What is increased intracranial pressure?
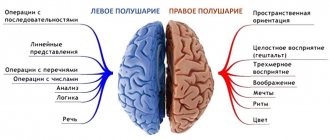
Inside the brain there is a system of interconnected ventricles, which are also filled with cerebrospinal fluid (CSF). This protects the human brain from injuries, concussions, as much as possible. The pressure of cerebrospinal fluid on brain structures is called intracranial pressure. Exceeding the permissible norms entails a number of consequences.
The main question for parents is what are the signs of intracranial pressure in a child, and what threat does this pose to the child?
What complications can there be in children? If left untreated, increased intracranial pressure can lead to the following consequences: the occurrence of epileptic syndrome, blurred vision, mental disorders, strokes, disorders of consciousness, breathing problems, weakness in the limbs, etc.
What should parents of a child with this diagnosis know? ICP is not a disease, but only a symptom, a consequence of various diseases. There are several misconceptions among parents regarding increased intracranial pressure. For example, the fact that this is an incurable condition. However, with timely treatment, the child’s recovery is possible. The main thing that needs to be done is to consult a specialist in time and follow the doctor’s instructions.
Detailed instructions from Dr. Komarovsky on fighting viruses
Cold season is coming, but you don’t want to get sick at all. The famous doctor Evgeny Komarovsky wrote an excellent article about how to avoid viruses, and about the rules of treatment if you have already become infected.
Remember the most important thing: the tactics of your actions are completely independent of the name of the virus. It's seasonal flu, swine flu, elephant flu, pandemic flu, it's not flu at all - it doesn't matter. The only important thing is that it is a virus, that it is transmitted by airborne droplets and that it affects the respiratory system.
Prevention
If you have the opportunity to get vaccinated, get vaccinated, but on the condition that you don’t have to sit in a snotty crowd at a clinic to get vaccinated. Available vaccines protect against all variants of the influenza virus that are relevant this year.
There are no drugs or folk remedies with proven preventive effectiveness. That is, no onion, no garlic, no vodka and no pills can protect against any respiratory virus in general, or the influenza virus in particular. All these “medicines” satisfy the main mental need - “something needs to be done.” The main benefit of all these “medicines” is psychotherapy.
The source of the virus is man and only man. The fewer people there are, the less chance you have of getting sick. Walking to the stop and not going to the supermarket one more time is a wise decision!
A mask is a useful thing, but not a panacea. It is advisable to see it on a sick person if there are healthy people nearby: it will not stop the virus, but it will stop droplets of saliva that are especially rich in the virus. A healthy person doesn't need it.
The patient’s hands are a source of the virus no less significant than the mouth and nose. The patient touches his face, the virus gets on his hands, the patient grabs everything around him, you touch everything with your hand - hello, ARVI. Don't touch your face. Wash your hands frequently and carry wet disinfectant wipes with you.
Monitor your air quality. Viral particles remain active for hours in dry, warm, still air, but are destroyed almost instantly in cool, humid, and moving air. Optimal indoor air parameters: temperature – about 20°C, humidity – 50-70%. Frequent and intensive cross-ventilation of the premises is mandatory. But you can walk as much as you like. It is almost impossible to catch a virus while walking.
Mucus constantly forms in the upper respiratory tract. Mucus ensures the functioning of local immunity - protection of mucous membranes. If the mucus and mucous membranes dry out, the work of local immunity is disrupted, viruses, accordingly, easily overcome the protective barrier, and the person becomes ill with a much higher degree of probability. Moisturize mucous membranes. You can buy a ready-made saline solution at the pharmacy or prepare it yourself (1 teaspoon of regular table salt per 1 liter of boiled water).
Treatment rules
Dress warmly, but the room should be cool and damp. Wash the floors more often, humidify the air, and ventilate the room.
Categorically do not force a sick person to eat. If he asks, give him something light, carbohydrate, liquid.
Drink as often as possible. The temperature of the liquid is equal to body temperature. In addition to water, compotes, fruit drinks, tea, raisin decoctions, and dried apricots are suitable. Ideal for drinking are ready-made solutions for rehydration (rehydron, humana electrolyte, gastrolit, normohydron, etc.).
Irrigate your nose with saline solutions more often.
To combat a high temperature, take only paracetamol or ibuprofen. Aspirin is strictly forbidden. If the upper respiratory tract (nose, throat, larynx) is affected, no expectorants are needed: they will only worsen the cough. Damage to the lower respiratory tract (bronchitis, pneumonia) no longer has anything to do with self-medication.
Viral infections are not treated with antibiotics. Antibiotics do not reduce, but increase the risk of complications. All antiviral drugs for topical use and for swallowing are drugs with unproven effectiveness. Homeopathy is safe, like psychotherapy, when “something needs to be done.”
When do you need a doctor?
