Cervical spine radicular syndrome (cervical radiculopathy) is a clinical description of pain and/or neurological symptoms caused by various pathologies in which the roots of the cervical spine are compressed.
Cervical radiculopathy is much less common than lumbar radiculopathy. The annual incidence is approximately 85 cases per 100,000 population. In the younger population, radicular syndrome (radiculopathy) of the cervical spine is the result of a herniated disc or acute trauma causing local impact on the nerve root. Disc herniation accounts for 20-25% of cases of cervical radiculopathy. In older patients, cervical radiculopathy is often the result of narrowing of the intervertebral joints due to the formation of osteophytes, decreased disc height, and degenerative changes in the uncovertebral joints. Treatment of radicular syndrome of the cervical spine can be either conservative or surgical, depending on the clinical picture and the genesis of compression.
The spinal roots (C1 - C8) emerge from the cervical spine and then branch, innervating the muscles of the upper extremities (shoulders, arms, hands), which allows them to function. They also carry sensory fibers to the skin, which provides sensitivity to the skin in the area of innervation.
When the roots of the cervical spine are irritated, due to inflammation or compression, pain appears in the neck with radiation to the arms, sensory disturbances, and muscle weakness in the area of innervation of the damaged root.
Symptoms of radicular syndrome in the cervical spine can develop suddenly or gradually, and periods of exacerbation are followed by remission.
Causes of cervical radiculopathy
Any condition that somehow compresses or irritates a nerve root in the cervical spine can cause cervical radiculopathy.
The most common reasons are:
- Disc herniation. If the internal material of the intervertebral protrudes and irritates the nearby root in the cervical spine, then the development of radicular syndrome (cervical radiculopathy) is possible. If a young person (20 or 30 years old) has cervical radiculopathy, the most likely cause is a herniated disc.
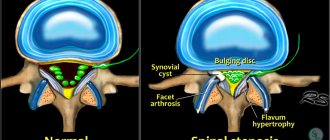
- Cervical spinal stenosis. As part of the degenerative process of the cervical spine, changes in the spinal joints can result in decreased space in the spinal canal. Spinal stenosis is a common cause of cervical radicular syndrome symptoms in people over 60 years of age.
- Osteochondrosis (degenerative disc disease). As discs in the cervical spine degenerate, the discs become flatter and stiffer and do not support the spine. In some people, this degenerative process can lead to inflammation or damage to a nearby nerve root. Cervical degenerative disc disease is a common cause of radiculopathy in people over 50 years of age.
- Cervical radiculopathy may be caused by other conditions that put pressure on the nerve roots or cause damage to the cervical nerve roots, such as tumors, fractures, infections or sarcoidosis, synovial cyst, synovial chondromatosis of the facet joints, giant cell arteritis of the radicular vessels.
- Factors associated with an increased risk of developing cervical spine syndrome include: heavy manual labor requiring lifting more than 10 kg, smoking, and long periods of driving or working with vibrating equipment.
Symptoms
Symptoms of cervical spine radicular syndrome typically include pain, weakness, or numbness in areas of the affected nerve root. The pain may be felt in only one area, such as the shoulder, or spread throughout the arm and fingers.
The type of pain may also vary. Some patients describe a dull, constant pain. However, other patients describe the pain as sharp (stabbing) or intense burning.
Patients may experience tingling in their fingers, which may also be accompanied by numbness. Feelings of numbness or weakness in the hand can also affect the ability to grasp or lift objects and perform other daily tasks such as writing or putting on clothes.
Certain neck movements, such as neck extension back, neck tilt, or rotation, can increase pain. Some patients note that the pain is relieved when they place their hand behind their head; movement can relieve pressure on the nerve root, which in turn reduces symptoms.
Types of cervical radiculopathy
Symptoms of radicular syndrome in the cervical spine depend on which root is subject to cervical compression. For example, C6 radiculopathy occurs when the nerve root that extends above the C6 vertebra is damaged.
