalov M.G. and others. Neurological aspects of neurogenic bladder dysfunction. Kazan, 1999. pp. 28–33. 30. Wyndaele JJ, Castro D, Madersbacher H et al. Neurologic urinary and faecal incontinence. In: Abrams P, Cardozo L, Khoury S, Wein A, eds. Incontinence. Plymouth: Health Publications. 2005: 1061–1062. 31. Del Popolo G., Filocamo MT, Li Marzi V. et al. Neurogenic detrusor overactivity treated with English Botulinum Toxin A: 8-year experience of one single center. Eur Urol. 2008;53(5):1013–1019. 32. Franco I., Horowitz M., Grady R. et al. Efficacy and safety of oxybutynin in children with detrusor hyperreflexia secondary to neurogenic bladder dysfunction. J Urol. 2005;173(1): 221–225. 33. Borisov V.V., Akarachkova E.S. Shvarkov S.B. The significance of dysfunction of the autonomic nervous system in idiopathic hyperactive bladder in women. Urology. 2012; 1:33–37. 34. Al-Ali M., Salman G., Rasheed A. et al Phenoxybenzamine in the management of neuropathic bladder following spinal cord injury. Aust NZJ Surg. 1999; 69 (9): 660–63. UPDATE MARCH 2008 35. 35. Homma Y., Ando T., Yoshida M., Kageyama S. et al. Voiding and incontinence frequencies: variability of diary data and required diary length. Neurourol Urodyn. 2002;21(3):204–209. 36. https://www.uroweb.ru 37. Cain MP, Wu SD, Austin PF et al. Alpha blocker therapy for children with dysfunctional voiding and urinary retention. J Urol. 2003;170(4 Pt 2):1514–15 discussion 1516–1517. 38. Wyndaele JJ, Castro D, Madersbacher H et al. Neurologic urinary and faecal incontinence. In: Abrams P, Cardozo L, Khoury S, Wein A, eds. Incontinence. Plymouth: Health Publications. 2005: 1061–1062. 39. Pushkar D.Yu. Overactive bladder in women. M.:MED press-inform; 2003. 160 p.
About the authors / For correspondence
B. A. Berdichevsky – professor of the department, e-mail [email protected] ru
Localization of enteral NS
The metasympathetic nervous system, intramural nerve plexuses are found in the heart and all hollow organs, but are more deeply studied using the example of the innervation of the stomach and intestines. In these parts of the gastrointestinal tract, the intragastric and enteric nervous system is represented so abundantly that the number of neurons (108 units) is comparable to the spinal cord. This gives rise to the figurative name of its “abdominal brain.”
acetylcholine, norepinephrine, serotonin, dopamine, nucleotides such as adenosine triphosphate and many neuropeptides: vasoactive intestinal peptide, substance P, somatostatin, enkephalin, gastrin-cholecystokinin-like substance, bombesin, neurotensin and others.
The intramural nervous regulation of intestinal motility is based on the peristaltic reflex. Physiology of the autonomic nervous system It ensures the movement of chyme in the aboral direction and represents a coordinated contraction of the circular muscles at the site of action of a mechanical stimulus (stretching a loop of intestine with chyme or, in experimental conditions, a balloon), and relaxation of the muscle layers caudal to the site of the stimulus on the mucosa. Similar effects are achieved when using chemical irritants.
Based on their responses to a long-term impulse of depolarizing current, all enteric neurons of the intermuscular plexus can be divided into two types: the first is type S and the second is type AN. Neurons of type S respond to this stimulation with a long series of spikes, and neurons of type AN - with only one or two spikes, which are accompanied by a strong and long-lasting (4-20 s) trace hyperpolarization, which is absent in type S. The spike in type S neurons is caused by sodium, and in neurons of the AN type - sodium and calcium conductivity of the membrane.
Question 1 Physiological features of the metasympathetic division of the ANS. Metasymptotic modules.
The metasympathetic section of the ANS is a complex of intramural microganglionic formations located in the walls of hollow visceral organs that have motor activity (heart, bronchi, stomach, intestines, ureter, bladder, urethra, or urethra, uterus, vas deferens). An example of a metasympathetic system is the nerve plexuses in the gastrointestinal tract, including the subserosal, intermuscular (Auerbach) and submucosal (Meissner). Each of these plexuses contains many microganglia, in which three types of neurons are distinguished (according to Dogel): type I neurons - efferent (their axon is in contact with the muscle cell); type III neurons - associative neurons; with their participation, local reflex arcs are formed; type II neurons - afferent neurons
In this case: part of the axons of afferent neurons switches to type I neurons (closure of the reflex arc at the microganglion level); some of the axons of afferent neurons go to the paravertebral or prevertebral ganglia, switching here to other neurons; some of the axons of afferent neurons reach the neurons of the spinal cord, switching here to other neurons.
The metasympathetic system plays the role of an independent integrating formation, since its neurons (afferent, efferent and intercalary) form local reflex arcs. Due to these arcs, processes of local regulation of the activity of the heart, digestive tract and other organs that have a smooth muscle basis are carried out.
The basis of the activity of the metasympathetic system is the functional module, i.e. a cluster of type I, II and III neurons connected in a certain way (according to Dogel), among which the leading ones are oscillator cells (pacemakers).
Cells are pacemakers, i.e. Pacemakers are spontaneously excited at a specific rhythm, and their action potentials are transmitted through a system of interneurons to a motor neuron, the axon of which is in contact with the muscle cell. This regulates the motility of the digestive tract or other structures.
Question 2 Detoxification and other non-digestive functions of the liver.
liver functions
Bile formation and excretory, Barrier and protective, Neutralizing and biotransformation, Metabolic, Homeostatic, Depositing, Regulatory
Non-digestive functions of the liver: The liver produces many proteins 100% fibrinogen, 96% albumin, 85% globulins, coagulation and anticoagulation factors. The liver synthesizes glucose, glycogen, fats, and ketone bodies. in the liver, ammonia, a toxic product, is bound due to the formation of urea and creatinine. Many hormones are inactivated in the liver: steroids, insulin, glucagon, biogenic amines - catecholamines, serotonin, histamine. In the liver, toxic and medicinal substances are neutralized due to their oxidation, reduction, and hydrolysis of conjugation with glucuronic and other acids. Thanks to this, the liver performs the most important function - a barrier. The liver acts as a depot of blood, carbohydrates, proteins, fats, vitamins (type A, D2, D3, K, C, PP), microelements. The liver takes an active part in erythrokinetics in the destruction of red blood cells and heme degradation. The liver is involved in immunopoiesis and immunological reactions.
Let us dwell in more detail on the processes of neutralization of metabolites and foreign compounds.
Up to 80% of liver cells are hepatocytes. They are organized in the form of plates (two layers of hepatocytes). The inner surfaces of each layer form a bile capillary, and their outer surfaces face the sinusoids. Liver sinusoids are modified capillaries. Mixed blood circulates through them - arterial-venous. Venous blood enters the liver from the portal vein, arterial blood from the hepatic artery. From the sinusoids, blood collects in the branches of the hepatic vein, which flows into the inferior vena cava.
1.2 liters of blood flows through the liver per minute, while 70% of it (820 ml) enters through the portal vein, which collects blood from the digestive tract.
It is in hepatocytes that the neutralization of both its own metabolites and foreign substances that do not contribute to the plastic or energy processes of the body (xenobiotics) occurs.
