Disorders of the venous circulation of the brain
Classification. The following chronic and acute variants of venous circulation in the brain are distinguished. Chronic include venous congestion and venous encephalopathy, acute include venous hemorrhage, thrombosis of the veins and venous sinuses, thrombophlebitis.
Venous stagnation. The most common form of venous circulation disorder is due to various reasons: cardiac and cardiopulmonary failure, respiratory diseases (bronchitis, bronchiectasis, bronchial asthma, emphysema, etc.); compression of extracranial veins (internal jugular, innominate, superior vena cava), struma, arterial aneurysm, tumor in the neck; neoplasms of the brain, membranes and skull, arachnoiditis, traumatic brain injury, thrombosis of the veins and sinuses of the dura mater, compression of the veins with cerebral edema and craniostenosis. With venous stagnation, metabolic changes and brain hypoxia occur, venous and intracranial pressure increases, and cerebral edema develops. More often, milder disorders occur in the form of changes in the tone of the cerebral veins, which is detected using orbital plethysmography and rheography.
Clinical manifestations. A dull headache, more pronounced in the morning, increases with movements of the head to the sides, changes in atmospheric pressure, changes in ambient temperature, after excitement, drinking alcohol, etc., there is a hum or noise in the head, cyanotic lips, cheeks, ears, nose , mucous membranes of the oral cavity, swelling of the lower eyelids, especially in the morning, dilation of the veins in the fundus. Venous pressure ranges from 55 to 80 mmH2O, arterial pressure is usually within normal limits. Stupefaction, dizziness, darkening of the eyes, fainting, and numbness of the extremities are observed. Epileptic seizures and mental disorders are possible. With severe venous stagnation, patients are unable to lower their heads and remain in a horizontal position.
Measurements of pressure in the ulnar vein, radiography of the skull (increased development of diploic veins, graduates and veins of the dura mater), and phlebography are of diagnostic value in venous pathology.
Venous encephalopathy. With venous encephalopathy, the following syndromes are distinguished: hypertensive (pseudotumorous), diffuse small-focal brain damage, bettolepsy and asthenic.
Bettolepsy, or cough epilepsy, develops with chronic bronchitis and emphysema, pneumosclerosis, bronchial asthma, especially with cardiopulmonary failure. A persistent cough may result in sudden loss of consciousness (syncope).
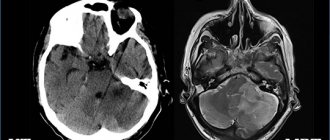
Venous hemorrhages. Capillary-venous hemorrhages in the brain and capillary-venous stasis are observed in hypertension. Venous stroke occurs in patients with heart failure, traumatic brain injury, brain tumor, infectious and toxic brain lesions. Clinical manifestations develop slowly: confusion, speech disorders, diplopia, pyramidal reflexes, hemiparesis, hemihypesthesia, damage to cranial nerves.
Thrombosis of cerebral veins. It occurs in the practice of clinicians of many specialties as a complication of various inflammatory processes, infectious diseases, operations, abortions, pregnancy, childbirth, skull trauma, “blue” heart defects, etc. Changes in the walls of the veins, a slowdown in the speed of blood flow and increased blood clotting play a role in the pathogenesis, as well as a change in the colloidal properties of endothelial cells, which contributes to the aggregation of blood cells. Often, thrombosis of the cerebral veins is combined with thrombosis of the sinuses of the brain, as well as the veins of the lower extremities.
Clinical manifestations. Cerebral vein thrombosis usually develops gradually. Headache, nausea, vomiting, meningeal symptoms, congestive optic discs, increased body temperature, and increased ESR appear. In the cerebrospinal fluid, mild pleocytosis and an increase in protein content, sometimes blood, are detected. Characterized by confusion, partial motor-type seizures, and less commonly generalized convulsions. Depending on the location of the venous lesion, focal symptoms occur: aphasia, alexia, hemianopsia, flaccid or spastic paresis or paralysis, and sensory disturbances. The outcome is often favorable, focal symptoms often undergo significant or even complete regression, but there are relapses of the disease. A slow chronic course over many months and even years is possible. Sometimes there are consequences in the form of mental disorders, aphasia, convulsive seizures and paresis of the limbs.
Thrombosis of the dural sinuses. Usually develops when infection penetrates into them from a nearby focus (furuncles or carbuncles of the scalp, face, erysipelas, etc., purulent osteomyelitis of the skull bones, purulent acute and chronic otitis media, mastoiditis, purulent processes in the orbit, paranasal sinuses) along the brain and diploic veins. In addition, phlebitis and thrombosis of the dural sinuses can occur hematogenously with thrombophlebitis of the veins of the extremities or pelvis and during septic processes. Thrombosis of the cerebral sinuses is sometimes accompanied by thrombophlebitis of the retinal veins, purulent meningitis, brain abscesses, etc. Sinus thrombosis can also occur with chronic infections (tuberculosis), malignant tumors and other diseases that occur with cachexia, in debilitated patients and in old age.