While specific symptoms in any given patient can vary widely, there are characteristic symptoms for each level of root involvement:
- C5 radiculopathy - may cause pain and/or weakness in the shoulders and arms. A characteristic symptom is discomfort around the shoulder blades; numbness or tingling is rare.
- C6 radiculopathy (one of the most common) causes pain and/or weakness along the entire length of the arm, including the biceps, wrist, thumb, and index finger.
- C7 radiculopathy (the most common) causes pain and/or weakness from the neck to the hand and may involve the triceps and middle finger.
- C8 radiculopathy causes pain from the neck to the arm. Patients may experience arm weakness, and pain and numbness may spread along the inside of the hand, ring finger, and little finger.
- When several roots are simultaneously affected, a combination of symptoms is possible
- Symptoms may worsen with certain activities, such as sitting with the neck tilted for long periods of time (working on a computer), and improve with rest.
- But in some cases, symptoms may become persistent and not improve when the neck is in a supported resting position.
To select adequate treatment tactics for radicular syndrome in the cervical spine, it is necessary to correctly identify the cause of the symptoms. For example, cervical radiculopathy and carpal tunnel syndrome may have similar symptoms, such as arm pain and numbness, so it is necessary to accurately determine the genesis of the symptoms, which will allow targeting the actual source of the problem.
Diagnostics
If you have symptoms such as neck pain or related symptoms such as tingling, weakness, or numbness in your shoulder, arm, and/or hand, your doctor will likely start with the following:
- Patient history. The doctor collects detailed information about the presence of any previous or current diseases or conditions, accidents or injuries, family history and lifestyle. This allows you to get a better idea of what may need to be examined further.
- Physical examination. Based on examination and palpation, the doctor determines the presence of abnormalities, painful areas, as well as the range of motion and strength of the neck muscles.
- The Spurling test allows the physician to determine whether compression of the cervical spine may provoke or (temporarily) worsen a patient's radicular symptoms. This test is usually performed by having the patient tilt their head to the side where the symptoms began, and then the doctor's hand applies gentle pressure to the top of the head. This process leads to a narrowing of the foraminal openings from which the nerve roots emerge and this leads to a reproduction of the radicular symptoms that the patient experienced. If the Sperling test reproduces radicular symptoms, then cervical radiculopathy is likely present.
- In patients who already have signs of cervical myelopathy (spinal cord compression) or who have radicular symptoms following an episode of trauma (and therefore may have fractures), the Spurling test is not recommended.
Instrumental diagnostic methods
- X-ray
of the cervical spine is usually the first method for diagnosing radicular syndrome and can detect the presence of injuries, osteophytes, and narrowing of the space between the vertebrae. Radiography is considered the best initial investigation in all patients with chronic neck pain. - CT (MSCT)
- CT scanning provides good visualization of bone morphology and can be a useful diagnostic tool for the evaluation of acute fractures. The accuracy of diagnosing disc herniations in the cervical spine using CT imaging ranges from 72-91%.
CT scans with myelography have an accuracy approaching 96% in diagnosing cervical disc herniation. In addition, the use of contrast material makes it possible to visualize the subarachnoid space and assess the condition of the spinal cord and nerve roots.
- MRI
- MRI has become the method of choice for imaging the cervical spine and can detect a significant proportion of soft tissue pathologies, such as disc herniation. MRI can detect ligament tears or disc herniation that cannot be detected by other imaging modalities. MRI can clearly visualize the entire spinal cord, nerve roots, and spinal column. MRI has been found to be quite useful in assessing the amount of cerebrospinal fluid (CSF) surrounding the spinal cord when evaluating patients with spinal canal stenosis:
- EMG (ENMG)
- Electrodiagnostic research methods are important for identifying physiological disorders of the nerve root and excluding other neurological causes of the patient's symptoms. EMG (ENMG) studies have been shown to be useful in the diagnosis of radiculopathy and correlate well with the results of myelography and surgical treatment.