Always. But this is unrealistic. Therefore, we list situations when a doctor is definitely needed:
- no improvement on the fourth day of illness;
- elevated body temperature on the seventh day of illness;
- worsening after improvement;
- severe severity of the condition with moderate symptoms of ARVI;
- the appearance alone or in combination of pale skin, thirst, shortness of breath, intense pain, purulent discharge;
- increased cough, decreased productivity, a deep breath leads to a coughing attack;
- when body temperature rises, paracetamol and ibuprofen do not help, practically do not help, or help very briefly.
A doctor is definitely and urgently needed when:
- loss of consciousness;
- convulsions;
- signs of respiratory failure (difficulty breathing, shortness of breath, feeling of lack of air);
- intense pain anywhere;
- even a moderate sore throat in the absence of a runny nose (sore throat + dry nose is often a symptom of a sore throat, which requires a doctor and an antibiotic);
- even moderate headache combined with vomiting;
- swelling of the neck;
- a rash that does not go away when you press on it;
- body temperature above 39°C, which does not begin to decrease 30 minutes after the use of antipyretics;
- any increase in body temperature combined with chills and pale skin.
Symptoms of increased intracranial pressure
Increased intracranial pressure in children, symptoms of which can appear in the first minutes and hours after birth, often leads to the development of serious complications.
When parents may suspect something is wrong:
In young children:
- The baby constantly cries and does not calm down;
- Lack of thirst in the child, reluctance to drink;
- The baby is irritated by bright lights and sharp sounds;
- The child burps frequently and profusely;
- The baby's fontanel bulges;
- The baby's chin is shaking;
- Rapid head growth (this is due to stagnation of venous blood);
- The child throws his head back.
In older children
- Severe headaches;
- Nausea, vomiting;
- Increased fatigue, weakness;
- Drowsiness;
- Tearfulness, irritability;
- Apathy;
- Double vision.
Knowing the key signs of the disease, you can establish the correct diagnosis in the early stages and prescribe the correct treatment for your child. Even if you have only one of the listed symptoms, you need to immediately contact a neurologist! The sooner your baby receives help, the fewer consequences it will have for the child’s body in the future.
Severe symptoms
Perhaps the main sign indicating this illness is the child’s restless behavior. The baby cannot sleep, cries all the time and does not even want to eat. He even vomits water.
In children, already at a few months old, external symptoms of increased intraocular pressure can be noticed and identified.
They are manifested by changes in the parameters of the child’s body:
- the head is disproportionately large;
- the frontal area is enlarged;
- the fontanel has signs of swelling;
- veins on the head;
- eyeballs are lowered too far;
- the child has problems gaining weight and slow reaction times;
- there are some developmental deviations;
- Sometimes frequent regurgitation also indicates an increase in IAP.
As your child grows, the symptoms become clearer and more pronounced. Having learned to speak, the child will be able to say that he is in pain, and it will be easier for parents to understand his condition.
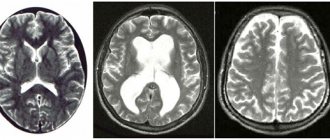
Diagnosis of intracranial pressure
Before prescribing treatment for your child, we perform a comprehensive neurological examination. It includes:
- Collecting anamnesis (conversation with the mother, studying the child’s medical record, history of pregnancy and childbirth and the results of previous studies);
- special neurological tests;
- active and muscle tests;
- reflex diagnostics;
- local palpation examination of the spine and musculoskeletal system.
In addition to the main examination, if necessary, the doctor may prescribe:
- NSG (neurosonography, ultrasound of the brain);
- MRI;
- Ultrasound;
- X-ray;
- Lab tests;
- EEG;
Treatment of ICP in infants
Treatment of intracranial pressure in infants can be aimed both at eliminating excess or replenishing the lack of cerebrospinal fluid in the cranium, and at eliminating the causes that provoke this problem.
The choice of one direction or another will depend on the cause of ICP in the child.
For example, if the problem is caused by a malignant tumor or anatomical disorders, then there is a reason to correct not the consequence, but the cause of the metabolic disorder (often, surgically).
But if, for example, the baby is suffering as a result of hypoxia, then it is enough to take measures that will ease the discomfort and promote normal circulation of the cerebrospinal fluid.
More details about treatment methods:
- surgical intervention: used in the most severe cases, when there is certain interference in the skull for the normal flow of cerebrospinal fluid;
- drugs that lower ICP (diuretics are usually prescribed: asparkam, diacarb, triamur);
- vitamins that help improve cerebral circulation;
- sedatives;
- massage;
- physiotherapy (a swimming pool is often prescribed);
- homeopathy;
- Doctors also strongly recommend frequent emotional contact with the baby, regular walks in the fresh air, breastfeeding, and maintaining a sleep schedule.
Advice: do not be afraid of drug treatment. The sooner you start it, the faster you will relieve your child of pain, and the lower the risk of possible developmental complications. Drugs are prescribed only those that are approved for this age category.
The course of treatment is selected by the doctor. Do not try to independently treat your baby or simply choose traditional medicine. You may harm your child.
Treatment of intracranial pressure
To treat our little patients, we use only painless, gentle treatment methods that do not cause discomfort to the baby.
