Group of neurodegenerative diseases
This group of diseases is characterized by damage to the central nervous system. A certain number of neurons die, and this leads to neurological pathologies. Neurodegenerative diseases can have different causes and different clinical manifestations. It is characteristic that all diseases in this category are incurable.
All therapy used is symptomatic. That is, it alleviates the manifestation of the disease, but does not in any way contribute to the regeneration of damaged areas. The most effective would be a transplantation of nerve tissue, but the method has both technical and moral obstacles. Similar diseases include Alzheimer's, Parkinson's, and Farah's diseases.
https://www.youtube.com/watch?v=https:accounts.google.comServiceLogin
A group of similar diseases is characterized by manifestations of central nervous system lesions. A certain number of neurons die, which leads to the development of neurological pathologies. Neurodegenerative diseases can occur for a variety of reasons and also have different clinical manifestations. A characteristic feature of all diseases from this group is their incurability. All therapeutic actions performed are symptomatic.
That is, therapy is aimed at alleviating the symptoms of the disease, but in no way can affect the regeneration of areas that are damaged. The most effective treatment would be tissue transplantation, but this method has several limitations, primarily technical and moral.
The most famous diseases of this group are Alzheimer's disease, Parkinson's disease, and Fahr's syndrome. Early diagnosis of these diseases is often difficult. In the diagnostic process, doctors mainly take into account patients' complaints and observe their behavior. The most modern and effective method for diagnosing diseases of this group is tomography, both computed tomography and magnetic resonance imaging.
Inheritance of Fahr syndrome
Since this disease is a rather rare phenomenon, it is difficult for specialists to provide the correct clinical picture of the syndrome. Symptoms may appear if the patient is over 40 years of age. In younger people, Farah's disease symptoms may be vague and vague. Patients have impaired coordination of movement and parkinsonism.
Also, the development of the disease may be indicated by such signs as tremor, dystonia, rapid and erratic movements of the limbs (chorea), involuntary contractions of the hands and feet. Since the disease affects areas of the brain, performance and mental capabilities decrease. A person’s memory also suffers.
Speech is often impaired. Other neurological signs include pain and mental disorders. There is a juvenile form of the disease, which manifests itself in children and adolescents. The main symptoms are: dystonia, chorea, epileptic seizures. The senile form is typical for middle-aged and older people. In this case, parkinsonism, speech disorders, and other problems in the functioning of the nervous system are observed. Urinary incontinence may also occur.
The reasons why the disease may develop have not been precisely established. However, it is known that disorders of the thyroid and parathyroid glands have a huge impact on its occurrence. In this case, disruptions occur in the metabolic processes of calcium and phosphorus. Similar neurodegenerative diseases can also occur when the acid-base balance in the body is disturbed.
Eye diseases and symptoms
Amblyopia
Amblyopia is a functional vision disorder that cannot be treated with glasses or contact lenses. With this disease, vision deterioration occurs irrevocably: contrast perception and accommodation capabilities are impaired. Amblyopia can occur in one eye or both at the same time. It is characterized by the following symptoms:
- vision in one or both eyes decreases;
- difficulties arise with visualizing three-dimensional objects;
- problems arise in measuring visual distance to objects;
- the process of receiving visual information deteriorates.
Amblyopia most often develops in childhood. This disease is otherwise called “lazy eye”. Due to a number of eye diseases (astigmatism, myopia, cataracts, corneal opacity, etc.), vision is reduced in one eye, and the brain turns it off from the vision process, perceiving information from only one eye. It is important to notice this situation in time and begin treatment, otherwise it will be impossible to restore vision to the eye in adulthood.
Astigmatism
With astigmatism, due to the irregular shape of the cornea of the eye (normally it has a spherical shape, and in the case of astigmatism, it is shaped like a melon or a rugby ball), the refraction of light rays occurs incorrectly (instead of one, two foci are formed), and the perception of the surrounding world is disrupted. With corneal astigmatism, vision problems arise due to the abnormal structure of the cornea. With lens-type (lenticular) astigmatism, vision deteriorates due to changes in the lens.
