Concussion in children - symptoms and treatment
When diagnosing SHM, it is necessary to take into account the nature of the injury and interviewing witnesses to the incident. In some cases, traces of trauma on the head and the psychological state of the child may indicate a concussion.
Since the signs of a concussion in a child are not very clear, changes in symptoms over time are important in diagnosis. Their disappearance after 3-7 days is a good reason to suspect SMG.
The difference between SHM and bruise and other forms of traumatic pathology:
- no skull fractures;
- the pressure and composition of the cerebrospinal fluid are unchanged;
- M-echo without offsets;
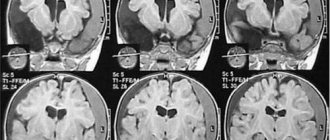
- CT and MRI without traumatic abnormalities in the parenchyma of the brain and in the cerebrospinal fluid-containing intracranial spaces.
To determine the severity of TBI, the following is assessed:
- duration of loss of consciousness in the acute phase of the injury (if it occurred);
- duration of post-traumatic amnesia (if present) and assessment of vital functions;
- degree of depression of consciousness at the time of examination (Children's Glasgow Coma Scale).
Electroencephalography and ophthalmoscopy can indirectly contribute to the objectification of concussion in the acute phase of TBI. Neurosonography (ultrasound of the brain) has become widespread in the diagnosis of TBI in children .
Ultrasound of the brain is performed on children from the first day of life until the period of closure of the large fontanelle, which is an acoustic window through which the state of all brain structures can be visualized. The study evaluates the cerebrospinal fluid system (lateral ventricles, choroid plexuses, III and IV ventricles, occipital cistern), thalamus, cerebellum, brain parenchyma, cerebral blood flow, the presence of free fluid between the brain parenchyma and the skull, as well as the skull bones.
This study allows us to exclude changes in the brain after injury - swelling of the parenchyma, displacement of the midline structures, fractures of the skull bones, areas of brain contusion and intracranial hemorrhage.[5][13]
Ultrasound signs of brain injury that exclude BMS:
- with edema of the brain parenchyma - a decrease in the echogenicity of the brain parenchyma in the first hours after injury, its increase in dynamics and normalization on days 6-7.
- in case of brain contusions - the presence of hyperechoic inclusions in the brain parenchyma against the background of a general decrease in the echogenicity of parenchyma tissue (intracranial hematomas have a higher echogenicity).
- for severe brain contusions:
- areas of the brain parenchyma of an isoechoic nature, visible only due to their additional volume;
- areas of additional volume with a moderate increase in echogenicity and an unclear contour;
- areas of additional volume with a clearly demarcated contour and an intense increase in echogenicity.
- areas of additional volume with a sharp increase in echogenicity.
- with epidural hematomas - a clearly demarcated spindle-shaped area adjacent to the skull bone, with increased or slightly decreased echogenicity, displacing the structures of the brain;
- for subdural hematomas:
- local changes in density boundaries (usually spindle-shaped), covering the entire hemisphere;
- chronic subdural hematomas with reduced echogenicity;
- for intracerebral hematomas:
- hyperechogenicity stage - lasts up to 8-10 days;
- anisoechoic stage - characterized by the appearance in the center of the lesion of zones of reduced echogenicity with an increase in size over time (10-30 days after injury);
- anechoic stage - only indirect signs of a volumetric process are visualized (1-2 months);
- the stage of subsequent residual changes with the formation of cysts or areas of brain atrophy.
- with intraventricular hemorrhages caused by trauma - the presence of an intraventricular hyperechoic zone, expansion of the lumen of the lateral ventricles and changes in the shape of the choroid plexus (rare, usually occur in the presence of multiple hematomas).[5]
Neurosonography also makes it possible to identify rare variants of the location of hematomas - the posterior cranial fossa, the pole of the frontal lobe with displacement of the echo structures of the brain and the “plus tissue” effect, the presence of free fluid along the anterior surface of the brain parenchyma. If the hematoma is located in the posterior fossa of the skull, signs of hydrocephalus are observed - expansion of the lateral ventricles of the brain and the third ventricle of the brain.[5]
Why do TBIs occur?
The causes of traumatic brain injury in children are a variety of factors. In young children, injuries occur due to parental inattention due to falling out of the crib or changing table. Domestic injuries at home, on the street and in sports are prevalent among older people. It is noteworthy that boys are injured much more often than girls.
In older childhood (after 10 years), everyday causes of TBI are less common, but the risk of developing pathology in road accidents increases.
The prognosis of the disease depends not only on the severity of the child’s condition, but also on the timeliness of medical care provided on site and in the hospital. Often the latter can cause difficulties, since in some cases of closed TBI the clinical picture develops gradually, and at first there may be no symptoms at all.
If a traumatic brain injury is suspected, children must be sent to specialized hospitals for a comprehensive examination and the necessary treatment.
Treatment
Treatment of traumatic brain injuries should be carried out in accordance with the severity. Thus, treatment of a concussion is possible on an outpatient basis, at home. More serious pathologies will require qualified medical care in a hospital. Most patients are treated in traumatology or surgical departments (less often in neurosurgical departments).
A concussion requires rest. Bed rest is prescribed for a week. Reading in bed, playing games and watching TV should be avoided. Drug treatment is limited to Phenobarbital or Diphenhydramine, vasodilators (Trental). In a hospital setting, treatment is continued for 14 days. After discharge, the child is exempted from physical education and school for the same period. In total, therapy is continued for about a month. In nutrition, preference should be given to foods rich in vitamins and minerals. It is better to avoid salty and spicy foods for a while.