Dizziness caused by pathology of the cervical spine
Dizziness and otoneurological symptoms are described in various types of pathology in the neck: traumatic injuries of the neck and spinal cord [4, 5, 10], cervical osteochondrosis [2], occlusion of the vertebral artery (VA) [1, 3, 12] and strokes caused by VA injuries [1, 11, 13, 15], VA dissection, in connection with neck movement or manipulation of the cervical spine [6, 7, 8, 9, 11, 14].
The identification of vertebrogenic dizziness is due to the prevalence of the pathology among young people, the severity of the disease, the variety of symptoms, and the occurrence of strokes during manipulation of the neck.
A distinctive feature of vertebrogenic dizziness is an acute onset associated with a certain position of the head (bending forward, throwing back, sharply turning to the side, etc.), often in the morning, after sleep. Dizziness, which occurs as a result of a change in the position of the head, can be caused by both irritation of the inner ear and the central vestibular structures of the brain (trunk, cerebellum). Compression of the arteries develops with osteophytes and lateral disc herniations in uncovertebral areas, anterior exostoses of the articular processes, as well as with subluxation.
The anatomical and topographical features of the VA include the location of most of its extracranial part in the spinal canal, where it is displaced and compressed by osteophytes or articular processes in various degenerative diseases, in particular osteochondrosis (Fig. 1).
An otoneurological examination of the patient allows for accurate topical diagnosis, as well as differential diagnosis from peripheral dizziness caused by other diseases: Meniere's disease, benign paroxysmal positional vertigo, vestibular neuronitis.
Barre (1926), who first drew attention to the connection between otoneurological symptoms and pathology in the neck, described them under the name “posterior cervical sympathetic syndrome,” pointing out the importance of the connection between the head and neck through the sympathetic nervous system.
It has been shown that an in-depth study of the VA, taking into account not only the diameter and characteristics of the blood flow, but also using functional tests, allows us to identify points important for the differential diagnosis between hemodynamically significant and insignificant extravasal compression of the VA.
The damaging effect of extravasal compression factors is directed primarily at its nerve plexus. Irritation of the spinal nerve, increasing the tone of the VA, can reduce the velocity of volumetric blood flow in it by 30% of the initial value, by 40% in the branches of the main artery, in particular the inner ear [1].
Thus, the functional state of the spinal nerve and structural changes in the VA are the basis for the development of blood flow insufficiency in the vertebrobasilar system (VBS) at the extra- and intracranial level. As various authors emphasize, cochleovestibular syndrome can develop with circulatory insufficiency in the VBS, both in the area of the inner ear and in the area of the vestibular nuclei and pathways of the brain stem and cerebellum.
In addition to disturbances in the blood supply to the VBS, impaired proprioceptive nerve impulses from the structures of the neck also play a role in the pathogenesis of vertebrogenic dizziness. Movements in the joints of the cervical vertebrae and discs altered by osteochondrosis and spondyloarthrosis, as well as the resulting tonic muscle tension, contribute to the development of inadequate afferent impulses and incorrect assessment by the vestibular system of information about the position of the head, which causes a feeling of dizziness and imbalance.
The purpose of the work carried out at the Scientific Center for Neurology of the Russian Academy of Medical Sciences was to identify clinical features and otoneurological symptoms in patients with vertebrogenic dizziness against the background of pathological changes in the cervical spine, as well as to compare vestibular disorders with structural changes in the vertebral column, blood pressure level, and the condition of the internal jugular veins.
We examined 115 patients with acute and chronic circulatory failure in the VBS, including 47 patients with degenerative-dystrophic changes in the cervical spine, of which 33 had degenerative changes (osteochondrosis), 9 had craniovertebral pathology, Kimmerli’s anomaly, in 4 patients there was an anomaly in the entry of the VA into the canal at the level of C4, and spinal canal stenosis in one patient. The age of the patients ranged from 28 to 74 years.