Astigmatism is characterized by the following symptoms:
- “blurry” visualization of objects (uneven edges, unclear contours);
- feeling of double vision;
- the need to constantly strain your eyes to focus on the subject;
- headaches arising from constant overstrain of the visual apparatus;
- frequent squinting.
In childhood, astigmatism can lead to amblyopia (“lazy eye”) and requires treatment with optical and hardware methods. In adults (after 18 years of age), it is possible to correct astigmatism using laser vision correction.
Blepharitis
Blepharitis is a lesion of the eyelids that occurs due to the development of inflammation. There are several types of the disease. The most common diagnosis is chronic blepharitis, which is difficult to treat with medications. Blepharitis may be associated with other diseases of the visual system, such as ocular tuberculosis and conjunctivitis. It is often accompanied by purulent lesions of the eyelids and loss of eyelashes.
Treatment is carried out by taking antibiotics. Before a course of therapy, serious diagnostics are carried out to identify the root causes of the disease.
Main symptoms of blepharitis:
- feeling of swelling on the eyelids;
- severe itching;
- eyelash loss;
- feeling of dry skin around the eyes;
- burning and feeling of “sand” in the eyes;
- peeling of the skin on the eyelids;
- the appearance of ulcers and crusts;
- decreased vision;
- photophobia.
Myopia (nearsightedness)
Myopia is a disease characterized by impaired refraction of the eyes. The patient is unable to see in detail objects located at a great distance from him. The cause of visual impairment is improper fixation of rays on the retina. They lie not on the retina itself, but in front of it. Because of this, the picture is blurred. Pathological refraction of rays in the visual system is manifested by the following symptoms:
- inability to clearly see objects located at a distance;
- frequent pain in the temples and forehead;
- burning sensation in the eyes.
Myopia is corrected with glasses or contact lenses, and if the patient does not want to wear them, surgery is performed using an excimer laser.
Glaucoma
Glaucoma is a chronic disease of the visual system. The reason is increased intraocular pressure. It leads to dysfunction of the optic nerves and their damage. The optic nerves are not restored - the process of vision loss in this case is irreversible. There are two forms of glaucoma:
- open angle;
- closed angle.
The consequences of glaucoma depend on the nature of its course and the individual characteristics of the human visual system. Acute glaucoma can cause permanent loss of vision. Treatment is carried out by an ophthalmologist together with a neurologist.
With glaucoma, the patient experiences the following dysfunctions:
- dark objects appear before your eyes;
- lateral vision deteriorates;
- decreased ability to see in the dark;
- image clarity decreases;
- “rainbow” shimmers appear when looking at lamps, the sun and other light sources.
Despite the listed signs, glaucoma is a very insidious disease that does not manifest itself in any way in the initial stages of development. Therefore, it is necessary, especially after 40 years, to visit an ophthalmologist at least once a year. Today there are many ways to reduce eye pressure and treat glaucoma: medication, laser and surgical treatment.
Farsightedness (hypermetropia)
Farsightedness is a disease associated with refractive error in the visual system. Light rays are focused not on the retina, as should normally happen, but behind it. With farsightedness, a person has difficulty distinguishing between objects located both at a close distance and at a distance from it.
Farsightedness can be manifested by the following symptoms:
- asthenopia;
- strabismus;
- poor fixation during binocular vision;
- increased eye fatigue;
- regular headaches;
- feeling of fog before the eyes.
At a young age, patients may not notice farsightedness, because the lens of the eye is still elastic and is able to change its shape, adjusting to work both near and far, thereby compensating for farsightedness. And with age, this problem will worsen vision.
Cataract
Cataracts occur due to complete or partial clouding of the lens of the eye. It can affect one visual organ or both at the same time. The essence of the disease is that due to clouding of the lens, light rays cannot enter the eye, onto the retina. As a result, visual acuity decreases. In some cases, advanced cataracts lead to complete loss of vision.