A mild cerebral contusion is treated in the same way as a concussion, but the duration of hospitalization and bed rest is slightly increased. Hospital stay – 21 days, bed rest – 2 weeks. Treatment at home after discharge lasts another month. Drug therapy includes Phenobarbital, Diphenhydramine, nootropics (Piracetam), B vitamins.
For severe brain contusions, specialized medical care and surgical treatment are immediately required.
In case of open craniocerebral injuries, primary treatment of the wound is required, and after a control X-ray of the skull, the treatment area is established (in the dressing room or operating room). Depressed or splintered injuries must be operated on; in case of depressions, reposition is applied.
For localized intracranial hematomas, craniotomy is necessary to empty and remove blood clots. MRI control is required.
In case of brain dislocation, surgical treatment must be carried out.
Subsequently, if necessary, plastic surgery of bone tissue in the wounded area is performed (several weeks or months after surgery).
Damage classification
TBI can be divided into open (with damage to the meninges) and closed (if they are intact).
In the first type, the wound can be penetrating into the cranial cavity or non-penetrating.
With a closed TBI, quite often there are no external signs at all, except for minor abrasions or scratches. The damage is divided into the most common types of traumatic brain injuries in children:
- Shake.
- Compression of brain structures (blood, bone fragments).
- Bruise (mild, moderate and severe).
In the doctor's practice, children with concussions or bruises of the brain of mild or moderate severity predominate.
But, despite the existing classification, the manifestations of the disease have similar features.
Shake
Concussion is the mildest degree of injury in traumatic brain injury in children. In this case, no changes in the cerebrospinal fluid are detected; accordingly, external deformations of the skull bones and no violations of the integrity of the meninges are observed. If damage to the integrity of the skull occurs, then this is no longer a concussion, but a bruise.
Signs of a concussion
Loss of consciousness during a concussion is extremely rare and is more a matter of casuistry. But if this does happen, it develops rapidly and passes just as quickly. After the child wakes up, he will remain in a state of stun for some time: he is not able to understand where he is and what happened. Infants begin to cry loudly, twitch convulsively, and it is extremely difficult to calm them down in this state. But after some time they fall asleep. After waking up, they begin to refuse food, become capricious and cry. Subsequently, the condition normalizes and false recovery occurs.
Developing cerebral symptoms include vomiting and dizziness.
Vomiting in sick children occurs at different ages, and in infants it is characterized by frequent regurgitation. The headache is mild, disappears with time at rest and does not require the use of painkillers. The duration of pain varies and averages from 1 to 3 days.
Classic signs of a concussion in children are:
- Decreased reflexes.
- Reduction in muscle strength.
- Deterioration of pupillary response to light stimuli.
- Paresis or severe disturbances in the innervation of facial muscles. In this case, the tongue may deviate to one side.
It should be noted that the above symptoms may not develop all at once. Moreover, sometimes a completely asymptomatic course of a concussion or an erased clinical picture of the disease is possible. Instrumental and laboratory examinations are considered the most reliable for establishing a diagnosis.
In general, all symptoms practically disappear by the end of the first week. However, general health returns to normal much earlier. It is important to remember that you should not neglect the necessary bed rest, since getting up early and active games in the absence of complete recovery can cause complications.
Compression
Compression of the brain occurs due to hematomas. In children, this pathology develops extremely rarely, but their course differs significantly from that in adults.
Hematomas form at the site of application of force, often combined with fractures of the skull bones and damage to the meninges. The following types of hematomas are distinguished by location:
- Epidural (located between the bone tissues of the skull and the meninges) - often found in school-age children. They can reach large sizes. The clinical picture develops in the first 3 hours from the moment of injury.
- Subdural (blood accumulates between the dura mater and the arachnoid) - develops in children in the first years of life. Blood accumulates gradually, so the clinical picture appears only after 5 – 6, or even more hours.
- Intracerebral.
Neurological manifestations of compression of the brain are most clearly expressed with epidural hematoma. In this case, the clinic develops acutely, the child suddenly loses consciousness. Subsequently, for a short period of time, the patient’s condition normalizes with the presence of mild stupor and disorientation in time. Sometimes there may be no manifestation of pathology at all. This state is called a “light gap”. It is important that upon admission to the hospital the doctor does not pass by such a child, since, despite the absence of clinical manifestations, bleeding continues in the brain, which can lead to an extremely serious condition. At this time, the baby may only notice headaches of varying severity. And after a couple of hours or a day, when a large volume of hematoma accumulates, cerebral edema and, as a consequence, its dislocation rapidly develop. Compression of the trunk occurs in the foramen magnum, and since vital centers for the regulation of respiration and cardiac activity are located there, coma develops, quickly leading to death.
With timely diagnosis of such hematomas, urgent surgery is necessary.
What are the common signs of brain compression?
- Decreased heart rate.
- Consciousness is greatly depressed.
- Unilateral pupil dilation and lack of reaction to light.
- Paralysis, paresis of the limbs and the whole body develop.
- Paresis of the extraocular muscles.
- Rarely – emotional and motor agitation.
Symptoms of hematomas in the brain increase gradually. Therefore, it is important to examine the child half an hour after the first admission. If there is an active development of the clinical picture, then with a high degree of probability we can say about compression of the brain. There will be no such clinic for a concussion or bruise of the brain.
With a subdural hematoma, the symptoms are less pronounced, but there is no “bright gap”. It should be noted that the younger the child’s age, the more pronounced the clinical manifestations will be. In infants, for example, symptoms of TBI may consist only of frequent regurgitation, bulging fontanel and restlessness of the baby.
Therefore, parents should definitely know what signs may be observed in a child after a traumatic brain injury:
- Epileptic seizures.
- Impaired sensitivity and motor activity.
- Delay in psychomotor development.
- Strong progression or sudden disappearance of all symptoms of the pathology.
If you notice such symptoms, you should immediately go to the hospital.