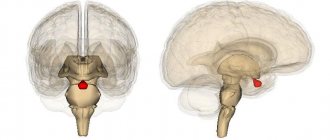
General information
Gliosis of the brain is a pathological process manifested by the replacement of neurons with glial elements.
Gliosis is not an independent disease; rather, it is a protective reaction to the death of neurons, that is, a secondary process. At the same time, the process of destruction of neurons stimulates the filling of the resulting voids with glial cells, which leads to a change in the quantitative ratio of elements of the nervous tissue. Brain tissue consists of a collection of neurons, ependymal membrane and glial cells. Normally, glial tissue is responsible for trophic/secretory functions and metabolism in brain cells, and also performs the function of protecting neurons. It accounts for about 40% of the total brain mass. The proliferation of glial cells forms foci of gliosis in the white matter of the brain, which, depending on the etiology of the primary disease, can be focal/diffuse in nature. Foci of gliosis can be located in any area (structures) of the brain. And the more glia are formed, the less efficiently the central nervous system functions. With a large proliferation of glia, a cystic-gliotic atrophied area of brain tissue can form. The more glia are formed in the white matter, the worse the functioning of the entire nervous system. A cystic-glial-atrophic area is formed.
There are no statistical data on the incidence of various types of gliosis. It can only be noted that supratentorial foci of gliosis are most common.
Supratentorial lesions - what are they? Supratentorial are foci of gliosis of vascular origin. Various pathological processes in the vessels of the brain ( thrombosis , fibrosis , necrosis ) that cause circulatory disorders contribute to the formation of small hyper/hypertensive areas, which are accompanied by such disorders as poor coordination, dizziness , and changes in handwriting.
Single foci of gliosis
Focal gliosis is characterized by single, clearly defined islands in the white matter, the size and location of which is determined by the causes of neuronal death. They occur in people of any age and, perhaps, as a manifestation of natural age-related degenerative processes in brain tissue, ischemia of cerebral structures, local inflammatory process, chronic hypertension demyelination process , and as a consequence of injuries during childbirth in infants. Typically, single (limited foci) of gliosis of the brain are an accidental finding on CT/MRI, since in most cases they are not clinically manifested and do not cause discomfort, with the exception of their localization in the frontal lobe, where the centers associated with feelings and sensations are located, which can manifested by the appearance of hallucinations. A single gliosis of the brain is not prone to proliferation.
Multiple foci of gliosis
The appearance of multiple foci of gliosis is caused by injuries and acute/chronic circulatory disorders of the brain, that is, of vascular origin. As the pathology/disease that causes neuronal death develops, both the number and size of the altered areas increase. They occur predominantly against the background of severe atherosclerosis , stroke , cerebral infarction , with compression of cerebral vessels and as a result of age-related changes. Multiple foci of gliosis for the most part enhance the clinical symptoms of the underlying disease and cause dysfunction of the central nervous system.
Definition of pathology
When the neurons that make up the nervous tissue are damaged, glial cells form in their place. Gliotic changes are a process occurring in the brain, which is characterized by an increase in the number of glial cells, which, when the scale of replacement expands, leads to a deterioration in the functioning of the central nervous system. The more glial foci in the medulla, the worse the brain performs its functions.
Disorders are most often associated with a deterioration in the transmission of nerve impulses, with the help of which the nervous system controls the organs and systems of the body. Proliferation of glial cells most often occurs in the form of diffuse distribution of astrocytes. As areas consisting of glial cells grow, signs of pathology appear, such as impaired motor coordination, memory impairment, slowness of movements and reactions. Gliotic transformation of the brain, depending on the type of primary pathology, occurs with characteristic features.
In diabetes mellitus, large-scale infiltration of macrophages and hypertrophy (pathological increase in size) of astrocytes is observed. Gliotic changes in drug addicts are accompanied by an increase in the number of oligodendrocytes of drainage forms. In multiple sclerosis, hypertrophy of astrocytes and changes in the glial formula are detected (astrocytes - 46%, oligodendrocytes - 40%, other cells - 14%).
