We present to you our own method for improving the functioning of the vestibular apparatus. Below are exercises that, if performed regularly, will greatly reduce the feeling of dizziness and unsteadiness.
Vestibular gymnastics is a set of gymnastic exercises aimed at strengthening the vestibular apparatus. Regular exercises in this program at home can significantly reduce the feeling of dizziness and instability.
IP – LYING ON YOUR BACK
- Arms extended behind the head, stretching in four counts. Repeat 6-8 times.
- Arms are extended behind the head, without lifting your hands from the floor, raise your head and look at your outstretched socks. Repeat 4-6 times
- “Bicycle” - put your hands under your head, legs bent, 3 sets for a count of 10.
- Legs bent at the knees, straighten your legs up, spread them apart, then connect them and lower them down. Repeat 6-8 times.
- Diaphragmatic breathing: inhale - inflate the stomach, exhale - draw in the stomach, 6-8 times.
Vestibular neuronitis
Vestibular neuronitis (VN) is an acute, most often viral lesion of the vestibular ganglion, vestibular nuclei and other retrolabyrinthine structures.
Schematic representation of vestibular nerve damage in VN
The disease occurs equally often in males and females, most often at the age of about 40 years.
Etiology and pathogenesis
VN is associated with diseases of infectious-allergic and toxic-allergic origin (herpes simplex virus type 1, food poisoning, metabolic disorders, etc.), as well as with diseases of unknown nature. The viral etiology of VN is supported by the frequent development of the disease after a respiratory viral infection, the epidemic nature of the disease with a peak incidence occurring in late spring and early summer, as well as cases described in the literature of simultaneous illness of several family members. The role of the herpes virus is confirmed by cases of the development of VL in herpetic encephalitis. The duration of clinical manifestations averages from 1 week to 3 months, after which the disease disappears without a trace and never recurs.
Clinic
Against the background of sudden severe dizziness, horizontal rotatory spontaneous nystagmus is detected, directed towards the affected ear, changing its direction to the opposite after a few hours. Dizziness usually increases with head movements and decreases with fixed gaze. Oscillopsia is often observed - unclear visual perception of surrounding objects when performing passive or active head movements due to instability of the image on the retina. Coordination of movements and balance are sharply disturbed: the patient lies on his side, corresponding to the side in which spontaneous nystagmus is directed. The vast majority of patients experience nausea (94%) and vomiting (65%). The severity of the symptoms frightens patients and their relatives so much that almost all patients with VN are taken to the hospital by an ambulance team.
Hearing does not decrease; neurological examination does not reveal symptoms indicating damage to the brain stem or other parts of the brain. The attack can last for several hours and days, then its severity gradually decreases, and usually after 10-14 days spontaneous signs of vestibular dysfunction disappear.
Diagnostics
It is based on the typical clinical picture of the disease: acute and relatively long-term (from several hours to several days) dizziness, accompanied by instability, horizontal or horizontal-rotatory spontaneous nystagmus with oscillopsia, nausea and vomiting. The diagnosis can be confirmed using a caloric test that reveals vestibular hyporeflexia or areflexia on the affected side, a head impulse test
The technique of performing the test is as follows: the patient is asked to fix his gaze on the tip of the nose of the doctor sitting opposite him, after which the doctor puts his hands on the patient’s head and with a sharp, sudden movement rotates it to the right, and then after a pause to the left by 20°. Normally, the patient's eyes remain fixed to the object of observation (the tip of the doctor's nose). If the vestibular function is impaired, the patient’s eyes turn along with the head, and then the gaze returns to the object (in this case, the patient has pathology on the left) and the Fukudo walking test.
Indirect signs of VN can be detected using high-field magnetic resonance imaging of the brain with gadolinium.
Enhanced MR signal from the left vestibular nerve in a patient with LN (contrast-enhanced MRI, gadolinium)
Treatment
The main directions of therapy for patients with VL are to reduce dizziness, nausea and vomiting and accelerate vestibular compensation. Symptomatic treatment includes the use of vestibular suppressants: dimenhydrinate (Dramine), metoclopramide (Cerucal), benzodiazepine tranquilizers (Diazepam) or phenothiazines (thiethylperazine). For vomiting, use the parenteral route of drug administration. Vestibular suppressants are recommended to be used for no more than 3 days, as they slow down vestibular compensation. It has been established that in patients with VL, the use of methylprednisolone in the first three days of the disease (at an initial dose of 100 mg, followed by a dose reduction by 20 mg every three days) leads to a higher rate of restoration of vestibular function a year after the disease.