Clinical manifestations. Low-grade or sometimes very high, stable or fluctuating body temperature, headache, vomiting, leukocytosis in the blood, increased intracranial pressure. With thrombosis of the sinuses of the convexital surface of the brain, general cerebral symptoms predominate; in the sinuses of the base of the brain, signs of damage to the cranial nerves predominate. Drowsiness develops, sometimes, on the contrary, motor restlessness, insomnia, delirium, epileptic seizures, rigidity of the neck muscles, Kernig's symptom, hyperesthesia to visual, auditory and skin stimuli, and sometimes trismus. Focal symptoms of brain damage correspond to the location of the sinus. Swelling and cyanosis of the face or mastoid area are noted. In the fundus, dilated veins and swelling of the optic discs are detected. The cerebrospinal fluid is clear or xanthochromic, sometimes with an admixture of red blood cells; moderate pleocytosis is noted. Septic thrombosis of the dural sinuses is manifested by chills and very high remitting temperature. With thrombosis of the superior sagittal sinus, epileptic seizures of the motor type, hemi- and paraplegia or paresis occur.
Symptoms of thrombosis of the transverse or sigmoid sinus: headache, bradycardia, sometimes double vision, septic temperature, chills, stupor, turning into a soporous and even comatose state, sometimes delirium and agitation, anti-pain position of the head with an inclination to the painful side, meningeal phenomena, leukocytosis in blood. The jugular vein may be involved in the process. In this case, swelling of the tissue surrounding the vein and signs of damage to the glossopharyngeal, vagus, accessory and hypoglossal nerves occur.
Symptoms of cavernous sinus thrombosis: exophthalmos, swelling and venous hyperemia of the eyelids, orbits, forehead, root of the nose, dilation of the fundus veins (congestion), pain and hyperesthesia in the area of innervation of the superior branch of the trigeminal nerve, chemosis of the conjunctiva, ophthalmoplegia - paralysis or paresis of muscles, innervated by the III, IV, VI cranial nerves, stupor, delirium, sometimes coma, metabolic and endocrine dysfunction.
Complications: purulent meningitis, metastatic abscesses in the lungs, septic pneumonia.
Thrombophlebitis of the cerebral veins. With thrombophlebitis of the cerebral veins, the temperature rises to subfebrile levels with periodic rises to 38–39 °C. Patients complain of headache, nausea, and vomiting. Observed stupor, stuporous state, epileptic seizures, paresis of the limbs; in the fundus – swelling and dilation of veins; in the blood - leukocytosis; in the cerebrospinal fluid - slight pleocytosis, an increase in the amount of protein and positive protein reactions, sometimes an admixture of erythrocytes.
Diagnosis of venous discirculation in cervical osteochondrosis
Venous discirculation in cervical osteochondrosis requires careful differential diagnosis. Clinical symptoms present with obstructed venous outflow through the vertebral veins can occur with a number of other pathologies. In particular, it is necessary to exclude brain tumors, acute cerebrovascular accident, cerebral aneurysm, etc.
If the outflow through the vertebral veins is difficult, diagnosis begins with a visit to a vertebrologist. The specialist examines the patient and conducts a series of diagnostic functional tests. Then, as necessary, he can prescribe additional examinations:
- Doppler scanning of the blood vessels of the brain and neck;
- examination of the fundus vessels (performed by an ophthalmologist);
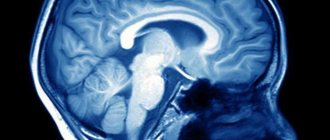
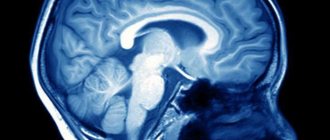
- MRI of brain structures and cervical spine;
- X-ray of the cervical spine in several projections;
- EEG of the brain, etc.
After an accurate diagnosis is made, treatment begins. It can be carried out using conservative methods and surgery (in advanced cases).
Prevention of vertebrobasilar insufficiency
To prevent the occurrence of vertebrobasilar insufficiency, people who have a predisposition to the disease must adhere to the following rules:
- eat right, limiting the consumption of salty foods;
- do gymnastics regularly - moderate physical activity has a positive effect on the condition of blood vessels and the blood circulation process;
- spend more time outdoors;
- try to avoid stressful situations and injuries;
- completely give up bad habits;
- position your torso comfortably during work and night rest;
- Visit your chiropractor regularly for preventive examinations.