Neutralization of substances usually occurs in two phases. In the first phase, the substance undergoes oxidation, reduction or hydrolysis, resulting in the formation of groups -OH, -COOH, -SH, -NH2 and others. In the second phase, any substance is added to these groups - glucuronic acid, sulfuric acid, glycine, glutamine, acetyl residue. These reactions are called “conjugation reactions.”
Question 3 Types of higher nervous activity. Theory I.P. Pavlova about the types of GNI. Strength, mobility and balance of the processes of excitation and inhibition as the basis for the division into types of GNI. General characteristics of the main types of internal income. Modern ideas about individual psychological differences in humans.
Teaching of I.P. Pavlova on the types of higher nervous activity.
I.P. Pavlov believed that both an animal and a specific person have their own, individual way of responding to stimuli. This individuality is determined by the properties of the nervous system. Among such properties, I.P. Pavlov considered three parameters - the strength of nervous processes, the balance of nervous processes and the mobility of nervous processes (excitation and inhibition). Under the strength of nervous processes of excitation and inhibition, I.P. Pavlov understood the degree of their expression and the ability to repeatedly reproduce conditioned reflexes. Nervous processes can be strong or weak.
Strong nerve cells, according to the ideas of I.P. Pavlova, have a significant supply of functional substances and they are able to work long and hard at a high level. Weak nerve cells are characterized by low efficiency, and the consumption of substances in these cells occurs even with a slight voltage of nervous processes.
I.P. Pavlov believed that, according to the relationship between themselves, nervous processes can be balanced or unbalanced. Under the mobility of nervous processes I.P. Pavlov understood speed (speed) and the possibility of transition from one process to another, i.e. from excitation to inhibition or from inhibition to excitation, the rate of change in a behavioral response when the external environment changes. Depending on this, nervous processes can be mobile (labile) or inert. Moreover, each individual is characterized by its own combination of the basic properties of cortical activity, which determines the peculiarity of the GNI. I.P. Pavlov showed that among people the same four types can also be distinguished, each of which corresponds to one of four types: 1) strong, normally excitable, balanced, fast (sanguine) type); 2) strong, hyperexcitable, unrestrained (choleric) type; 3) strong, normally excitable, balanced, slow (phlegmatic) type; 4) hyperexcitable, weak (melancholic) type.
In addition, I.P. Pavlov believed that people differ from each other in one more important parameter - in the relationship between the first and second signaling systems. Therefore, he introduced the concept of specific human types of GNI, identifying three main ones - artistic, mental and average. Thus, starting from the 20s in domestic and foreign literature, thanks to the works of I.P. Pavlov established the idea that the type of higher nervous activity is a set of innate (genotype) and acquired properties of the nervous system that determine the nature of the interaction of the organism with the environment and are reflected in all functions of the organism. The specific importance of congenital and acquired in the phenotype may vary depending on conditions.
Strong, balanced, mobile (labile) type, or sanguine type of temperament. It is characterized by strong nervous processes and their great mobility, great ease of transition from one process to another, ease of development of conditioned reflexes and ease of their inhibition, pronounced negative and positive induction, which limits the irradiation of excitation and inhibition processes in the cerebral cortex
Strong, unbalanced, active type (“unrestrained”), or choleric type of temperament. It is characterized by a pronounced predominance of the excitation process over inhibition (the presence of a strong excitatory process with a relative weakness of the inhibitory process). Strong, balanced, inert type, or phlegmatic type of temperament. This type is characterized by the ability to develop very persistent conditioned reflexes. Weak type, or melancholic temperament. This type of VND is characterized by high sensitivity but low performance.
Ticket 44
Microstructure and functional organization
The activity of the MNS is based on a functional module: a cluster of neurons connected in a special way, where oscillatory cells are distinguished, such as sensory neurons, tonic neurons, motor neurons, interneurons. The oscillator cell is the key cell of the module. It is excited spontaneously in a certain rhythm, transmitting action potentials through interneurons to the motor neuron, the axon of which is in contact with the muscle cell. The more active the oscillator cell, the more pronounced the inhibition of the motor neuron becomes. The oscillator-motoneuron system is modulated by:
- afferent neurons acting on the motor neuron through activation through the cholinergic synapse or at its termination (axo-axonal inhibition), removing the inhibitory effect on the muscle cell;
- parasympathetic and sympathetic postganglionic fibers, by influencing interneurons.
Oscillatory cells are extremely stable, and their function does not change under the action of neurotransmitters or ganglion blockers. Through an interneuron, an impulse from an oscillator cell triggers slave cells, which, according to the structure of their connections, represent sequentially organized chains. The sensory elements included in the neural ensemble activate special tonic neurons, causing the appearance of a prolonged discharge in them. In turn, tonic neurons form excitatory or inhibitory synaptic input to slave cells. Activation of a tonic neuron depends on the nature of the connection and can create either supportive excitation or, conversely, inhibition, which determines the direction of the responses of smooth muscles, epithelial cells, endocrine and other elements.
Metasympathetic nervous system. Physiology
What neurons does this nervous system consist of? What is the structure of the metasympathetic nervous system? Let's take a closer look at the neuron system. In the structure of the nerve fibers of each hollow organ there is a rhythm director who controls motor activity (vibration), there are intercalary, tonic and effector neurons. And of course, they have their own sensory cells.
The key unit of the entire module is the oscillator cell, or pacemaker. This cell transmits its signals (action potentials) to the motor neuron. The axon of each motor neuron makes contact with muscle cells.
The function of the oscillator cell is very significant. Cells are protected from external influences, for example from the influence of ganglion blockers or neurotransmitters.
Thanks to the work of the network of neurons, the work of the muscles, the apparatus that absorbs nutrients, and the mechanism of blood supply to the organ are controlled.
Parasites, viruses and the central nervous system
A large number of “interventionists” live in the brain. Various viruses: cytomegalovirus, herpes virus, papillomavirus. Toxoplasma enters the human body, for example, through cat scratches, resulting in the formation of toxoplasmosis gumma. If someone is diagnosed with epilepsy, can you somehow relate this to the fact that they have worms? Hardly. If a child has epilepsy, will you go to a helminthologist? You 100% won't go. And in vain
It is very important to establish the direction in which to go. It is necessary to carry out certain actions: antiparasitic programs, or at least be examined for the presence of toxoplasma, cytomegalovirus
Important Drugs for the treatment of Parkinson's disease
Peripheral department
This section is represented by nerve cells and fibers located outside the spinal cord and brain. This part of the visceral nervous system accompanies the vessels, weaving around their wall, and is part of the peripheral nerves and plexuses (related to the normal nervous system). The peripheral department also has a clear division into the sympathetic and parasympathetic parts. The peripheral department ensures the transfer of information from the central structures of the visceral nervous system to the innervated organs, that is, it carries out the implementation of what is “planned” in the central autonomic nervous system.
Sympathetic department
Represented by the sympathetic trunk, located on both sides of the spine. The sympathetic trunk is two rows (right and left) of nerve ganglia. The nodes are connected to each other in the form of bridges, moving between parts of one side and the other. That is, the trunk looks like a chain of nerve lumps. At the end of the spine, two sympathetic trunks unite into one unpaired coccygeal ganglion. In total, there are 4 sections of the sympathetic trunk: cervical (3 nodes), thoracic (9-12 nodes), lumbar (2-7 nodes), sacral (4 nodes and plus one coccygeal).