Most often the disease occurs in older people. In young patients, the development of cataracts may be associated with previous somatic diseases or eye injuries. Medicine knows cases of congenital cataracts.
Main symptoms of cataracts:
- blurred vision;
- the emergence of a regular need to replace glasses;
- decreased vision at night;
- increased eye sensitivity to bright light;
- decreased ability to distinguish colors;
- sensation of a veil before the eyes, as if looking through foggy glass;
- halos around light sources;
- pain in the eyes when reading.
In some cases, cataracts can cause double vision in one eye when the other eye is closed.
Keratoconus
Keratoconus is a degenerative disease of the cornea. Normally its shape is spherical. As the cornea becomes thinner, it protrudes forward and takes the shape of a cone. This disease often occurs at a young age and leads to changes in optical properties. At the initial stage of the disease, it is possible to correct visual functions with the help of glasses, but the further the disease progresses, the more often it is necessary to select new glasses.
Keratoconus is characterized by the following symptoms:
- a sharp decrease in vision in one eye;
- reducing the clarity of the contours of objects;
- the appearance of halos around light sources when looking at them;
- increased eye fatigue;
- rapid development of myopia.
With keratoconus, the patient needs to regularly replace glasses with enhanced lenses. Vision deterioration can be stopped if you consult an ophthalmologist in time. Eye surgeons use several types of operations, primarily aimed at stopping the progression of keratoconus. At advanced stages, keratoplasty is performed - operations to replace the cornea of the eye with a donor one.
Keratitis
With keratitis, inflammation of the cornea of the eyeball develops and a feeling of cloudiness in the eyes occurs. The most common cause of keratitis is a viral infection. The disease can also develop as a result of eye injury. Damage to the cornea can spread to other areas of the visual system over time.
Keratitis occurs in several forms:
- light;
- moderate;
- heavy.
Based on the causes of occurrence, this disease is divided into:
- to exogenous - inflammation began due to exposure to external factors;
- endogenous - inflammation arose due to internal changes in the human body.
Keratitis is characterized by the following symptoms:
- photophobia;
- profuse lacrimation;
- redness of the eyelid and eyeball;
- blepharospasm (convulsive compression of the eyelid);
- loss of natural shine of the cornea;
- sensation of a foreign body in the eye.
Computer vision syndrome
Working at a computer for a long time can lead to the development of computer vision syndrome. This is the name for a set of pathologies of the visual system associated with eye strain in front of the monitor. To one degree or another, the syndrome manifests itself in 60% of personal computer users. It develops due to the specifics of the image on the monitor, incorrect ergonomics of the workspace and non-compliance with the correct mode of working at the computer.
The main symptoms of computer vision syndrome:
- decreased visual acuity;
- increased eye fatigue;
- tearfulness;
- photophobia;
- burning in the eyes;
- difficulty focusing on objects located near or far away;
- split image;
- dry eyes;
- redness and pain in the eyes.
The main problem when working at a computer is that the eyes are under constant tension and the person blinks very rarely - dryness occurs. Therefore, the recommendations of ophthalmologists are as follows: take breaks from work and use moisturizing drops.
Conjunctivitis
Conjunctivitis is an inflammation of the mucous membrane (conjunctiva) that covers the outer surface of the eyeballs and the adjacent surface of the eyelids. The disease can be of a different nature: viral, bacterial, allergic, chlamydial or fungal. Some types of conjunctivitis are contagious and can be transmitted from one person to another in everyday life. Infectious conjunctivitis is not a strong threat to the visual system, but in some cases it can cause serious complications.
Symptoms of conjunctivitis vary depending on the nature of the disease. Most often there are:
- swelling and redness of the eyelids;
- discharge of mucous and pus;
- increased tearfulness;
- burning sensation and itching.