Normally, the glial formula looks like this: astrocytes - 8.5%, oligodendrocytes - 85%, other cells - 7.5%. In epilepsy, there is a decrease in the number of oligodendrocytes by 20% and microgliocytes by 6%. Glial cells are the most numerous and active components of brain tissue. They retain the ability to divide throughout their lives. Due to their high activity, glia cells immediately respond to any changes in the functioning conditions of the brain.
The average number of cells in 1 mm2 of brain tissue varies depending on the location of the site. For example, in the parietal lobe the number of cells is 2 times greater than in the frontal region. When diagnosed with multiple sclerosis, the number of glial cells in areas not affected by the demyelination process may increase by about 3 times. In patients with drug addiction, the proportion of glial cells increases approximately 2 times.
With dyscirculatory encephalopathy, this indicator increases slightly. Foci of gliosis arise as a reaction of neuroglia to damage to nervous tissue or changes in the functioning conditions of the brain. The mitotic activity of gliocytes increases in response to the development of pathological processes in the tissues of the central nervous system. Gliotic foci are a consequence of the process of restoration of destroyed brain tissue. However, the functions of areas of restored tissue are not always adequate to normal physiological processes.
The reason for the incomplete correspondence of functions lies in the underdevelopment of glial cells, which, having not reached maturity and a normal level of functioning, undergo apoptosis (a regulated process of cell death). Similar phenomena are most clearly observed in multiple sclerosis. What is dangerous for humans is not the process of glial transformations itself, but rather its scale and incompleteness associated with the interruption of the normal development of gliocytes.
Classification
The classification is based on the nature of the proliferation of glial cells and their localization.
Based on morphological characteristics, the following are distinguished:
- The isomorphic form is characterized by an ordered proliferation of neuroglia.
- Anisomorphic form - has a pronounced cellular structure and is characterized by chaotic growth; most often localized subcortically/paraventricularly. Periventricular gliosis - formed in the ventricles of the brain. Often periventricular gliosis is accompanied by the development of cysts. Fibrous form—the predominance of the fibrous type structure is noted.
According to the localization of the pathological process, the following are distinguished:
- Periventricular gliosis - glial cells are formed in the ventricles of the brain. Periventricular gliosis is often accompanied by the development of cysts.
- Perivascular (vascular) gliosis is the growth of glia along atherosclerotic vessels. It is often diagnosed on MRI as microangiopathy with the presence of foci of gliosis.
- Subependymal gliosis is predominantly localized on the inner lining of the ventricles of the brain.
- Marginal gliosis - located on the surface of the brain.
- Marginal gliosis - foci of degeneration are localized in the intrathecal region.
Based on quantitative criteria, single and multiple foci of gliosis are distinguished. Histologically, hypodense (without a definite structure, cannot be stained) and hyperintense (clearly structured, well stained) areas of gliosis are distinguished.
Based on the nature of the process/prevalence, the following are distinguished:
- A focal type of flow, involving a limited area of the brain (usually in the temporal/parietal regions).
- Diffuse type of course - characterized by multiple lesions of various sizes/localizations. Most often of vascular origin and may have the appearance of a cystic-gliotic formation.
Diagnosis of cerebral gliosis
In most cases, the disease is verified by chance during an MRI or CT scan of the brain. The form is not dangerous. A repeat examination after a few months is carried out in order to study old glial areas. The absence of an increase in size indicates a favorable prognosis.
MR and CT angiography with a contrast agent helps to identify the vascular genesis of the nosology. Electroencephalography (EEG) determines or excludes changes in cerebral activity. The procedure is prescribed for the occurrence of epileptic seizures and muscle cramps.
Practice shows a predominant transformation of neuroglia during aging in the frontal lobes.
Causes
The pathological process of replacing neurons with neuroglial cells may be based on a variety of reasons:
- Age-related changes caused by the natural process of neuron death.
- Diseases of hereditary origin - lysosomal storage disease ( Tay-Sachs disease ), inherited in an autosomal recessive manner, characterized by massive death of neurons in children, which is the cause of their death); genetically determined pathology - tuberous sclerosis .
- Birth injuries at birth.
- Traumatic brain injuries.
- Multiple sclerosis (destruction of myelin and the formation of foci of demyelination in various brain structures).