The main diseases against which vestibular disorders developed were arterial hypertension (AH) in combination with atherosclerosis, vegetative-vascular dystonia, and osteochondrosis.
All patients underwent a complete classical otoneurological examination, including the study of spontaneous and experimental vestibular reactions (rotational and caloric tests) and hearing. The auditory analyzer study was carried out using audiometry and auditory evoked potentials.
Structural changes in the great arteries of the head (MAG) and hemodynamic parameters of blood flow through the VA and internal carotid artery (ICA) were studied using duplex ultrasound scanning of the MAG (MAG DS) with functional tests, in some cases during spiral computed tomography (SCT), magnetic resonance angiography.
Treatment
Conservative treatment of radicular syndrome of the cervical spine may include the following treatment methods:
Rest or change in activity
. Wearing a cervical collar during acute pain. Cervical radiculopathy often resolves on its own, especially if symptoms are mild. Limiting strenuous activities such as playing sports or lifting heavy objects or improving your posture while sitting or driving may sometimes be sufficient treatment.
Exercise therapy.
Exercise and stretching may help relieve symptoms. A physical therapy doctor can develop an individual plan for a specific patient. Exercise therapy is the most effective method of treating radicular syndrome in both the short and long term. Exercises aimed at opening the intervertebral foramen are the best choice for reducing the effects of compression on the root. Exercises such as contralateral rotation and lateral flexion are the simplest forms of exercise that are effective in reducing the symptoms of radicular syndrome and increasing range of motion in the neck. Exercises can also be performed to strengthen the muscles, which will improve neck stability and reduce the risk of developing nerve root irritation in the future, if the root compression is not due to reasons for which exercise therapy does not have a therapeutic effect. During the initial stages of treatment, muscle strengthening should be limited to isometric exercises in the involved upper extremity. Once acute symptoms have resolved, progressive isotonic strengthening can begin. Initially, resistance exercises should be done with light weights and frequent repetitions (15-20 repetitions). It is necessary to engage in exercise therapy for a long time, periodically adjusting the volume and intensity of exercise with a physical therapy doctor.
Medicines
. To reduce pain symptoms, it is possible to use various anti-inflammatory drugs (diclofenac, movalis, ibuprofen) and muscle relaxants.
If medications in this group do not have an effect, then opioids may be added for a short period of time.
Cervical epidural steroid injections
used in patients refractory to other treatment methods. When performed correctly by experienced doctors under X-ray control, in most cases of radicular syndrome in the cervical spine, a fairly good effect can be achieved.
Manual therapy
. Manipulations during manual therapy can remove blocks and improve the mobility of motor segments and thus reduce symptoms.
Traction therapy
. Skeletal traction is often used in the treatment of radicular syndrome in the cervical spine. Tractions are performed on specialized traction tables with a controlled load. Traction allows you to slightly reduce root compression by increasing the distance between the vertebrae. •
Acupuncture
, along with other methods, is used in the treatment of radicular syndrome in the cervical spine. This treatment method improves conductivity in nerve fibers, reduces pain and restores sensitivity.
Physiotherapy
. Modern methods of physiotherapy, such as cryotherapy or Khivamat, as well as traditional methods (electrophoresis, phonophoresis) are widely used both in the acute stage of radicular syndrome and in a complex of rehabilitation techniques.
Cervical spine instability - symptoms and treatment
If instability is present, treatment should be comprehensive. Prevention plays a huge role.
Treatment consists of several stages.
Drug treatment:
- non-steroidal anti-inflammatory drugs are intended to relieve inflammation, reduce and cure pain;
- muscle relaxants help reduce muscle spasm and tone, help reduce compression of the nerve roots;
- B vitamins nourish nervous tissue, restoring and protecting it;
- D vitamins and calcium supplements are prescribed to patients with osteoporosis.