We use methods:
- Transcranial micropolarization (TCMP) is the effect of a low-power direct electric current (less than 1 mA) on brain tissue in order to activate individual brain centers (speech, motor, psychomotor, etc.);
- Manual therapy;
- Osteopathy - treatment by the hands of a doctor, a gentle effect on the musculoskeletal system, nervous and vascular systems, internal organs;
- Acupuncture - exposure to biologically active points with microneedles;
- Pharmacopuncture - the introduction of medicinal drugs of natural origin to the source of the problem;
- Isometric kinesiotherapy - individual gymnastic techniques/exercises, according to indications, with elements of joint massage;
- Isometric kinesiotherapy using the Exart installation;
- Ozone therapy - treatment with active oxygen;
- Physiotherapy;
- Physiotherapy with enzyme preparations;
- Medical massage;
- Therapeutic droppers;
- Hirudotherapy - treatment with leeches;
- Botulinum therapy - treatment with botulinum toxin;
- Tsubotherapy is a gentle effect on the reflex points of the body.
Remember that with increased intracranial pressure in children, treatment should be comprehensive, individual and under the supervision of a doctor.
Main directions of treatment
As soon as it is determined that the child has increased intracranial pressure, consultation with the attending physician is necessary. After conducting the necessary examinations and tests, he will analyze the child’s condition and decide what to do next and what treatment regimen to prescribe.
Treatment of the disease can begin only after eliminating the causes that provoked it.
Otherwise, it will be ineffective and the likelihood of recurrence of attacks will continue. As a rule, therapy lasts several months.
The following elements are often prescribed in complex therapy:
- Taking diuretics. They help quickly remove excess fluid from the body. Harmful substances that improve the child’s well-being are removed along with it. These include products such as Furosemide, glycerin, a decoction of blueberry and parsley leaves.
- Using nootropics. They stimulate brain function. These are Actovegin, Pantogam and other drugs. They are prescribed in courses.
- Carrying out a relaxing massage. Improves blood flow and strengthens the walls of blood vessels. Children require at least 10 procedures several times a year - 2-3 times a year for 10-14 procedures.
- Procedures using tempered water, which have a beneficial effect on the movement of cerebrospinal fluid.
- Use of antiviral and antibacterial drugs.
- Use antiemetics if necessary.
- Taking a balanced multivitamin complex.
- Sedatives are prescribed to relieve nervousness.
In addition, it is recommended to follow the diet to ensure that it contains all the microelements the child needs. It is also important to follow a daily routine, take your child out for a walk and put him to bed on time.
The most extreme measure used in cases of brain injury is surgery. The operation is performed to restore the correct position of the bone structures and remove hematomas inside the skull.
Diseases caused by increased intracranial pressure
Our pediatric neurology department will help you not only make a correct diagnosis, but also undergo a course of treatment if your child has:
- Hyperactivity (attention deficit hyperactivity disorder, ADHD);
- Cerebral palsy (cerebral palsy);
- Autism;
- Delayed psychomotor development;
- Delayed speech development;
- Speech defects;
- Stuttering;
- Nervous tics;
- Enuresis;
- Sleep disturbances (sleeps poorly, sleeps little, wakes up frequently, does not fall asleep for a long time);
- Hypertonicity;
- Pyramid syndrome (pyramidal insufficiency syndrome);
- Hypertensive syndrome;
- Hydrocephalus (hydrocephalic syndrome, dropsy of the brain);
- Perinatal encephalopathy (perinatal damage to the central nervous system, PEP, PPCNS);
- Minimal brain dysfunction (MCD).
Causes of intracranial pressure:
- Birth or traumatic brain injury;
- Prematurity, pathologies during pregnancy or childbirth;
- Untimely fusion of the skull bones in a child;
- Benign brain tumors, which lead to increased blood pressure and changes in brain structures;
- Malignant brain tumors;
- Meningitis;
- Encephalitis;
- Toxic cerebral edema;
- Hydrocephalus;
- Genetic abnormalities and defects of the cerebrospinal fluid tract;
- Traumatic brain injury;
- Intracerebral hemorrhage.
WHEN does a child need to have their blood pressure measured?
In accordance with the order of the Ministry of Health of the Russian Federation dated July 3, 2000 No. 241, blood pressure should be measured at the age of 3 years (before entering a nursery school, kindergarten), 1 year before school (at 5-6 years), immediately before school (6 -7 years), after finishing 1st grade (7-8 years), at the ages of 10, 12, 14-15, 16 and 17 years.
- In children under 1 year of age, this pathology is most often associated with concomitant diseases - pathology of the kidneys, endocrine system, as well as congenital heart disease (coarctation of the aorta).
- From one to 6 years of age, pathologies of the kidneys and endocrine system are also the leading causes. Such children are observed by specialists and should be additionally examined by a cardiologist.
- From the age of 7, cases of so-called essential hypertension (primary, for unknown reasons) are detected.
- During puberty, this type of hypertension becomes the leading one.