The cell bodies of neurons are located in the area of the sympathetic trunk. Fibers from the nerve cells of the lateral horns of the sympathetic part of the central part of the autonomic nervous system approach these neurons. The impulse can switch on the neurons of the sympathetic trunk, or it can transit and switch on intermediate nodes of nerve cells located either along the spine or along the aorta. Subsequently, the fibers of the nerve cells, after switching, form weaves in the nodes. In the neck area it is the plexus around the carotid arteries, in the chest cavity it is the cardiac and pulmonary plexuses, in the abdominal cavity it is the solar (celiac), superior mesenteric, inferior mesenteric, abdominal aortic, superior and inferior hypogastric. These large plexuses are divided into smaller ones, from which autonomic fibers move to the innervated organs.
Parasympathetic Division
Represented by nerve ganglia and fibers. The peculiarity of the structure of this department is that the nerve nodes in which the impulse switches occur are located directly next to the organ or even in its structures. That is, the fibers coming from the “last” neurons of the parasympathetic department to the innervated structures are very short.
From the central parasympathetic centers located in the brain, impulses go as part of the cranial nerves (oculomotor, facial and trigeminal, glossopharyngeal and vagus, respectively). Since the vagus nerve is involved in the innervation of internal organs, its fibers reach the pharynx, larynx, esophagus, stomach, trachea, bronchi, heart, liver, pancreas, and intestines. It turns out that most internal organs receive parasympathetic impulses from the branching system of just one nerve: the vagus.
From the sacral sections of the parasympathetic part of the central visceral nervous system, nerve fibers go as part of the pelvic splanchnic nerves and reach the pelvic organs (bladder, urethra, rectum, seminal vesicles, prostate gland, uterus, vagina, part of the intestine). In the walls of organs, the impulse is switched in the nerve ganglia, and short nerve branches are in direct contact with the innervated area.
Metasympathetic division
It stands out as a separate separately existing department of the autonomic nervous system. It is detected mainly in the walls of internal organs that have the ability to contract (heart, intestines, ureter and others). It consists of micronodes and fibers that form a nerve plexus in the thickness of the organ. The structures of the metasympathetic autonomic nervous system can respond to both sympathetic and parasympathetic influences. But, in addition, their ability to work autonomously has been proven. It is believed that the peristaltic wave in the intestine is the result of the functioning of the metasympathetic autonomic nervous system, and the sympathetic and parasympathetic divisions only regulate the force of peristalsis.
Metasympathetic part of the nervous system
Most internal organs, in addition to sympathetic and parasympathetic innervation, have their own autonomous mechanism, thanks to which the organs are able to contract rhythmically at a certain frequency without external influence. This autonomous mechanism, which causes rhythmic contractions of the heart, digestive tract, uterus... is carried out by the metasympathetic n/s.
) are located in the walls of internal organs. Preganglionic fibers depart from them, which go to microganglia, which also lie inside the wall of the organs. Postganglionic fibers emerge from these microganglia, carrying out rhythmic contractions of the innervated organs.
This relative functional autonomy of the metasympathetic system is explained by its own neurogenic rhythm and an independent reflex arc, consisting of the following links: sensory (sensitive), associative (intercalary), efferent (motor) and mediator. Most hollow organs, along with the existence of extraorgan sympathetic and parasympathetic n/s, have their own basic mechanism. Control of the work in this case is provided by reflex arcs that close within the walls of the organs themselves. Previously, only the reflex arcs that closed in the submucosal and intermuscular plexuses of the intestine were classified as the third section of the autonomous n/s, called the enteral. Now the concept of metasympathetic n/s is much broader; it covers the entire complex of hollow visceral organs (heart, intestines, gall bladder, bronchi, uterus, ureter, bladder).
(Existing evidence suggests that the fundamental model of the metasympathetic nervous system is completely consistent with a similar model of the central nervous system. Most of the real and putative mediators of metasympathetic n/s are also neurotransmitters in the central nervous system. It is now firmly established that, for example, in the enteric part of the metasympathetic system, the mediator function is performed by at least 20 mediators of cholinergic, adrenergic, serotonergic and other nature. All of them are found in the central nervous system. The metasympathetic nerve also contains blood-ganglionic barrier structures that resemble the blood-brain barrier in nature. They protect metasympathetic neurons from direct effects of substances circulating in the blood
.)
Indeed, the metasympathetic n/s has its own sensory elements, which can be mechano-, chemo-, thermo- and osmoreceptors. They constantly send information about the state of the wall of the internal organ to their internal networks. Along with this, sensory elements are capable of transmitting signals to the central structures of the nervous system.
Metasympathetic neurons synapse into networks that process incoming sensory information and simultaneously control the activity of effector neurons. The latter, in turn, are common final pathways to effectors and can initiate, support, and finally inhibit their behavior.
In vertebrates, the nuclear formations of the sympathetic and parasympathetic systems are located in the central nervous system. Metasympathetic n/s does not have such representations and is to a much greater extent independent. The sympathetic nervous system innervates all vessels, and through them the skeletal muscles, all internal organs, part of the smooth muscles of the eyeball, hair muscles, etc. The area of innervation of the parasympathetic nervous system is narrower: exocrine glands, part of the smooth muscle of the eyeball, internal organs. The scope of innervation of the metasympathetic n/s is even more limited and covers purely internal organs, and not all of them, but only those with their own motor rhythm. Thus, the metasympathetic part of the n/s has many features that distinguish it from other parts of the autonomous n/s.
Features of the metasympathetic nervous system:
1. It innervates only internal organs endowed with their own motor activity; in the sphere of its innervation there are smooth muscle, absorptive and secreting epithelium, local blood flow, and local endocrine elements.
2. It receives synaptic inputs from the sympathetic and parasympathetic systems and does not have direct synaptic contacts with the efferent part of the somatic reflex arc.
3. Along with the general visceral efferent pathway, it has its own sensory link
4. Representing truly basic innervation, it has much greater independence from the central nervous system than the sympathetic and parasympathetic n/s
5. Organs with metasympathetic pathways destroyed or switched off with the help of ganglion blockers lose their inherent rhythmic motor function.
6. Metasympathetic n/s has its own mediator link.
In conclusion, I would like to note, according to modern concepts, the main role of the parasympathetic and metasympathetic systems is to implement the mechanisms of various functions that ensure homeostasis - the relative dynamic constancy of the internal environment and the stability of basic physiological functions.
In contrast, sympathetic n/s is considered as a system of anxiety, mobilization of protective forces and resources, for active interaction with environmental factors. It follows from this that, by ensuring maximum tension in the functions of organs and systems to protect the body, sympathetic nervous system destabilizes the constancy of the internal environment. The task of restoring and maintaining this constancy, disturbed as a result of excitation of the sympathetic nervous system, is taken on by the parasympathetic and metasympathetic systems.
Lecture 10. ANALYZERS
The concept of analyzers. Olfactory, visual,
Equilibrium auditory, gustatory, tactile and
Visceral analyzers
The cerebral cortex constantly receives and analyzes various information coming from internal organs and from the external environment. The perception and analysis of this information is provided by analyzers - derivatives of the nervous system.
The analyzer is a single functional system of neurons that perceive irritation, transmit excitation and analyze it in the cerebral cortex. In each analyzer, according to I.P. Pavlova distinguishes three sections: perceptive, conducting and central.
1) The perceptive department is receptors that transform the energy of external or internal stimulation into a nervous process. They are divided into two groups: exteroceptors
, which perceive irritations from the external environment and, together with auxiliary structures, form sensory organs, and
interoreceptors
, which perceive irritations from the internal environment of the body.
These include visceroreceptors (
located in the internal organs and perceive various sensations, for example, the fullness of the stomach, intestines, bladder, pain); proprioceptors (located in the musculoskeletal system and determine muscle-joint sensation); vestibuloreceptors (located in the locomotor apparatus and the organ of balance - they signal changes in the position of the body and its individual parts in space.