Physiotherapeutic treatment.[1][2][5]
It is an effective means of treating pain, relieving inflammation, restoring nerve and muscle tissue. Physiotherapeutic treatment also allows you to deliver a medicinal substance to the lesion using an electric current. In physiotherapeutic treatment the following is used:
- techniques that relieve inflammation: electrophoresis, magnetic therapy, UHF therapy;
- techniques that promote tissue regeneration: laser therapy, mud therapy.
Novocaine blockade[1][2]
It is a method of relieving acute pain by delivering a medicinal substance directly to its source. It is carried out by a neurologist in a medical institution (not at home!) after a special training course. The medicinal substance can be a solution of Novocaine 0.5% or a solution of Lidocaine 2%. You can also add solutions of vitamins or hormones. The composition of the administered substance is selected by the doctor in accordance with clinical indications in the absence of contraindications to the administered drugs. It should be noted that a neurologist should not inject the substance into the intervertebral joints; this procedure can only be performed by neurosurgeons.
Spinal immobilization.[2][3][5]
It is one of the first remedies for exacerbation. It is carried out with a special collar that limits mobility. It is prescribed only by a doctor and is selected strictly individually according to the size of the neck. It is recommended that the selection be carried out in specialized orthopedic salons. The mode of wearing a collar is also recommended depending on the cause of the exacerbation.
Manual therapy.[3][5]
It is a means of mobilizing the vertebrae. It is forbidden to perform during the acute period of injury. Performed by a chiropractor on the recommendation of a neurologist after examination.
Physiotherapy.[3]
It is one of the most effective means of prevention and treatment. The course is developed for the patient depending on the cause of instability, as well as the condition of the spine. The goal of gymnastics is to strengthen muscle tissue (ligaments and muscles). If gymnastics is carried out after an injury or surgery, it is carried out only under the supervision of a neurologist or instructor-methodologist in the exercise therapy room. After training, the course is carried out at home independently.
Reflexology , particularly acupuncture .
It is a means of relieving pain, restoring muscle and nervous tissue, treating associated symptoms: improving blood circulation, improving sleep. It is performed only by a reflexologist using special needles.
Surgery.[1][5]
Is a rare practice. Performed in childhood in case of proven structural anomalies. In adult practice, spinal fusion is more often performed. It consists of implanting a structure made of metal plates and fixing elements. Its task is to prevent excessive mobility of the spine. The operation is used after injuries, discotomies and laminectomies. The last two are performed for spinal hernias.
Surgery
If conservative treatments do not provide pain relief, or if neurological symptoms such as numbness and arm weakness continue to worsen, then surgery may be considered.
The following surgical techniques are most often used in the treatment of cervical radiculopathy:
Anterior cervical discectomy and fixation
. This surgery is performed through a small incision in the front of the neck to remove the herniated disc, and then fixes that motion segment of the cervical spine to ensure spinal stability. This is the most common operation for root decompression.
Replacement of an intervertebral disc with an artificial disc
. This technique allows you to replace the fixation of the vertebrae. A potential advantage of this technique is that it aims to maintain mobility at this level of the cervical spine rather than fusion of two vertebrae.
Surgical treatment of radicular syndrome in the cervical spine can effectively reduce symptoms and restore conduction through nerve fibers. According to statistics, the efficiency rate ranges from 80% to 90%. As with any surgery, there are some risks, but most often the benefits of surgery outweigh the risks.
Symptoms of occipital neuralgia
Primarily, neuralgia of the greater occipital nerve is characterized by headache. Her character is very specific:
- pain is concentrated behind the ears, in the occipital region, lower part of the neck, as well as in the eye area or above them;
- attacks occur unexpectedly when turning the head or touching the area of innervation, often when touching the skin of the head;
- painful sensations are localized on one side, although bilateral damage occasionally occurs;
- the pain looks like “lumbago” and disappears as suddenly as it begins;
- bright light causes pain in the eyes.