- Cerebral infarction (ischemic stroke).
- Hemorrhagic stroke is a hemorrhage into the structures of the brain, which forms foci of gliosis of vascular origin.
- Brain swelling.
- Epilepsy.
- Arterial hypertension/encephalopathy caused by a persistent increase in blood pressure.
- Neuroinfections ( encephalitis , meningitis ). oxygen starvation of brain tissue ( hypoxia ).
- Hypoglycemia (low blood sugar).
- Surgical interventions on brain structures.
- Atherosclerosis of cerebral arteries.
- Abuse of products containing animal fat.
Causes of gliotic changes
Hereditary predisposition is considered one of the main (25% of cases) causes of the development of gliosis. The occurrence of gliosis changes is associated with the following diseases affecting brain tissue:
- Multiple and tuberculous sclerosis.
- Encephalitis and encephalopathies of various etiologies.
- Oxygen starvation (hypoxia).
- Status epilepticus.
- Arterial hypertension occurring in a chronic form.
- Diabetes mellitus and other metabolic disorders.
- Drug use.
- Neuroinfections occurring in acute and chronic forms.
- Cerebrovascular pathologies.
- Neurodegenerative processes.
- Chronic renal failure.
- Phakomatoses (hereditary, chronic diseases characterized by damage to the central nervous system, skin, visual organs and other body systems).
Some doctors make an analogy. If a person's skin is damaged, scars form on them. Such “scars” appear in nervous tissue after damage and partial death of neurons. The process does not occur spontaneously; it is always a consequence of primary pathology. The most common reason is deterioration of blood flow in the circulatory system supplying the brain, associated with damage to the vascular wall, narrowing of the lumen, or disruption of neurohumoral regulation.
Gliotic changes in the intracranial structures of the head in adults are detected after cerebral infarctions, strokes, and after the appearance of foci of intracerebral hemorrhage. Similar transformations of nervous tissue are detected after neurosurgical intervention and poisoning with harmful substances (carbon monoxide, salts of heavy metals, narcotic substances). Gliotic foci form around tumor neoplasms.
Symptoms
Clinical symptoms vary widely and are determined mainly by the symptoms of the underlying disease that caused gliosis. As a rule, single small foci of gliosis do not produce specific neurosymptoms and are discovered by chance during an MRI examination of the brain. At the same time, multiple (extensive) foci of gliosis almost always manifest neurosymptoms in the form of:
- Unreasonable long-term intense headaches that are not controlled by taking antispasmodics.
- Blood pressure instability (sudden changes in a short period of time).
- Periodically occurring dizziness .
- Decreased performance/increased fatigue.
- Changes in visual/auditory perception.
- Disorders of coordination, attention and memory.
- Motor disorders (with large lesions, up to convulsive conditions).
Clinical symptoms are largely determined by the localization of the focus of gliosis:
- Localization of foci of gliosis in the temporal lobes is characterized by frequent, intense, long-term headaches. With the vascular genesis of the process, the pain syndrome is combined with sudden changes in blood pressure.
- Supratentorial gliosis manifests itself mainly with visual disturbances – hallucinations; distortion of the outlines, sizes, shapes of objects; loss of visual fields, difficulty recognizing an object by appearance.
- Gliotic foci in the white matter of the brain can cause dizziness , an episyndrome characterized by increased convulsive activity with the possible development of epileptic seizures. Such symptoms develop as a complication of traumatic brain injury/surgery.
The localization of gliosis foci in the frontal lobes is often due to age-related changes. It is generally accepted that if diseases that can cause the death of neurons and the proliferation of glial cells have not been identified, then such a process should be considered a primary pathology that develops as the body ages and manifests itself as impaired concentration, attention, memory, fine motor disorders, and slowed reactions.
Signs of neuroglial accumulation in the brain
Pathological manifestations of the accumulation of neuroglia inside the brain are only in rare cases provoked by serious diseases. In older people, foci of gliosis gradually increase, which leads to the progression of neurological symptoms:
- Impaired coordination of movements;
- Memory loss;
- Prolonged pain syndrome of the head;
- Frequent changes in blood pressure;
- Muscle cramps;
- Epileptic seizures;
- Dizziness.