Macular degeneration
The macula is the area that is located in the center of the retina of the eye. Small in size, it is responsible for image clarity and correct color perception. With macular degeneration (chronic pathology of the macula), visual functions decrease. The disease can occur in two forms: wet and dry. Both lead to vision impairment, but the wet form is considered more dangerous, as it is fraught with complete loss of central vision.
The main symptoms of macular degeneration:
- the appearance of a cloudy spot in the center of the visual field;
- loss of reading ability;
- deformation of lines and contours of the image.
Floaters in the eyes
Destruction of the vitreous body is a condition in which the patient experiences “floaters” in the eyes. The cause of visual impairment lies in local changes in the structure of the vitreous body, leading to the appearance of optically opaque particles. It is these particles that are perceived by the eye as floating “flies”. Destruction of the vitreous body does not pose a serious threat to vision, but causes some discomfort.
Symptoms of destruction usually appear in strong lighting. Along with “floaters”, small spots, threads or dots may appear that move within the boundaries of a person’s field of vision.
Retinal disinsertion
Retinal detachment is one of the most dangerous pathologies of the visual system. In the absence of timely surgical intervention, the disease can lead to complete loss of vision. Detachment of the retina from the deep pigment epithelial tissues of the choroid occurs for various reasons.
The main symptoms of retinal detachment:
- frequent appearance of glare and sparks before the eyes;
- the appearance of a veil that obscures the field of vision;
- reduction of image sharpness;
- deformation of the contours and appearance of objects visible to the eye.
To avoid this pathology, it is important to visit an ophthalmologist at least once a year to examine the fundus. If micro-tears or dystrophies are detected, such areas are attached to other membranes of the eye using a laser, thereby preventing ruptures and detachment.
Ophthalmic rosacea
Ophthalmic rosacea (rosacea) is a dermatological disease closely related to ophthalmology. It manifests itself as irritation and dry eyes, blurred vision. The image becomes blurry and blurry. The culmination of the disease is severe inflammation of the surface of the eyes. Ophthalmic rosacea can be one of the causes of keratitis.
With ophthalmic rosacea, the patient experiences the following symptoms in the eyes:
- dryness;
- itching;
- burning;
- redness;
- photophobia;
- discomfort;
- the appearance of barley;
- loss of eyelashes;
- terigum.
Often with rosacea, the upper eyelid becomes swollen and white particles in the form of dandruff appear on the eyelashes. Vision decreases, swelling occurs on the eyelids.
Presbyopia, or age-related farsightedness
We can say that these are age-related changes in the body due to the fact that with age the lens of the eye loses its elasticity and ability to accommodate (focus vision at different distances). Unfortunately, this process is inevitable and most people are forced to use glasses for working at close range, reading, etc.
Pterygium
Pterygium is a progressive eye disease that arises in the conjunctiva of the eyeball and spreads to other elements of the visual system. In its development, the pterygium can reach the center of the cornea. The disease is dangerous due to damage to the central optical zone, which can cause partial or complete loss of vision. The most effective treatment option for pterygium is surgery.
At the initial stage, the disease has no symptoms. In the future, a feeling of discomfort in the eyes, redness, swelling and itching may occur. Against the background of pterygium, visual acuity decreases and fog appears in the eyes.
The occurrence of pterygium is more typical for residents of southern countries.
Dry eye syndrome
Dry eye syndrome occurs due to impaired tear production and evaporation of fluid from the cornea. This disease occurs quite often nowadays. Often the disease is caused by progressive Sjogren's syndrome and other diseases that have a direct effect on reducing the amount of tear fluid. One of the reasons for the development of the syndrome is infection of the lacrimal glands.
Prerequisites for the development of dry eye syndrome also include eye burns, taking certain medications, and the development of oncological processes and inflammation in the body.
Working at a computer for a long time and staying in an air-conditioned room can also contribute to the development of this disease.
