Intracranial hypertension clinic
The time during which the pressure rises characterizes the severity of complaints and symptoms.
Main complaints of intracranial hypertension:
- constantly intensifying long-term headache, which is perceived as pressing, is located in the temples, intensifies with physical activity, reaching a maximum in a horizontal position, after a night's sleep;
- nausea, vomiting. More often in the morning, sometimes without previous nausea;
- hiccups;
- double vision;
- changes in vision that occur when the head position changes;
- drowsiness;
- disturbance of consciousness;
- breathing disorder.
Ten causes of intracranial hypertension:
- Tumor of the brain or spinal cord;
- Benign hypertension;
- Hydrocephalus;
- Stroke;
- Meningitis;
- Traumatic brain injury;
- Encephalopathy due to high blood pressure;
- Brain swelling;
- Severe heart failure;
- Obstructive pulmonary disease.
Life-threatening complications of intracranial hypertension:
- compression of the brain;
- extrusion of the brain from one part of the skull to another (herniation)
ICP on MRI
Yuri, Voldgograd
May 18, 2019
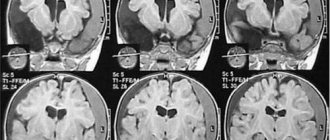
For a very long time I have been bothered by pain behind the eye sockets and heaviness of the head from the forehead to the crown of the head, when the head is tilted there is a strong bursting headache (in childhood this did not happen until I was 15 years old), there is no nausea, dizziness is rare, ringing in the ears (often) The neurologist sent me for an MRI of the eye sockets, vessels and brain: MRI data from the disk I attach on Yandex disk link: https://yadi.sk/d/81L4XqaZ-zYEYw ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ ⠀⠀⠀⠀⠀⠀⠀⠀⠀ MRI photo of the descriptive part: ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ https://a.radikal.ru/a10/1905/37/38b0a550131e.jpg ⠀ ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ https://d.radikal.ru/d10/1905/52/052d956aba8e.jpg⠀⠀⠀⠀⠀ ⠀⠀ ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ https://c.radikal.ru/c30/1905/7a/33fbcc2e7d2a.jpg ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ ⠀⠀⠀ ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ https://b.radikal.ru/b15/1905/28/cc05c81a71c2.jpg ⠀⠀⠀⠀ ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ ⠀⠀⠀ ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ ⠀⠀⠀⠀⠀⠀⠀⠀⠀ ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ MRI data for pathological changes in the orbital area were not detected, moderate expansion of the subarachnoid spaces of the optic nerves.⠀ ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ ⠀ ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ ⠀⠀⠀⠀⠀ Brain-changes the substances of the cerebral hemispheres, brainstem and cerebellum are not visualized, moderate expansion of the subarachnoid spaces of the optic nerves, the developing sella turcica (the pituitary gland tissue is normal, 3 mm thick in the central section due to prolapse of the suprasellar cistern into the sellar cavity), lll ventricles are slit-like, INDIRECT SIGNS OF INTRACRANIAL HYPERTENSION. ⠀ ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ ⠀⠀⠀⠀⠀⠀⠀ MRI series of angiograms performed in TOF mode in axial projection - the arterial circle is not closed (development option), coiling of the left ICA. ⠀ Venography - no pathological changes in the veins of the brain were detected. ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ ⠀⠀⠀⠀⠀⠀ MRI neck - Picture of dystrophic changes in the cervical spine: chondrosis C2-Th1, protusion of the C5-6 intervertebral disc with narrowing of the spinal canal, dorsal diffuse protrusion of the C6-7 intervertebral disc (with narrowing of the vertebral canal). It is impossible to exclude the presence of unevenness in the course of the V2 segment of the vertebral arteries. Craniverbal transition normal.