2) The conducting section serves to conduct nerve stimulation. It includes nerves (spinal and cranial) and exteroceptive pathways of the spinal cord and brain.
3) The central section is the neurons of the projection zones of the cerebral cortex (visual, auditory, etc.), where the analysis and synthesis of the received sensations occurs. Based on incoming information, an attitude towards the surrounding world and the body’s response to irritations in various situations are formed.
Classification of analyzers.
Depending on what stimulus the receptors perceive, the following analyzers are distinguished:
1) Visceral analyzers perceive irritations arising in organs and tissues and signal to the central nervous system about the state of the internal environment of the body. Perceiving department - interoreceptors, conducting - spinal and cranial nerves, central - brain and spinal cord.
2) The tactile analyzer perceives various irritations from the external environment (cold, heat, touch, pressure, pain...). The perceptive department consists of exteroceptors of the skin and mucous membranes of a number of organs in contact with the external environment, namely the mucous membrane of the eyes, lips, mouth, tongue, nasal cavity, rectum and external genitalia. The perceptive department is sometimes also called the organ of touch (organon tactus). Skin sensitivity is caused by nerve endings that have different shapes and structures. Various sensitive points and areas of the skin can be considered as projections of corresponding points in the brain. The following areas of the skin are especially rich in sensitive nerve endings: lips, tip of the nose, trunk or proboscis (pig, mole), fingertips (primates). In addition to the skin itself, hair, which is connected to nerve endings, also has a sense of touch. In a number of places, special tactile hairs (vibrissae) develop. They are especially common on the lips and cheeks and in the form of separate tufts above the eyes and on the chin, forming a sensitive area on the muzzle. The conducting section of the tactile analyzer is the s/m and cranial nerves, the central section is the spinal cord and brain.
3) The taste analyzer provides analysis of the ingested feed and water. It has not yet been studied enough in animals, but there is evidence that they can distinguish all four basic tastes (sweet, bitter, sour and salty), but prefer certain taste sensations. Thus, pigs and dogs prefer sweet foods, cattle and horses prefer salty foods. As for birds, their sense of taste is poorly developed and is largely replaced by the sense of touch. The receptive section of the taste analyzer, or taste organ (organon gustus), is represented by numerous taste buds, which are located in the epithelial layer of the oral mucosa. In domestic animals, taste buds are located mainly on the taste buds. In addition to them, they are also found in the pharynx, hard and soft palate, pharynx, and larynx. In young animals they are more common and can be found in other places of the oropharynx, and in adults - on the tip, edges and back of the tongue. Animals with well-developed chewing surfaces of molars (horse, cow, sheep, goat) have the largest number of taste buds - several tens of thousands. In humans, the total number of taste buds reaches two thousand. Taste buds, located in the thickness of the mucous membrane, form its numerous outgrowths - papillae. The papillae of the tongue are heterogeneous in their function and are divided into mechanical and gustatory. The taste buds include: mushroom-shaped, leaf-shaped, ridge-shaped. In fungiform papillae
taste buds are usually concentrated in its expanded tip (cap) - they perceive sour and salty tastes.
Leaf-shaped papillae
are vertically oriented folds.
The taste buds lie on the opposite sides of these folds. They perceive sweet taste. Roller-shaped (vallate) papillae
look like a cylinder surrounded by a ridge. Taste buds are located both on the side surfaces of the cylinder and on the inside. They perceive bitter taste. In a hungry animal or person, the taste buds are in a state of high activity. During meals, their activity noticeably decreases and begins to gradually recover only after one and a half to two hours. And only four to five hours after eating, the ability to acutely perceive taste stimuli becomes high again. If you eat the same food day after day, it begins to seem tasteless. This is explained by the taste buds becoming accustomed to monotonous stimuli. Various spices and seasonings for dishes increase their sensitivity. To a certain extent, foods that contrast in taste, for example, sweet tea and a sandwich with salted fish, stimulate and restore the activity of taste receptor cells. With various diseases of the gastrointestinal tract, taste sensitivity is distorted, even the appearance of the tongue changes. Thus, according to the observations of clinicians, with chronic gastritis with high acidity, chronic enteritis, colitis, the tongue somewhat increases in volume and is almost completely covered with a whitish coating. A dry, coated and slightly reduced tongue is characteristic of gastritis with low and zero acidity. With an exacerbation of peptic ulcer disease, the plaque is often gray or yellowish-gray. With the help of this plaque, the body, as it were, seeks to block the taste apparatus of the tongue, thereby suppressing appetite and creating a gentle regime for the diseased organ. Particular attention is paid to plaque on the tongue. Thus, a thin coating indicates an incipient disease or superficial localization of the pathological process; significantly more pronounced plaque is a sign of a chronic disease. If the white coating on the tongue, gradually thickening, becomes yellow and then gray, dark in color, this means the progression of the disease. Lightening and thinning of plaque indicates an improvement in the condition.
So, the receptive section of the taste analyzer is represented by taste buds. Each taste bud is formed by taste receptor and supporting cells. The shape of the bud resembles an onion, the top of which faces the surface of the tongue and opens on it with a tiny hole - the taste pore. Microvilli of receptor cells face the lumen of the taste pore; They, in fact, come into direct contact with various nutrients. As soon as this happens, reactions begin in the receptor cell, as a result of which the chemical irritation is transformed into a nerve impulse. Information about the food substance travels along nerve fibers (several of them approach each taste bud), which unite into nerves. The conducting section is represented by cranial nerves: the chorda tympani (7th facial nerve) - from the anterior 2/3 of the tongue; glossopharyngeal nerve (9th) - from the posterior 1/3 of the tongue and from the splenoid papillae; vagus nerve (10th) - from the pharynx. The central processes of the neurons that carry out taste innervation in the oral cavity are sent to the above-mentioned nerves to their common sensitive nucleus, which lies in the medulla oblongata. The axons of the cells of this nucleus are sent to the thalamus (diencephalon), where the impulse is transmitted to the following neurons, the central processes of which end in the cerebral cortex.. So, the taste center of the brain is located in the temporal lobe. This is where the highest analysis of taste sensations takes place.