Forecast
The prognosis is relatively favorable. Statistics show that in 65% of cases a complete cure occurs, in 29% of cases minor residual effects are observed. The mortality rate as a result of poor blood flow from the head is about 23%. The prognosis is unfavorable in cases where the pathology is aggravated by hemorrhagic infarctions, sepsis, epileptic seizures that are difficult to control, and pulmonary embolism. Therapy is perceived more difficult by patients in early childhood and old age. Dysgemia at the third stage threatens the health and life of the patient. At the first signs of pathology, it is better to undergo a diagnostic examination and, if necessary, a course of therapy prescribed by a doctor.
148
Thrombolysis
Dissolution of venous blood clots with special drugs - thrombolytics. These include streptokinase, urokinase and actilise. Only direct administration of a thrombolytic through a catheter into a thrombus with regular monitoring of the patency of the affected segment is effective. Thrombolysis options may include the use of a special Angiojet device. The thrombolytic solution is supplied through a special probe under high pressure, and then the blood clots are sucked out by a special suction. Another similar device used in our clinic is the Aspirex probe. This is a special spiral suction that gently removes thrombotic masses. The use of Aspirex in the inferior vena cava is limited due to its large diameter, so catheter thrombolysis is the most acceptable method. Thrombolysis is possible only in the first 10 days from the onset of the disease, while the blood clots have not yet healed.
Characteristic symptoms
Signs of venous discirculation begin to appear at stage 2.
| Pathology can be recognized by the following symptoms | When the headache gets worse |
| Headache (dull, bursting) | In the morning, especially if you haven't gotten enough sleep |
| Weakness, fatigue, difficulty getting up in the morning | When you take a horizontal position or tilt your head down |
| Swelling of the lower eyelid, bags under the eyes | When you turn your head many times |
| Noise, ringing in the ears | When performing complex movements that require good coordination |
| Dizziness, fainting | When you exercise |
| Periodic numbness of the limbs | When there is a sudden change in weather |
| Blue tint to the tip of the nose, lips, cheeks | When you're nervous |
Closer to the third stage, the following signs are added to the listed characteristics:
- Disorders of coordination, memory, speech, thinking, psyche.
- The patient's gait is disturbed and he cannot perform precise movements, for example, touching his nose with his eyes closed.
- He becomes forgetful, whiny, irritable.
- May begin to speak less clearly.
- Intellectual abilities decrease.
- The frequency of numbness in the extremities also increases. This can eventually lead to paralysis.
- Epileptic seizures may also develop.
Ultimately, all this leads to a condition similar to the consequences of a stroke. At a very late and advanced stage of venous discirculation, the patient becomes disabled. Also, the disease at the third stage can lead to a stroke, which will further aggravate the severity of the patient’s condition.
What contributes to the disease
CVI is caused by the characteristics of the circulatory system. To rise through blood vessels, blood must resist gravity. Its rise is caused by a diaphragm, the main function of which is to create a pressure difference. Help in overcoming gravitational forces is also provided by muscles, by contracting which the vein is compressed and, thus, blood is pushed through. Valves located on the walls prevent it from flowing back.
Failure in the activity of any component of this complex system impairs the outflow of blood, the vessels become overcrowded, and the pressure in them increases. Thus, venous insufficiency of the lower extremities develops.
The development of such a disease can be facilitated by:
- low mobility;
- genetic predisposition;
- obesity;
- increased intra-abdominal pressure, which can be caused by lifting heavy things, tight clothing, severe coughing and even constipation;
- overheating of the legs;
- pregnancy;
- taking hormonal contraceptives;
- heavy loads when playing sports;
- varicose veins, vascular injuries and other pathological changes in the functioning of the circulatory system of the lower extremities, previously suffered.
Treatment methods
- First of all, doctors will try to rid you of the underlying disease. For this, various drugs may be prescribed (ACE inhibitors for hypertension, glycosides for heart failure, etc.) or surgery may be performed (for example, to remove a tumor compressing a vein).
- To improve the outflow of venous blood, you will be prescribed a venotonic. Examples of drugs in this group: Venoplant, Detralex, Aescusan, Anavenol.
- To thin the blood and prevent thrombosis, one of the medications based on acetylsalicylic acid will be prescribed: Aspirin, Aspirin Cardio, ThromboASS, Cardiomagnyl.
- To strengthen the vascular walls, doctors prescribe a course of treatment with Pyridoxine to their patients.
- To relieve cognitive symptoms, such as poor memory, emotional instability, difficulties in thinking, nootropics are used: Glycine, Phenibut, Phenotropil.