Using MRI and CT, it is possible to calculate the number of neuroglial proliferations per unit volume of cerebral tissue. The value is used to assess the progression of the disease and evaluate the effectiveness of treatment.
Interesting fact
A study by epidemiologists has proven the influence of neuroglia on the aging process. Experts added blood taken from an elderly person to the morphological material of glia. The consequences of the experiment turned out to be impressive - neuroglial layers began to actively multiply, destroying neurons. The results suggest mechanisms for the development of senile dementia.
A similar process does not occur in children. The proliferation of neuroglia in the white matter is observed only after the death of neurons. The mechanism is local in nature. The lesions cover the formed defects.
Tests and diagnostics
Diagnostics is based on imaging methods (MRI/CT) of the brain. These methods allow you to determine:
- location and size of pathological foci;
- the presence of marginal (perifocal) infiltration;
- structure (homogeneity) of the white matter of the brain;
- perivascular spaces of various areas;
- areas of the basal ganglia;
- the presence of other pathological formations;
- condition of the ventricles of the brain/pituitary gland, functionality/condition of the blood vessels of the brain.
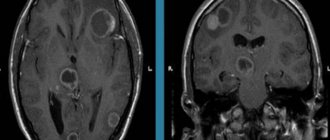
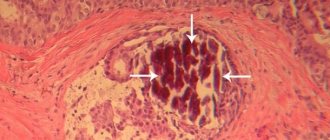
The image below shows multiple foci of gliosis.
MRI makes it possible to establish not only the presence of areas of gliotic changes, but also to identify the cause. MRI images provide a clear picture of the presence of areas in the brain that do not receive sufficient nutrition due to vascular obstruction by atherosclerotic plaques; allow you to identify inflammatory processes, areas of hematoma, and identify neoplasms. This, to a certain extent, makes it possible to eliminate the provoking factor and develop tactics to minimize the risks of further spread of the process.
Diagnostics
CT and MRI studies allow us to get an idea of the location of foci of gliosis of vascular or other origin in the brain. Based on the results of neuroimaging, the scale and nature of the process of neuronal replacement are judged. The study helps to establish the primary disease that provoked the change in tissue structure.
The clinical picture presented by a tomogram after an MR study and reflecting the presence of single supratentorial foci of gliosis is often associated with a diagnosis of multiple sclerosis or a brain tumor. Neuroimaging in most cases makes it possible to determine the nature of glial changes - post-traumatic, vascular, postoperative, inflammatory, associated with demyelinating processes in brain tissue.
During an MRI study of the brain, foci of gliosis are identified as areas with a hyperintense signal in T2 and Flair mode; they are brightly highlighted on the tomogram. Often the identified areas do not correspond to the morphological structure of glial tissue, which indicates the need for additional diagnostic studies. A consultation with a therapist, neurologist, ophthalmologist, and neurosurgeon is indicated.
Diet
There is no special diet, but it is recommended to adhere to the diet recommended for the underlying disease that initiates the process of formation of glial lesions ( Diet for stroke , Diet for hypertension , atherosclerosis , diabetes mellitus , Diet for obesity , etc.). In general, it is recommended to adhere to a low-calorie diet with sufficient vitamin content (vegetables, fruits) and a minimum content of animal fats in the diet.
Traditional treatment
- To inhibit the processes of sclerosis of blood vessels and neurons:
400 gr. mix crushed leaves of 5-year-old aloe with 650 mg of honey and 650 g. red Cahors. Let it brew in a dark place for at least 5 days. Take 1 teaspoon 3 times before meals. The course of treatment is 2-4 weeks.
- To dilate blood vessels in the brain:
2 tbsp. Mix dill seeds and a glass of crushed valerian root with 1.5-2 glasses of honey, pour 1 liter of boiling water. Let it brew for a day. Before meals, take a tablespoon of the mixture for 4-6 weeks .
150-250 gr. Pour boiling water over hawthorn fruits. Let it brew for 30 minutes. Take the infusion 1 tbsp. half an hour before meals. The course of treatment is up to 1.5 months .