4) The olfactory analyzer provides the ability to distinguish odors. In the life of terrestrial animals, the sense of smell plays an important role in communicating with the external environment. It is used to recognize odors and to determine gaseous substances contained in the air. In the process of evolution, the olfactory organ, which is of ectodermal origin, first formed near the oral opening, and then combined with the initial part of the upper respiratory tract, which separated from the oral cavity. Some mammals have a very well developed sense of smell (macromatics). This group includes insectivores, ruminants, ungulates, and carnivores. Other animals have no sense of smell at all (anosmatics). These include dolphins. The third group of animals has a sense of smell, but it is poorly developed (microsmatics). These include pinnipeds and primates. The olfactory analyzer is a distant-action device and consists of a perceptive (receptive) apparatus, pathways and a part of the brain where higher analysis and synthesis of information about odors is carried out. The perceptive apparatus of the analyzer is located in the initial section of the airways - in the olfactory part of the nasal cavity. This is a relatively small area, the mucous membrane stands out here with its swelling and pigment color, like in croup. and small horn. cattle, the horse is yellow, the pig is brown, the dog and cat are gray. In animals with a highly developed sense of smell (dogs), it can be folded. In this place, in the thickness of the mucous membrane, olfactory neurosensory cells lie, alternating with supporting (supporting) ones; they fit quite tightly to each other, forming the olfactory epithelium. The receptor layer of the olfactory lining is not continuous; it is interrupted deep in the folds. Here scattered small olfactory (Bowman's) glands open, secreting a secret that contains mucus, which protects the mucous membrane from drying out and dissolves odorous substances and thus makes them available for receptor perception. The process of smell perception begins with the olfactory receptor cell. Their number can reach 200 million in a dog, 100 million in a rabbit, 80 million in ungulates, and 40 million in humans. The shape of the olfactory cells resembles a spindle with two processes: one is short, peripheral, directed to the surface of the mucous membrane, the other is long, central - into the brain. The peripheral processes have a thickening at the end in the form of a club with 10-12 thin hairs - cilia. These cilia are extremely mobile: they bend, straighten, and turn in different directions, as if searching for and capturing molecules of odorous substances. Receptor sites have been found on olfactory cilia that have a special structure and properties, due to which they come into contact only with certain odorous molecules. As a result of such contact, a nerve impulse is born in the receptor cell, which travels along the central process to the brain. The central processes form 15-20 olfactory nerves. The olfactory nerves penetrate the cranial cavity through the holes of the perforated plate of the ethmoid bone, reaching the next section of the olfactory analyzer - the olfactory bulbs. The olfactory bulb is a complexly organized center where preliminary processing of all information about smell is carried out. From the bulbs along two olfactory tracts, through the olfactory triangles, signals enter the pyriform lobes (secondary olfactory centers), the hippocampus (higher subcortical olfactory centers) and the cortex of the temporal lobe of the brain, where the higher part of the olfactory brain is located and where, after final processing and synthesis of information a sensation of a particular smell is formed.
5) The visual analyzer perceives the size, shape, color of objects in the external world, their location in space, movement, etc. The perceptive department of the visual analyzer is the organ of vision (organon visus), which consists of the eye and protective and auxiliary devices (orbit, periorbita, conjunctiva, eyelids, lacrimal apparatus and eye muscles). The eye or eyeball is a paired spherical optical organ. Nocturnal animals have the largest eyeballs. Among domestic animals, cats have the largest eyes in relation to body size, followed by dogs. In underground animals, due to the reduction of the organs of vision, the eyeballs are very small and almost completely hidden under the skin (mole, shrew). The visual axes located in the orbits of the eyes also have different directions in animals. When the visual axes of both eyes approach each other, i.e. As the angle between them decreases, the field of vision of one eye overlaps the field of vision of the other eye. This achieves high-quality binocular vision. With more primitive monocular vision, both fields of vision are independent of each other, and as a result, the field of vision is much larger, but of lower quality. The visual angle (between both visual axes) is: for a hare - 170o, for a horse - 137o, for a pig - 118o, for a dog - 93o, for a cat - 77o, in a person - 14o, in a lion - 10o. These values are determined by the way of life of animals - some need a large field of vision in order to escape in time (hare, horse), while others, on the contrary, need the quality of vision for accurate orientation when catching prey (cat, lion).
The wall of the eyeball is formed by three membranes. The outer (fibrous) membrane or sclera, making up 4/5 of the entire circumference of the eye, is the thickest and strongest; it provides the eyeball with a certain shape and consists mainly of collagen fibers. Only in the anterior section is a tiny window, as it were, cut into the sclera - the cornea. At the border of the sclera and cornea there is a groove - the limbus. The network of capillaries located in the limbus provides nutrition to the cornea, which does not have its own blood vessels, which largely determines its absolute transparency. Adjacent to the outer shell is the choroid, which consists of the choroid proper, the ciliary body and the iris. The iris is located behind the cornea and contains cells called myopigmentocytes, which determine its color and can dilate or constrict the pupil. The pupil is a small hole in the center of the iris. Its shape differs between species: in dogs, pigs and primates it is round, in cats it is in the form of a vertical slit, in herbivores it is transverse oval. The iris is separated from the choroid proper by the ciliary or ciliary body. In its thickness is the ciliary muscle, when it contracts, the ligaments that hold the lens relax and it becomes more convex. And when the ciliary muscle relaxes, the ligaments, on the contrary, tighten, which leads to some flattening of the lens. Thus, the ciliary body provides focusing of vision, without which it is impossible to distinguish objects located at a distance. The inner layer of the ciliary body, rich in blood vessels, produces intraocular fluid that enters the chambers of the eye (anterior and posterior). This fluid provides nutrition to the cornea, lens and vitreous body. The lens, vitreous body and intraocular fluid make up the optical or refractive system of the eye. Inside the choroid proper, herbivores and predators have a reflective zone (tapetum), which has a crescent shape and a blue-green color. Thanks to it, the eyes glow in the dark and have the ability to see in reflected light. The innermost of the three shells is the reticular one. As the ancient Greek scientist Herophilus , “the retina is a tightened fishing net, thrown to the bottom of the eye glass and catching the sun’s rays.” In the photoreceptor layer of the retina (and there are 10 layers in total) there are light-receiving elements: highly specialized cells with processes in the form of rods and cones. Rods provide twilight vision, while cones are adapted to daylight and perceive colors. Moreover, rods are much more sensitive than cones. Thanks to them, we see quite well in the dark, but we cannot distinguish colors: as you know, all cats are gray at night. The ability of the eye to perceive different colors is provided by three types of cones: red-, blue- and green-sensitive. Therefore, normal human vision is called three-dimensional, or trichromatic. As for colorblind people, who cannot distinguish between red and green, they do not have green-sensitive or red-sensitive cones in their retina. Color vision is not expressed in all animals. A horse distinguishes between red, green, yellow, blue and violet, a cow and a pig - red, yellow, green and blue. The dog can clearly distinguish up to 50 shades of gray from black to white, and there is evidence that dogs are able to distinguish the color green. As for birds, most of them have color vision. Cones and rods are connected through intermediate bipolar cells to large ganglion cells that give rise to nerve fibers. Collecting into a bundle, these fibers form the optic nerve, which leaves the eyeball and goes to the brain. The optic disc, the place where the fibers exit, is clearly visible when examining the fundus. There are no rods and cones here, so light is not perceived by this part of the retina and the spot is called a blind spot. And almost next to it there is another oval-shaped spot, called yellow. This is the place of best vision, since the retina is thinnest in the area of the macula. Thus, the retina of the eye is the perceptive part of the visual analyzer; conductive - 2 pairs of cranial (optic) nerves and optic tracts; central - the lateral geniculate body (thalamus), the visual hillocks of the quadrigeminal region and the occipital lobes of the cerebral cortex.
6) The equilibrium auditory analyzer is designed to perceive the sounds of the external world and the position of the body in space. The greatest hearing acuity is observed in predatory animals (dogs, cats), average - in primates, and some animals are even able to perceive ultrasound (bats, whales, dolphins). The perceptive section of the statoacoustic analyzer is represented by the vestibulocochlear organ (organum vestibulocochleare). The organ of hearing and balance is divided into three parts: the outer ear, the middle ear and the inner ear. The outer ear serves to capture sound vibrations and consists of the auricle, its muscles and the external auditory canal. The basis of the auricle is elastic cartilage covered with skin. The external auditory canal is a canal that begins with the external auditory opening and ends with the eardrum. Its wall contains sebaceous glands, as well as sulfur glands that secrete earwax. In cattle and pigs, the external auditory canal is long, while in horses and dogs it is short. The eardrum is made of dense connective tissue (collagen fibers) and separates the outer ear from the middle ear. It is absent in cetaceans.