It is also recommended to conduct vestibular gymnastics, which includes exercises in which movements of the eyes, head and torso lead to sensory mismatch.
Exercises for vestibular rehabilitation (Cawthorne-Cooksey, 1940)
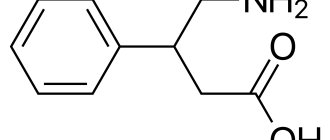
To accelerate vestibular compensation in combination with vestibular gymnastics, betahistine can be used up to 48 mg/day for 1 month or more. The use of neuromidin according to the regimen of 20 mg 3 times a day for two months is also pathogenetically justified.
← Back
IP – SITTING ON A CHAIR OR STOOL
- Arms are lowered along the body, tilt your head forward - slowly and touch your chin to your chest, and just as slowly come back. 6-8 times
- The arms are lowered along the body - we bend the arms at the elbows, move the elbows back - inhale, return to the starting position - exhale. 4-6 repetitions.
- Hands on knees, palms between legs. For 2 counts, tilt the head and torso to the left, return to the starting point, for 3-4 counts, tilt the head and torso to the right, return to the starting point. 4-6 repetitions.
- Rest – “coachman” pose: head tilted forward, hands resting loosely on knees, breathing calmly. 1-2 minutes.
Therapeutic positional maneuver for dizziness
Dizziness is the second most common reason after headache for which patients seek help from a doctor. Most often, these patients turn to a neurologist, general practitioner, or therapist. In the age group over 50, about 30% experience dizziness. It belongs to the group of subjective sensations, which is why it is so difficult to describe. Like any sensation, it is strictly individual and always has a bright emotional coloring.
Dizziness can be a symptom of many diseases, most of which relate to neurological and otoneurological pathologies.
In this article we will talk about such a condition as Benign Paroxysmal Positional Vertigo (BPPV).
The prevalence of this pathology: every 3rd person over 70 years old has had an attack of positional vertigo at least once. Women get sick 2 times more often than men. In 80% of cases, the posterior semicircular canal is affected and in 90% of cases an attack of positional vertigo occurs for no apparent reason. Other causes include: traumatic brain injury, Meniere's disease, labyrinthitis, vestibular neuronitis, middle ear surgery, ARVI, otitis media, intoxication.
Pathogenesis:
Clinical manifestations of benign paroxysmal positional vertigo are preceded by changes in the vestibular apparatus itself:
- Movement of otolith fragments from the vestibule into the semicircular canal
- Formation of canalolithiasis (otolith particles enter the lumen of the semicircular canal) or cupulolithiasis (otolith particles settle on the cupula) with irritation of the ampullary receptor
- Destruction of the otolithic membrane with the formation of a clot, its movement into the vestibule of the labyrinth.
Favorable conditions for the formation of a clot occur during sleep, when the head is motionless. When turning in bed, this clot enters the semicircular canal, which causes irritation of the receptors and, as a result, dizziness and autonomic reactions (nausea, vomiting, palpitations, a feeling of fear). Over time, clot particles dissolve in the endolymph. The dizziness subsides. However, relapses of dizziness are possible due to the fact that particles can stick to the walls of the canal and suddenly slide off, stick together when the head is stationary and again cause an attack of dizziness.
Clinic:
- BPPV is characterized by the sudden development of an attack of dizziness with a sensation of objects spinning around the patient. It intensifies when changing the position of the head (turning in bed, throwing the head back or tilting the head forward) and the body (from a lying position to a sitting position and vice versa).
- Time of occurrence of attacks: at night, when turning in bed or after sleep.
- The duration of the attack is up to 1 minute.
- Nystagmus is horizontal or horizontal-rotatory. It indicates irritation of the receptors of the posterior semicircular canal.
- Autonomic reactions: nausea, vomiting, anxiety, oscillopsia.
- Attacks may recur over several months, followed by remission for up to several years.
Diagnostics:
The main method for diagnosing BPPV is the Dix-Hallpike test.
Treatment:
In the treatment of this pathology, the main place is occupied by therapeutic positional maneuvers and vestibular gymnastics.
- Semont maneuver.