Prevention
No drugs or methods of specific prevention of neuronal death have been developed. To maintain the activity of neuro-processes and brain vessels, we can only recommend:
- Lead a healthy lifestyle.
- Monitor your body weight.
- Maintain age-appropriate physical activity.
- Constantly monitor blood pressure, cholesterol , and blood sugar levels.
- Minimize bad habits.
- Practice a healthy balanced diet by minimizing foods containing animal fats.
- Train brain functions: solve puzzles/crosswords, learn poetry, foreign languages.
Diagnosis, treatment
Diagnosing education is not difficult. It is enough to perform a CT or MRI examination. The latter is more preferable, since in addition to better visualization there is no radiation exposure.
Additional diagnostic methods are angiography and electroencephalography (EEG).
The only effective treatment for cystic gliosis transformations is surgery. It should be understood that dead neurons cannot be restored and the operation is aimed at eliminating epilepsy or hydrocephalus that has developed against the background of atrophy.
Many neurosurgical centers have learned to perform this operation in a low-traumatic manner using endoscopic techniques. The essence of the operation is to puncture the resulting cavity and remove the internal fluid. This eliminates excessive compression of the brain.
Forecast
The prognosis of life with cerebral gliosis is largely determined by the underlying disease and can vary significantly depending on the volume of gliosis foci and the intensity of neuronal replacement. As a rule, the prognosis for life with single foci outside important brain structures is relatively favorable, while extensive foci of gliosis in areas of the brain responsible for important functions of the central nervous system can be unfavorable, for example, in the temporal lobe, initiating frequent epileptic seizures.
Morphology of brain gliosis
The destruction of functional brain tissue leads to the replacement of damaged areas with neuroglia. The process is necessary to ensure cerebral nutrition and provide necessary substances.
MRI of brain gliosis
The main anatomical structures of the central nervous system:
- The cell layers of the lining of the ventricles are ependymal;
- Functional elements of nerve signal transmission are neurons;
- Tissues that provide framework, construction, metabolic, secretory functions are neuroglia.
Most of the cerebral structure consists of glial elements. The complex provides many functions, but signal transmission is achieved through interconnections between neurons. The fewer nerve fibers, the slower the processes proceed. Trophic functions are performed by glia, which fills about forty percent of the brain.
Inflammation, infections, and traumatic brain injuries can lead to the destruction of neurons and ependyma. The sites of destruction are filled with neuroglia, creating scars that are similar to scars on the skin (overgrowth of connective tissue fibers).
List of sources
- Vereshchagin N.V., Gulevskaya T.S. Pathology of the brain in atherosclerosis and arterial hypertension. – M.: Medicine, 1997. – 228 p.
- Vasiliev V.N., Kindyashova V.V., Kozhevnikova V.V., Tikhomirova O.V., Lomova I.P., Serebryakova S.V. Clinical and diagnostic significance of microfocal brain lesions of vascular origin among management specialists // Medical, biological and socio-psychological problems of safety in emergency situations. 2014. No. 3. pp. 27-32.
- Gladky P. A., Sergeeva I. G., Tulupov A. A. Infectious lesions of the brain. Tutorial. Novosibirsk 2015. – 24 p.
- Putilina M.V. Chronic cerebral ischemia//Attending physician. 2005. No. 5.
- Yanishevsky S.N. Brain damage in patients with type 2 diabetes // International Journal of Endocrinology. No. 8(64). 2014 pp. 89-97.
What is the danger?
The consequences of cystic glial changes can be fatal if symptomatic epilepsy or malignant hydrocephalus occurs.
In the first case, constantly occurring irritation of the area adjacent to the cystic-gliotic transformation leads to its depletion and neuronal atrophy. Epilepsy is fraught with everyday discomfort, limitation of social activity, mental and mental disorders.
Acutely developed dropsy of the brain can cause death. When the liquor pathways are completely blocked, the latter begins to “put pressure” on the substance of the brain. Intracranial pressure increases. The brain tends to the area with less pressure and ends up being pinched into the hole in the occipital bone. Death occurs instantly.
Cystic-glial changes are a serious consequence of brain injuries in the absence of proper control and treatment.