Symptoms of the disease:
- increased lacrimation;
- complete absence of tear fluid;
- redness of the eyes;
- feeling of discomfort in the eyes;
- development of photophobia;
- decreased clarity of vision;
- severe burning in the eyes.
Chalazion
Chalazion is an inflammation of the meibomian glands, which has the character of a tumor. The cause of the disease is blockage of the sebaceous glands, leading to their swelling. Swelling may occur due to the accumulation of excessive amounts of opalescent fluid. Chalazion can occur in people of any age. Externally, the tumor resembles a small ball under the skin. Over time, the disease can progress: the ball will increase in size, put pressure on the cornea and distort vision.
At the initial stage, the disease is characterized by swelling of the eyelids and the appearance of minor pain. Over time, a slight swelling appears on the eyelids. It does not cause discomfort or pain. Gray and red spots may appear on the inside of the eyelid.
Chemical burns to the eyes
Chemical burns to the eyes are one of the most dangerous eye injuries. A burn occurs when alkali or acid comes into contact with the eyeball. The level of damage depends on the type of substance, its quantity, temperature and exposure time. How deeply the substance penetrates inside the eye is also important. Burns are classified according to their form, from mild to severe. They can not only partially reduce visual acuity, but also cause complete loss. Therefore, at the first signs of burns, you should immediately contact an ophthalmologist.
Chemical burns are manifested by the following symptoms:
- severe pain in the eyes;
- redness of the eyelids and swelling;
- sensation of a foreign object in the eye;
- inability to fully open the eyelids.
Electroophthalmia
Electroophthalmia is a disease that develops due to damage to the eye by ultraviolet rays. Exposure can occur in various situations: while on vacation at sea, when working with electric welding without protective equipment, when walking on snow-covered mountain slopes without glasses.
Main symptoms of the disease:
- redness of the eyes;
- decreased visual abilities;
- nervousness;
- active lacrimation;
- discomfort in the eyes;
- strong photosensitivity.
Endocrine ophthalmopathy
Grace's ophthalmopathy (endocrine ophthalmopathy) is a disease that is autoimmune in nature and characterized by dystrophic infection of tissues. Most often, the pathology develops in patients with thyroid dysfunction.
The main symptoms of the disease are a feeling of tightness, dryness and pain in the eyes, swelling of the conjunctiva and periorbital part of the eye. In patients with endocrine ophthalmopathy, the eyeball is slightly convex.
Episcleritis
Episcleritis is an inflammation of the eye tissue located between the sclera and conjunctiva. At the initial stage, redness occurs in areas of the sclera located next to the cornea. Then a swelling forms at the site of inflammation. Most often, the disease goes away on its own, but relapses are possible.
Barley
Barley is an inflammation of the meibomian gland that is purulent in nature. Appears on the edge of the eyelid or on the hair follicle of the eyelashes. Barley can be internal or external. The cause of the disease is often a bacterial infection.
Barley is manifested by the following symptoms:
- redness of the edge of the eyelid;
- itching and swelling of the eyes;
- pain when touching the area of inflammation.
Sometimes it can be accompanied by headache, fever and general weakness.
Diagnostic methods
Before the advent of computed tomography, patients underwent X-ray examinations of the brain. Thanks to the advent of modern research methods, specialists received more informative pictures from the affected area. However, it is worth noting that computed tomography rather than magnetic resonance imaging has greater sensitivity for this clinical picture.
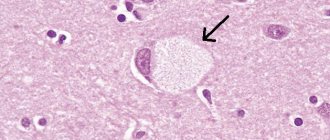
When analyzing most images, the affected areas are limited to the globus pallidus. They are small in size. Most often, the basal ganglia, thalamus, and cerebellum undergo changes. The level of calcification is approximately the same in young and elderly people. Also, no differences were found between groups in which Farah's disease is asymptomatic and those in which the syndrome is accompanied by pronounced symptoms.
When conducting a postmortem examination, the following picture is observed in the brain: the vessels have a whitish appearance (some branched areas). When touched by a knife, they make a sound similar to a crunch. For histological analysis, material is collected: sections of the cerebral cortex, basal ganglia, and cerebellum.