Performed with the help of a doctor. The initial position of the patient is sitting on the couch, legs hanging down. While sitting, the patient turns his head in a horizontal plane 45° to the healthy side. Fixing the head with his hands, the doctor places the patient on his side on the side of the affected ear and lingers there for about 90 seconds. Then the doctor, continuing to fix the patient’s head in the original position, quickly moves the patient to the opposite side through the “sitting” position - forehead down. The patient also remains in this position for 90 seconds. Next, without changing the position of the patient’s head, he is seated on the couch. If necessary, you can repeat the maneuver. - Epley maneuver (for pathology of the posterior semicircular canal).
The patient's starting position is sitting along the couch. First, the patient's head is turned towards the pathology and 45 degrees upward. Next, the patient is placed on his back, head tilted back 45°. The next turn of the fixed head is in the opposite direction in the same position on the couch. Then the patient is placed on his side, the position of the head also remains fixed. Next, the patient sits down, head tilted forward. The patient's stay in each position is determined individually, on average 90 seconds. As a rule, 2-3 maneuvers are performed during one session. - Lempert maneuver (for pathology of the horizontal semicircular canal).
The starting position, the same as when performing the Epley maneuver, is along the bed. The patient's head remains fixed by the doctor throughout the procedure. The patient's head is turned 45° in the horizontal plane towards the pathology. Then the patient is placed on his back, sequentially turning his head to the healthy side. After which the patient turns on his healthy side - with his healthy ear down. Next, in the same direction, the patient turns onto his stomach; The head is given a position with the nose down. Following this, the patient is placed on his side on the affected side; head - sore ear downwards. The last stage - the patient is seated on the couch through the healthy side. The maneuver can be repeated.
The starting position, the same as when performing the Epley maneuver, is along the bed. The patient's head remains fixed by the doctor throughout the procedure. The patient's head is turned 45° in the horizontal plane towards the pathology. Then the patient is placed on his back, sequentially turning his head to the healthy side. After which the patient turns on his healthy side - with his healthy ear down. Next, in the same direction, the patient turns onto his stomach; The head is given a position with the nose down. Following this, the patient is placed on his side on the affected side; head - sore ear downwards. The last stage - the patient is seated on the couch through the healthy side. The maneuver can be repeated.
After performing the positional maneuver, the patient is recommended to perform gymnastics using the Brandt-Daroff method at home for several days, after which he returns to see a doctor to assess his condition and correct therapy.
According to this technique, the patient is recommended to perform exercises three times a day, 5 times in both directions. Exercises are performed in bed, immediately after waking up. The patient sits in the center of the bed with his legs hanging down. Then he lies on either side, with his head turned upward by 45°, and remains in this position for 30 seconds (or until the dizziness stops). After which the patient returns to the original sitting position. The patient remains in the starting position for 30 seconds. Then everything is repeated, but in the opposite direction. If dizziness occurs at least once in any of the positions, then the gymnastics should be repeated during the day and evening.
Drug therapy for BPPV includes the use of the following groups of drugs:
- Antiemetics
- Antihistamines
- Vestibulolytic drugs
- Nootropic drugs
In conclusion, I would like to say that if dizziness occurs, it is necessary to consult a doctor for differential diagnosis of the disease, correct prescription of medications and therapeutic measures. All this is the key to your health!
IP – LYING ON YOUR Stomach
- Stretch your arms forward without lifting your chin from the floor, raise your legs, spread them, connect them, then lower them. Repeat 4-6 times.
- “Swimming” - raise your upper body and perform a movement with your arms as if swimming, without touching the floor with your hands. 4-6 repetitions of 4 movements on each hand.
- Hands in a “lock” behind your head, bend over 4-6 times.
- “Wings” - raise your arms and torso above the floor, spread your arms to the sides and swing them up and down 6 times
- Rest.
Exercises
First of all, at group exercise therapy, we did squats, among other things.
That is, it seems, what’s wrong with sitting down and standing up?
But, there are special conditions for this.
Firstly, getting up and sitting down is not so easy after a stroke.
Exercise 1:
Get up from the chair and sit down on it, first looking forward at any stationary object, and then all with your eyes closed.
Exercise 2:
From a sitting position on a chair, lean forward, take out an object located on the floor, then return to the starting position.
Next, you need to return this item to the floor.