The middle ear is a sound-conducting section and is located in the tympanic cavity, which is filled with air and connected to the pharynx through the auditory tubes. Through these pipes, the air pressure in the tympanic cavity is balanced with atmospheric pressure. The horse has a sac-like protrusion in the area of the auditory tube - an air sac with a capacity of 450 cm3. The middle ear contains 4 auditory ossicles (hammer, incus, lentiform bone and stapes), which are connected by joints and ligaments. The malleus is fused to the eardrum. Vibrations of the membrane, arising under the influence of sound waves, are transmitted to the malleus, from it to the incus, then to the lenticular bone and from it to the stapes. The base of the stapes is movably inserted into an oval-shaped window, “cut out” on the inner wall of the tympanic cavity. This wall separates the tympanic cavity from the inner ear. Through the chain of these bones, sound vibrations, amplified 22 times, are transmitted from the eardrum to the wall of the inner ear, behind which there is a specific fluid (perilymph), which is also capable of vibrating.
The inner ear consists of a bony labyrinth and a membranous labyrinth located within it. The bone labyrinth is a system of hollow bone formations that are located deep in the temporal bone. It is divided into three parts: the vestibule, semicircular canals and cochlea. The membranous labyrinth approximately follows the shape of the bony labyrinth and is a set of interconnected cavities filled with endolymph fluid. The soft walls of the membranous labyrinth react very sensitively to vibrations of the perilymph, which surrounds them from the outside, and transmit them to the endolymph, which in turn also begins to vibrate. The membranous labyrinth is conventionally divided into two parts: auditory and vestibular.
The auditory part is represented by the membranous cochlea. The number of its turns (turns) depends on the type of animal, for example, a horse and a rabbit have 2, cattle and dogs have 3, and a pig has 4. Inside the membranous cochlea there is a spiral organ (Organ of Corti), which is the sound-receiving part of the organ of hearing. . The main elements of the spiral organ are receptor cells that perceive sound stimulation. These cells are called hair (auditory) cells and are located between the supporting cells. In receptor hair cells, the physical energy of sound vibrations is converted into nerve impulses. The hair cells are approached by the sensitive endings of the auditory (cochlear) nerve, which perceive information about sound and transmit it further along the nerve fibers. The higher auditory center is located in the temporal lobe of the cerebral cortex: the analysis and synthesis of sound signals is carried out here.
The vestibular part of the membranous labyrinth is represented by the vestibule and semicircular membranous canals. In the vestibule, oval and round sacs are distinguished. On the walls of the sacs and canals there are small elevations - maculae - sensitive spots and ridges that contain receptor hair and supporting cells. Above these ridges and spots in the endolymph float calcite crystals - otoliths, which form the otolithic membrane. When this membrane is displaced, the receptor hair cells are irritated and a nerve impulse is generated, which is transmitted further along the nerve fibers of the vestibular (vestibular) nerve. Together with the fibers of the cochlear nerve, the vestibular nerve forms the 8th pair of cranial nerves - the vestibulocochlear nerve. Its fibers end in the vestibular nucleus of Deiters of the medulla oblongata. The axons of the cells of this nucleus begin the central pathways of the vestibular analyzer, which reach the cerebellum and the cortex (temporal lobe) of the brain.
Phylogeny of sense organs.
The sense organs are of ectodermal origin. In invertebrates, they are mainly represented by sensitive cells, which are located in the epidermis and are associated with receptor nerve endings.
The lancelet has light-sensitive cells (ocelli of Hesse), an olfactory fossa and sensory cells on the oral tentacles.
Cyclostomes develop paired visual organs - eyes, have an olfactory capsule and a lateral line organ appears that perceives the movement of water.
In fish, taste organs are formed in the oral and pharyngeal regions, there are olfactory pits, eyes develop (rods and cones appear in the retina and the lens) and a lateral line organ.
In amphibians, an organ of smell arises, and taste buds form taste buds, an organ of hearing appears, and the lateral line organ gives rise to the inner ear.
Reptiles develop turbinates, where the sense of smell is located; cones develop in the retina of the eye, the lens can change curvature; the organ of hearing and balance is formed.
In birds and mammals, the sense organs reach their greatest development.
Lecture No. 11 ENDOCRINE APPARATUS
The concept of the endocrine apparatus and its constituent elements. General anatomical and physiological features of the endocrine and mixed secretion glands. Classification
iron Thyroid
The concept of the endocrine apparatus. Control of the functioning of the digestive, respiratory, reproductive organs... is provided not only by the nervous system, but also by the endocrine apparatus, which includes the endocrine and mixed secretion glands
, producing biologically active substances - hormones. Hormones (Greek hormao - move, excite) enter directly into the blood and lymph and have a regulating effect on the development of cells, tissues, organs and the whole organism. The endocrine apparatus (endo - inside, crino - secrete) includes endocrine and mixed secretion glands, as well as the diffuse endocrine system. In addition, there are a number of organs that perform an endocrine function, but for them it is not the main one.
| Endocrine glands | Glands of mixed secretion | Organs that produce hormone-like substances | Diffuse endocrine system |
| Pituitary | Pancreas (pancreatic islets) | Thymus – thymosin – on the immune system | APUD-syst parafollicular cells shield. yellow; brain cells. adrenal gland; neurosecretory cells of the hypothalamus; pinealocytes of the pineal gland; heads parathyroid cells parathyroid. yellow; endocrine cells of the pituitary adenophysis; placentas; pancreas gastrointestinal tract |
| Pineal gland | Gonads (interstitial tissue) | Kidneys – renin – for water-salt metabolism | |
| Thyroid | Stomach - secretin - increases the secretion of pepsin | ||
| Parathyroid | Intestines - gastrin - stimulates the secretion of the pancreas | ||
| Adrenal gland | Placenta - gonadotropin - increases the number of maturing eggs | ||
| Heart – auriculin – for water-salt metabolism | |||
| Spleen |
Despite the differences in origin, shape, size and location, the endocrine glands have common anatomical and physiological features:
1. All endocrine glands are compact organs, i.e. have stroma and parenchyma. The stroma is represented by a capsule and trabeculae, which are built from connective tissue. Parenchyma, the working tissue of the gland, is built from epithelial or nervous tissue.
2. Endocrine glands do not have excretory ducts and therefore secrete hormones directly into the blood or lymph.
3. The endocrine glands are abundantly supplied with blood and have a well-defined network of capillaries, which along their course form extensions - sinusoids. In the sinusoids, the blood flow slows down and, as a result, the metabolism between the blood and the gland tissue improves. The peculiarity of the blood supply and innervation of the endocrine glands ensures the rapid entry of hormones into the blood or lymph and their distribution in the body.
4. The endocrine glands are characterized by the merocrine type of secretion, i.e., the release of hormones occurs without destroying the integrity of the gland cells.
5. In the endocrine apparatus, the glands do not function in isolation, but under the direct influence of the central nervous system, especially the hypothalamus. Neurosecretory cells (nuclei) of the hypothalamus secrete special neurohormones that affect the pituitary gland. In turn, the pituitary gland, which is the central gland of the endocrine apparatus, secretes crinotropic hormones, which activate the activity of almost all other glands.
Hypothalamus
Neurohormones
Pituitary
Crinotropic hormones
1) pineal gland 2) thyroid 3) cortex 4) interstitial tissue
adrenal gland gonads
Thus, the central nervous system influences the activity of the endocrine apparatus through the pituitary gland, as well as through the nerves going to the glands.
What side effect do we get?
Our nervous system forgets how to slow down on its own. What does this mean?
When external disturbance or change occurs, we change and cannot stop for a long time. We get used to “drinking the problem down” or “smoking.”