It is in the area of the latter that calcification occurs most often. The samples contain calcium salts. They are also most often detected on arteries (small, medium-sized) and capillaries. Less commonly (in isolated cases), Farah's disease affects the veins. Small calcium conglomerates are found along the entire length of the vessels, as well as in adjacent tissues. The presence of traces of arsenic, aluminum, cobalt, and mucopolysaccharides is also detected in the tissues.
Depending on whether Farah disease has symptoms, making a diagnosis can be somewhat more difficult. It is often diagnosed accidentally, when a tomography is performed to confirm a completely different disease. First of all, the specialist excludes calcium metabolism disorders and other developmental defects. Then a computed tomography scan (or x-ray examination) is prescribed.
Doctors note that one of the problems in making a correct diagnosis is hypoparathyroidism. This is a disease that occurs due to parathyroid hormone deficiency. As a result, the level of calcium in the blood decreases, and the level of phosphorus increases. If calcification of the striopallidodentate structures is observed on a CT scan, then additional tests are necessary to distinguish hypoparathyroidism from a condition such as Fahr's disease.
Treatment
To treat calcification, a therapeutic course is prescribed that will help cope with the underlying disease. So, if inflammation of an infectious nature has led to excessive calcium deposition, antibacterial drugs are prescribed.
If calcium absorption is impaired, medications containing magnesium, which is a calcium antagonist, are prescribed. Sufficient intake of magnesium from food and medications allows you to dissolve conglomerates and remove excess calcium from the body. During treatment, it is important to take diuretics, which will help speed up the process of excretion of the macroelement.
Vitamin D takes part in the process of calcium absorption, the excess supply of which also negatively affects the condition of the body. Therefore, during treatment, it is necessary to follow a special diet that excludes the consumption of large quantities of foods rich in calcium and vitamin D. These include fatty fish, leafy greens, dairy products, egg yolk, and nuts.
If conservative treatment methods are ineffective, as well as the formation of large conglomerates, their surgical removal is prescribed. The choice of surgical intervention method is carried out depending on the size of calcium accumulations, as well as their location.
Consequences
What are the consequences of Farah disease?
All of the listed characteristics are realized only if there is complete dominance, and for the appearance of the trait, only one gene of a dominant nature will be sufficient.
https://www.youtube.com/watch?v=ytaboutru
Based on the listed features of the type of inheritance through which Farah syndrome is transmitted, we can say that the presence of a diseased gene in the future father can cause the disease to manifest itself in the child. In order to determine the likelihood with which your child may inherit Farah disease, you should contact a genetics specialist who will conduct all the necessary studies and calculations and give a fairly accurate result.
Prevention
To prevent calcification of soft tissues and internal organs, special attention should be paid to proper nutrition. It is important to ensure a sufficient supply of all minerals and vitamins to the body in order to prevent the development of pathologies of various etiologies.
It is also important for people with congenital and acquired diseases of the cardiovascular system, kidneys, and endocrine pathologies to undergo regular scheduled examinations by specialists, which will help to promptly prevent the development of complications.
Treatment of various diseases should be carried out only under the supervision of a specialist and in accordance with his recommendations. Some groups of medications, including those for lowering blood cholesterol levels, blood pressure, as well as antibacterial and hormonal agents, can lead to an increase in calcium levels in the body and disruption of its metabolism.
To prevent calcinosis, you should lead an active lifestyle, which helps restore normal metabolism, and stop drinking alcoholic beverages and smoking.
Tissue calcification is a pathological process associated with a high concentration of calcium in the body. Affects the cardiovascular, nervous, musculoskeletal, digestive and urinary systems. To prevent illness, you need to eat right and lead a healthy lifestyle. As therapy, a course of medications is prescribed to eliminate the cause of the pathological process and normalize the level of calcium and magnesium in the blood.