Exercise 3:
While sitting, move your head up and down and left and right.
First, accompany the movements with your gaze, then fix your gaze on any stationary object at face level.
Exercises 4:
From the starting position lying on your back, turn to your left side, return to the supine position, then turn to your right side.
Copy from the Neurorehabilitation Center of Krasnoyarsk
Read also: REHABILITATION OF THE MUSTOCULAR SYSTEM DOCTOR ARACCHAA ERA MAADYEVNA
IP – SITTING ON A CHAIR OR STOOL
- Keep your head and shoulders straight. Slowly turn your head as far to the right as possible (5 times). Move to the left the same number of times.
- Lower your chin to your neck. Turn your head first 5 times to the right and then 5 times to the left.
- Throw your head back. Try to touch your right ear to your right shoulder (5 times). Perform the same movement, trying to touch your left shoulder with your left ear (5 times).
***The exercise therapy complex is designed for “dummies”, i.e.
a person who has never played sports, so it’s easy to do. First, within 2 months you must master the exercise therapy complex to the point of automatism, doing one approach of each exercise, then from the 3rd month the number of approaches can be increased to 2 for each exercise. Alternate exercises with rest, do not strain. Additional information can be obtained from our medical center.
What is vestibular gymnastics
Epley maneuver - vestibular gymnastics to improve coordination
Vestibular gymnastics for dizziness - a set of exercises, maneuvers to improve the functioning of the balance organ. If the pathology is not treated, the risk of complications increases.
Benefits of therapeutic exercise:
- a person learns to control the body, maintain balance, and the risk of falling during an attack decreases;
- it becomes easier to endure long trips, does not cause motion sickness;
- blood flow to the brain is normalized, tissues are saturated with oxygen;
- The quality of life improves after neurological diseases.
Correcting and improving the functioning of the vestibular apparatus helps to avoid the occurrence of dizziness, nausea and vomiting when external factors influence the balance organ. Gymnastics will help avoid falling and the development of other side effects of the pathology.
Indications and contraindications
Vestibular gymnastics can be beneficial during recovery after a stroke.
Vestibular gymnastics is prescribed by a doctor, taking into account the clinical picture and diagnosis. Exercises can be performed when the pathology is stable, without signs of progression. Exercises against dizziness are prescribed in combination with drug therapy.
Indications:
- post-stroke period;
- relief of BPPV symptoms;
- lack of coordination;
- cervical osteochondrosis, intervertebral hernia;
- ear pathologies;
- infectious diseases;
- rehabilitation after TBI, spinal injuries.
Contraindications: colds, fever, severe symptoms of vestibulopathy, cardiovascular pathologies.
Symptoms and course of the disease
VL is characterized by a monophasic course—an acute or subacute onset followed by subsidence of symptoms. The duration of clinical manifestations ranges on average from 1 week to 3 months (maximum manifestations range from several days to several weeks), after which the disease disappears without a trace. The probability of VN recurrence is 2-5%.
The disease begins with severe dizziness, accompanied by a certain type of nystagmus. Dizziness increases with head movements and decreases with fixed gaze. In 78% of cases, it appears suddenly; in 22% of patients, 1-2 days before the onset of the disease, phenomena in the form of instability and slight loss of coordination of movements are noted. Oscillopsia is often observed - unclear visual perception of surrounding objects when performing passive or active head movements due to instability of the image on the retina. Coordination of movements and balance are sharply impaired. Almost all patients experience nausea, and 65% have vomiting.
During the first day, the patient lies in bed - the slightest movements of the head provoke nausea and vomiting. On the 2-5th day, the patient is able to move within the room (ward), but the gait remains unsteady, and sudden head movements or walking long distances provoke nausea. On the 10-14th day, the patient complains of “heaviness” in the head and fatigue, but overall he feels healthy and can return to his usual lifestyle.
In the first days of the development of the disease, the brain “understands” that the vestibular apparatus is transmitting an incorrect sensory signal: the healthy labyrinth is always in an active state, the other (affected) labyrinth is depressed, which is interpreted by the brain as a constant rotation in the healthy direction. Since it is impossible to restore conduction along the affected vestibular nerve in a short time, the brain blocks the activity of the healthy labyrinth, aligning the flow of sensory signals from both vestibular apparatuses. As the vestibular nerve recovers, the control system returns to its original, healthy state.