If we don't have access to a drug (alcohol), we become overstimulated. The motors of the psyche continue to work at full speed when this is no longer necessary. Imagine, the conflict has long ended or the problem has been resolved, but you continue to be in an overexcited state for several hours or even several days (this is quite realistic).
And all because your psyche has forgotten how to use “inhibition”.
This is also the difficulty of getting out of addiction.
If you want to learn even more about this, read my previous article “The Effects of Alcohol on the Nervous System.”
- Now it seems to you that in order to “relieve tension” (slow down), you need to “drink.”
- By drinking, you even more forget how to “slow down” and calm down naturally without the use of alcohol.
- The situation is getting worse.
Autonomic ganglia
Ganglia are nerve nodes. The autonomic ganglia help distribute electrical signals efficiently. One or more preganglionic nerve fibers approach one ganglion, which transmit signals from the “higher” system. And postganglionic neurons depart from the ganglion, transmitting excitation or inhibition further along the network. This universal system allows you to fully control all processes in the body.
In the ganglia of the excitatory nerve network, the presynaptic fiber regulates up to 30 nerve cells connected to the ganglion. And in the parasympathetic there are only 3 or 4 neurons.
Vegetative nodes are found in all tissues and organs, as well as in the glands of internal and external secretion. The neurons of the MHC network are extremely diverse, but each consists of an axon, a nucleus, and a dendrite.
Important Haptophobia - fear of being touched
Dendrite - from Latin - tree-like. From the name it is clear that this part of the neuron transmits signals through a highly branched network of small fibers. In the enteric system, for example, each neuron has many dendrites.
Some fibers have a myelin sheath, which improves conductivity and speeds up the signal.
Meaning of MHC
In medicine, the study of ganglion nodes of internal organs is important for the study of diseases associated with impaired organ development. One such disorder is Hirschsprung's disease. MHC is responsible for feeding organ cells and blood circulation in the internal muscle layers of organs.
One more important detail. Due to the fact that reflex arcs are present in the intraorgan system, it has the ability to work without the constant “guidance” of the central nervous system. What is a reflex arc? This is a chain of neurons that allows you to quickly transmit a pain signal and receive an immediate response to receptor irritation.
Enterometasympathetic system
The enteric nervous system is a unique mechanism where thousands of neurons are completely coordinated with each other. This mechanism, created by nature, is rightfully considered the second human brain. Because even if the vagus nerve, which is connected to the brain, is damaged, the system continues to perform all its functions, namely: digesting food and absorbing nutrients.
But it turns out that the digestive tract is not only responsible for the digestion of food, but, according to the latest data, also for the emotional background of a person. It has been established that the intestines produce 50% of dopamine, the hormone of joy, and about 80% of serotonin. And this is even more than is produced in the brain. Therefore, the intestines can safely be called the emotional brain.
In the enteric autonomic metasympathetic system, several types of neurons are distinguished:
- primary sensory afferents;
- ascending and descending interneurons;
- motor neurons.
Motor neurons, in turn, are divided into moving muscles, excitatory and inhibitory.
Intestinal peristaltic reflex and MHC
The small and large intestines also have an autonomous metasympathetic division of the autonomic nervous system. It is known that each villi of the large intestine contains 65 sensory neurons; Each millimeter of tissue contains 2,500 different nerve cells.
Sensory neurons are integrated with motor neurons through various interneurons in the enteric system. It is enough for one neuron to be activated to trigger alternating tension and relaxation of the intestinal muscles further along the chain. This is called the peristaltic reflex, which moves food through the intestines. The intestinal autonomic system is also completely independent of the central nervous system, which is vital if, in the event of a stroke, for example, part of the brain stops functioning.
What is a synapse?
A synapse is a special structure that ensures the transmission of a nerve impulse from a nerve fiber to another nerve fiber or nerve cell, and in order for a nerve fiber to be affected by a receptor cell (the area of contact between nerve cells and another nerve fiber), two nerve cells are required .
A synapse is a small section at the end of a neuron. With its help, information is transferred from the first neuron to the second. The synapse is located in three areas of nerve cells. Also, synapses are located in the place where the nerve cell enters into connection with different glands or muscles of the body.
Intrauterine development of the central nervous system
The importance of the nervous system is to ensure the functioning of internal organs, intellectual function, motor skills, sensitivity and reflex activity. The child’s central nervous system develops not only during the prenatal period, but also during the first year of life. Ontogenesis of the nervous system begins from the first week after conception.
The basis for brain development is formed already in the third week after conception. The main functional nodes are identified by the third month of pregnancy. By this time, the hemispheres, trunk and spinal cord have already been formed. By the sixth month, the higher parts of the brain are already better developed than the spinal part.
By the time a baby is born, the brain is the most developed. The size of the brain in a newborn is approximately an eighth of the child’s weight and ranges from 400 g.
The activity of the central nervous system and PNS is greatly reduced in the first few days after birth. This may include an abundance of new irritating factors for the baby. This is how the plasticity of the nervous system manifests itself, that is, the ability of this structure to be rebuilt. As a rule, the increase in excitability occurs gradually, starting from the first seven days of life. The plasticity of the nervous system deteriorates with age.
Functions of the metasympathetic division of the ANS
The MHC is a relatively independent department of interconnected neurons that regulates the functioning of internal organs:
- preserves the absorption capacity of the intestines and intestines;
- regulates heart contraction;
- affects contractions of the ureter, cervix, etc.;
- innervates and controls the activity of all organs in standard conditions and in pathologies of the spinal cord;
- provides constant regulation of organ functions.
MS affects the activity of cardiac muscle tissue, smooth muscle structures and glandular epithelium. Areas or strips of the uterus, bladder, and gall bladder contract with the range and amplitude that is characteristic of each organ.
Microglia of this system are found in the stomach, kidneys, intestines, bronchi and other areas. The structure plays a significant role in lesions and dysfunctions of organs. In case of damage to the spinal nerve canal, many internal organs undergo failure and are restored after six months due to the presence of the metasympathetic network.
All reflexes of the system are controlled by the autonomic centers of the telencephalon - the striatum, as well as the hypothalamus, the structure of the midbrain.
The gastrointestinal tract, more clearly than other systems, displays the main characteristics of the MNS - it is there that it has been studied to a greater extent. Here it regulates complex intestinal motility - peristalsis.
The structure of the gastrointestinal tract includes various formations - muscle tissue, mucosal surfaces, endocrine and lymph nodes.
The local MHC regulates all these structures with the participation of other parts of the autonomic system. Thanks to this, the functionality of the gastrointestinal tract is not greatly affected by disruptions in the activity of parasympathetic and sympathetic nerve tissues.
Methesympathetic nervous system. What is this?
Until recently, only 2 parts of the nervous system were distinguished - sympathetic and parasympathetic. The first, as you know, is responsible for mobilizing the body, and the second for relaxation and rest. But when scientists noticed that each organ has its own rhythm of movement and its own separately functioning microganglia, they decided to isolate another system - the metasympathetic one.
This is a completely independent formation that has reflex arcs at its disposal. Each hollow organ has its own ganglion network: in the kidneys, stomach, uterus, intestines, and in the prostate gland, men also have their own nerve plexuses. Moreover, some networks are still poorly understood, so we can only speculate about how complex they are organized.
The entire autonomic nervous system (sympathetic, parasympathetic, metasympathetic divisions) is designed to control homeostasis, that is, the constancy of the internal environment. If there are no failures in the autonomic nervous system, then the metabolism is perfectly adjusted, the lymphatic and circulatory systems are functioning properly.