Signs of gliosis
Quite often, the patient learns about the presence of a single focus of gliosis in his brain, by chance, during a routine examination. At the same time, nothing bothers the person. This situation requires special attention.
The patient must be carefully examined and the reason why the lesion formed is identified, that is, the disease that provoked the proliferation of glial fibers. In the case of multiple foci of glia, the situation is different; unpleasant symptoms cannot be avoided.
Symptoms:
- Constant headaches.
- Blood pressure surges
- Dizziness.
- Violation of intellectual activity.
- Loss or impairment of coordination.
- Changes in speech functions.
- Paresis and paralysis.
- impairment .
- Changes in the mental sphere.
- Dementia.
The larger the area of brain damage, the more pronounced the symptoms of this disease.
Foci of gliosis
Foci of gliosis can vary in number and area. This proliferation of glial tissue occurs against the background of the destruction of its own neurons, it follows that the greater the number of these nerve cells is destroyed, the larger the focus of gliosis will be.
Diseases that provoke gliosis:
- Epilepsy.
- Hypertension lasting for a long period.
- Multiple sclerosis.
- Hypoglycemia.
- Ischemic stroke.
- Low oxygen content in the blood.
- Poor blood circulation.
- Encephalitis.
- Anemia.
- Injuries and swelling of the brain.
Gliosis can also occur for other reasons not related to specific diseases.
Causes:
- Hereditary factor.
- Injuries during childbirth.
- Elderly age.
- Excessive consumption of fatty foods.
The prognosis of treatment and the patient’s life depends entirely on the extent of the gliosis process; the more advanced the process, the more complex the therapy and the longer the patient’s recovery.
Single
Single foci of gliosis can occur in many. This usually means that the patient has hypertension. With constantly elevated blood pressure, after some time, as a rule, hypertensive encephalopathy occurs, which leads to isolated foci of gliosis.
It is important to contact a medical facility to stop the process of neuronal death, otherwise the affected area and the number of lesions may increase significantly. The problem is that it is no longer possible to reverse this process, the nerve cells die irrevocably, and, most importantly, prevent their further destruction.
Gliosis often causes diseases of the nervous system , which cannot be completely cured, but modern medicine can stop the progression of such diseases, and therefore the development of gliosis itself.
Multiple
Multiple foci of cerebral gliosis are usually found in the diffuse type of this disease. A disease of this form is characterized by large foci of glial growths, which makes the functioning of the nervous system almost impossible.
If with single lesions, the symptoms of this disease are weakly expressed or may be completely absent, then with multiple lesions the symptoms are quite serious and severe .
It should be noted that gliosis of the brain can appear against the background of aging , when neurons in the brain die off. This situation is quite natural; with the help of medications, it is possible to partially restore the functions of the nervous system of an elderly person.
How to prevent brain gliosis
There is no specific prevention that can protect neurons from destruction and brain tissue from glial growths.
But doctors can give advice that will help support the blood vessels of the brain and preserve the activity of neurons for as long as possible.
Patients must adhere to the following rules:
- Lead a healthy lifestyle.
- Stay physically active. Avoid gaining excess weight.
- “Train” the brain: learn languages, poetry, solve crosswords.
- Monitor cholesterol and glucose levels.
- Monitor blood pressure, and if you have hypertension, take antihypertensive medications regularly.
For reference. It is important to eliminate risk factors that may cause neurological problems. Limit your intake of “junk” food, do not drink alcohol and do not smoke. Monitor the course of chronic diseases (hypertension, arrhythmia, diabetes mellitus).
Consequences and life prognosis
Gliosis of the brain cannot be called a minor pathology. This situation requires immediate medical attention. The prognosis for such patients will depend entirely on the extent of the gliosis process and the diseases that caused it. Often it is enough to undergo a course of therapy with a neurologist, and the disease will recede. Sometimes treatment can take years without improvement.
Unfortunately, newborn children suffer from this disease much more severely than adults. The death of nerve cells in infants progresses rapidly, leading to the death of the child. During routine examinations of pregnant women, ultrasound diagnostics can reveal glial changes in the fetal brain. In this case, the question of termination of pregnancy .