⠀ ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ Ultrasound of neck vessels - https http://b.radikal .ru/b43/1905/4e/7b1a3cc392a2.jpg Speed indicators are relatively symmetrical. TI is not thickened. ASb is not detected. The IJV is compressed by hypertrophied neck muscles. Vessel with straight stroke. Ultrasound of the vessels of the head - Speed indicators of blood flow in the middle, anterior, posterior cerebral arteries, vertebral arteries at the level of the V4 segment are not reduced. The speed indicators of blood flow through the main artery are not reduced. ⠀⠀ ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ EXAMINATION BY AN OPHTHALMOLOGIST: https://d.radikal.ru/d07/1905/96/0206607d718c.jpg Vascular angiopotia according to the hypertensive type of both eyes (veins strongly dilated, arteries narrowed, arteries compress veins in many places), eye pressure is normal. Assigned: Broxinac - 1 month ⠀⠀⠀⠀⠀⠀⠀ ⠀⠀⠀⠀⠀ INSPECTION Cardiologist: PMK-1st.RVNS.Prehypertension (133-135 on 60) Hormones are normal, kidneys are normal, Thyroid is normal. ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ ⠀⠀⠀⠀⠀⠀⠀⠀ Lor doctor: vasomotor rhinitis (X-ray of the sinuses is fine) ⠀⠀⠀⠀⠀ ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ ⠀⠀⠀⠀⠀⠀⠀ X-ray of the cervical department: Spondylosis, osteochondrosis, left-sided scoliosis C form https://radikal.ru/lfp/d.radikal.ru/d25/1905/1c/beec0d5d78a3.jpg/⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ REG: Pulse blood filling in the basin of the vertebral arteries and in the basin of the left internal artery (Fms by 32%, Oms by 28%, Omd 12%) The tone of the main arteries is increased in the basin of the vertebral arteries, the tone of large arteries is reduced in the basin of the right internal carotid, the tone of the medium and small arteries is increased in the basin of the internal carotid, peripheral resistance is increased in the basin of the left vertebral arteries. In the basin of the left vertebral artery there are signs of obstructed venous outflow. ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ ⠀⠀⠀⠀⠀⠀⠀⠀⠀ ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ Treatment: diacarb 10 days 1 table. on an empty stomach, then 2 days a week of any kind (headaches became less, pain remained behind the eyes). They also prescribed Troxerutin and Tanakan (but as I understand it, they do not have an evidence base, probably that’s why they didn’t really help), so the hedgehog sirdalud and our Shlantsa collar for 2 hours each.⠀⠀⠀⠀⠀⠀ ⠀⠀⠀⠀⠀⠀ ⠀⠀ All this doesn’t really help, is it necessary to do a lumbar puncture for an accurate diagnosis, and subsequently an operation, if not necessary then what to do, life becomes unrealistic. According to the ophthalmologist and MRI, everything points to symptoms of ICP
The question is closed
Read also
Myelitis
Myelitis is a neurological pathology characterized by inflammation of the gray and white matter of the spinal cord, which leads to damage to myelin (the substance that forms the sheath of nerve fibers) and the axon (the process...
Read more
Neurogenic bladder
In a healthy person, the process of urination is carried out in the form of a voluntary reflex act, and we can control it. However, this is not the case with this disease. Patients are extremely...
More details
Perinatal encephalopathy
Perinatal encephalopathy is a frequently encountered concept in the practice of pediatricians and pediatric neurologists! What it is? Literally, “perinatal encephalopathy” means “damage to the brain in the perinatal...
More details
Chiari malformation
What is Chiari Malformation? Chiari malformation (formerly Arnold-Chiari malformation) is a congenital defect of brain development that involves the dislocation of the cerebellar tonsils into the spinal canal through the large…
More details
Syringomyelia
Syringomyelia is a disease caused by the formation of spaces in the substance of the spinal cord filled with cerebrospinal fluid. They expand the spinal cord at the level of the lower cervical and thoracic regions...
More details
Intracranial pressure
The integral components of the cranial cavity that determine the amount of intracranial pressure are: the cerebral contents themselves: the brain and pathways (85%), cerebrospinal fluid (CSF) (10%), as well as blood-filled vessels (5%).
Normally, this ratio of the components of the cranial cavity maintains intracranial pressure at a constant level - about 0-13 mmHg.
It is necessary to take into account the fact that all of these structures: the brain, cerebrospinal fluid, blood are located in a closed cavity formed by hard, poorly stretchable walls - the skull. Therefore, in the case of an increase in at least one of the components of the cranial cavity, this inevitably leads first to a limited decrease in the other component, and, subsequently, to an increase in intracranial pressure.