After damage to the spinal central nerve canal, all internal organs, such as the bladder and intestines, gradually recover after experiencing shock. The organs are rebuilt and begin to function fully again after 5–6 months. This happens thanks to another nervous system embedded in their muscle walls—the metasympathetic.
Features of the structure of the PNS
Thanks to the PNS, the activity of the entire human body is regulated. The PNS consists of cranial and spinal neurons and fibers that form ganglia.
The human peripheral nervous system has a very complex structure and functions, so any slightest damage, for example, damage to blood vessels in the legs, can cause serious disruptions to its functioning. Thanks to the PNS, all parts of the body are controlled and the vital functions of all organs are ensured. The importance of this nervous system for the body cannot be overestimated.
The PNS is divided into two divisions - the somatic and autonomic PNS systems.
The somatic nervous system performs double duty - collecting information from the sensory organs, and further transmitting this data to the central nervous system, as well as ensuring the motor activity of the body by transmitting impulses from the central nervous system to the muscles. Thus, it is the somatic nervous system that is the instrument of human interaction with the outside world, as it processes signals received from the organs of vision, hearing and taste buds.
The autonomic nervous system ensures the functions of all organs. It controls the heartbeat, blood supply, and breathing. It contains only motor nerves that regulate muscle contraction.
Important Anankasty personality disorder
To ensure the heartbeat and blood supply, the efforts of the person himself are not required - this is controlled by the autonomic part of the PNS. The principles of the structure and function of the PNS are studied in neurology.
Diseases of the autonomic nervous system (ANS)
Autonomic nervous system
Autonomic nervous system
(from Lat. vegetatio - excitement, from Lat. vegetativus - plant),
ANS
,
autonomic nervous system
,
ganglion nervous system
(from Lat. ganglion - nerve ganglion), visceral nervous system (from Lat. viscera - insides), organ nervous system, splanchnic nervous system,
systema nervosum autonomicum
(PNA) - part of the body’s nervous system, a complex of central and peripheral cellular structures that regulate the functional level of the body, necessary for the adequate response of all its systems.
The autonomic nervous system is a section of the nervous system that regulates the activity of internal organs, endocrine and exocrine glands, blood and lymphatic vessels. Plays a leading role in maintaining the constancy of the internal environment of the body and in the adaptive reactions of all vertebrates.
Anatomically and functionally, the autonomic nervous system is divided into sympathetic, parasympathetic and metasympathetic. The sympathetic and parasympathetic centers are under the control of the cerebral cortex and hypothalamic centers.
The sympathetic and parasympathetic divisions have central and peripheral parts. The central part is formed by the bodies of neurons lying in the spinal cord and brain. These clusters of nerve cells are called vegetative nuclei. Fibers extending from the nuclei, autonomic ganglia lying outside the central nervous system, and nerve plexuses in the walls of internal organs form the peripheral part of the autonomic nervous system.
The sympathetic nuclei are located in the spinal cord. The nerve fibers extending from it end outside the spinal cord in the sympathetic ganglia, from which the nerve fibers originate. These fibers are suitable for all organs.
The parasympathetic nuclei lie in the midbrain and medulla oblongata and in the sacral part of the spinal cord. Nerve fibers from the nuclei of the medulla oblongata are part of the vagus nerves. From the nuclei of the sacral part, nerve fibers go to the intestines and excretory organs.
The metasympathetic nervous system is represented by nerve plexuses and small ganglia in the walls of the digestive tract, bladder, heart and some other organs.
The activity of the autonomic nervous system does not depend on the will of a person. This means that under normal conditions a person cannot force his heart to beat less often or his stomach muscles not to contract. However, it is possible to achieve conscious influence on many parameters controlled by the ANS using special training methods - for example, using biofeedback methods.
The sympathetic nervous system enhances metabolism, increases the excitability of most tissues, and mobilizes the body's forces for vigorous activity. The parasympathetic system helps restore spent energy reserves and regulates the functioning of the body during sleep.
The organs of circulation, respiration, digestion, excretion, reproduction, as well as metabolism and growth are under the control of the autonomous system. In fact, the efferent section of the ANS carries out nervous regulation of the functions of all organs and tissues, except for skeletal muscles, which are controlled by the somatic nervous system.
Unlike the somatic nervous system, the motor effector neuron in the autonomic nervous system is located in the periphery, and the spinal cord only indirectly controls its impulses.
Terms autonomous system
,
visceral system
,
sympathetic nervous system
are ambiguous. Currently, only part of the visceral efferent fibers is called sympathetic. However, different authors use the term "sympathetic" in different ways:
- in the narrow sense, as described in the sentence above;
- as a synonym for the term "autonomous";
- as the name of the entire visceral (“autonomic”) nervous system - both afferent and efferent.
Have there been any cases of miraculous healing in your practice?
Law of Opposites
Ensuring the existence of the human body requires the ability to adapt. Different situations may require opposite actions. For example, when it’s hot you need to cool down (sweating increases), and when it’s cold you need to warm up (sweating is blocked). The sympathetic and parasympathetic sections of the autonomic nervous system have opposite effects on organs and tissues; the ability to “turn on” or “turn off” one or another influence allows a person to survive. What effects does activation of the sympathetic and parasympathetic divisions of the autonomic nervous system cause? Let's find out.
Sympathetic innervation provides:
- dilation of the pupil, widening of the palpebral fissure, “protrusion” of the eye forward;
- decreased salivation, saliva becomes thick and viscous;
- increased heart rate;
- increased blood pressure;
- dilatation of the bronchi, decreased mucus secretion in the bronchi;
- increased breathing rate;
- slowing down intestinal motility;
- decreased secretion of digestive glands (stomach, pancreatic juice);
- stimulation of ejaculation;
- vasoconstriction;
- raising of skin hairs (“goose bumps”).
Parasympathetic innervation acts as follows:
- constriction of the pupil, narrowing of the palpebral fissure, “retraction” of the eyeball;
- increased salivation, there is a lot of saliva and it is liquid;
- reduction in heart rate;
- decreased blood pressure;
- narrowing of the bronchi, increased mucus in the bronchi;
- decreased breathing rate;
- increased peristalsis up to intestinal spasms;
- increased secretion of the digestive glands;
- causes erection of the penis and clitoris.
There are exceptions to the general pattern. There are structures in the human body that have only sympathetic innervation. These are the walls of blood vessels, sweat glands and the adrenal medulla. Parasympathetic influences do not apply to them.
Typically, in the body of a healthy person, the influences of both departments are in a state of optimal balance. There may be a slight predominance of one of them, which is also a variant of the norm. The functional predominance of excitability of the sympathetic department is called sympathicotonia, and the parasympathetic department is called vagotonia. Some periods of human age are accompanied by an increase or decrease in the activity of both departments (for example, activity increases during adolescence, and decreases during old age). If there is a predominant role of the sympathetic department, then this is manifested by sparkle in the eyes, wide pupils, a tendency to high blood pressure, constipation, excessive anxiety and initiative. The vagotonic effect is manifested by narrow pupils, a tendency to low blood pressure and fainting, indecision, and excess body weight.
Thus, from the above it becomes clear that the autonomic nervous system with its oppositely directed sections ensures human life. Moreover, all structures work in harmony and coordination. The activity of the sympathetic and parasympathetic departments is not controlled by human thinking. This is exactly the case when nature turned out to be smarter than man. We have the opportunity to engage in professional activities, think, create, leave ourselves time for small weaknesses, being confident that our own body will not let us down. Internal organs will work even when we are resting. And this is all thanks to the autonomic nervous system.
Educational film “The Autonomic Nervous System”
https://youtube.com/watch?v=BT6h2aiwVg4