The amount of “reserve” for compensation of intracranial pressure is individual and increases with atrophy (decrease in volume) of the cerebral cortex, after removal of part of the brain matter during neurosurgical interventions, as well as with a long-term increase in “excess” volume in the cranial cavity.
Thus, in the case of an increase in the volume of the cerebral component, for example, with a brain tumor, especially a slowly growing one, intracranial pressure can remain normal for a long time due to a compensatory decrease in the content of cerebrospinal fluid and/or blood in the vessels of the brain - this is the so-called cerebral compliance. It’s another matter when “extra” volume appears in the cranial cavity in a short period of time, as happens with hemorrhage, cerebral edema, or a rapidly growing tumor. In these cases, intracranial pressure increases rapidly, despite compensation mechanisms.
Thus, in simplified terms, we can describe the doctrine developed by A. Monroe and J. Kelly, according to which: the appearance of additional intracranial volume leads to a conflict of intracranial components.
The main causes of increased intracranial pressure can be divided into intracranial, that is, associated with pathological processes in the cranial cavity, and extracranial.
Intracranial causes include:
- Volumetric lesions of the brain: tumors (Fig.), abscesses, etc.;
- Hydrocephalus is a disease accompanied by disruption of the processes of formation and/or disposal of cerebrospinal fluid (see another article);
- Stroke - ischemic/hemorrhagic (hemorrhage) (Fig.);
- Inflammatory diseases of the brain - meningitis/encephalitis;
- Traumatic brain injury.
Extracranial causes:
- Diseases that cause a sharp increase in protein content in the cerebrospinal fluid - spinal cord tumors, Guillain-Barré syndrome;
- Water-electrolyte imbalance - Na level in the blood;
- Severe blood pressure - acute hypertensive encephalopathy;
- Eclampsia is an extreme degree of manifestation of gestosis (toxicosis) in pregnant women;
- Disturbances of homeostasis (internal environment of the body), hypoxia (insufficient supply of oxygen to tissues), leading to cerebral edema;
- Congestive heart failure is a disease associated with disruption of the normal function of the heart with a decrease in its contractile function;
- Chronic obstructive pulmonary disease (COPD) is a disease associated with exposure to tobacco smoke on the respiratory system;
- Impaired outflow through the veins coming from the brain, for example, with tumors of the upper lobe of the lung and other diseases;
- Pericardial effusion is an accumulation of free fluid in one of the membranes surrounding the heart muscle.
The main symptoms of increased intracranial pressure (hypertension):
- Headache, often of a bursting nature, occurring mainly in the morning (later it can become permanent), aggravated by coughing, sneezing, straining, changing body position (tilting the head), not relieved by sleep - a growing headache!
- Nausea ± vomiting - the latter is most typical for tumors in the posterior cranial fossa (Fig.), may be the first symptom and occur without previous nausea.
- Persistent hiccups.
- Changes in the level of consciousness - drowsiness in mild cases, coma in more severe cases.
- Double vision is especially common when looking at distant objects (due to compression of the abducens nerve).
- Congestive optic discs - upon examination, the ophthalmologist can identify characteristic changes in the fundus (the exception is the early stages of acutely developed intracranial hypertension).
- Episodes of “blurred” vision are associated with impaired venous outflow from the eyeball.
- Cushing's triad - an increase in arterial (mainly systolic) pressure (BP) + a decrease in heart rate (bradycardia) + a decrease in breathing (bradypnea) - is associated with compression of the vital centers of the brain stem. An increase in blood pressure is protective in nature, helping to improve blood supply to the brain stem.
Diagnostics is based on the analysis of complaints, identification of concomitant diseases, medical examination, as well as additional examination methods, such as:
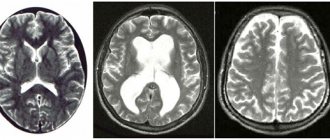
- CT/MRI of the brain - to exclude structural damage to the brain;
- Lumbar puncture - identifying changes in the cerebrospinal fluid, measuring intracranial pressure. In the absence of contraindications!
Laboratory and instrumental methods - to diagnose extracranial causes of increased intracranial pressure.
Treatment consists of treatment of the underlying disease leading to increased intracranial pressure and/or the use of drugs that help reduce intracranial pressure. First of all, these are osmotic, often in combination with loop diuretics, glucocorticosteroids (especially in the case of a tumor process), a carbonic anhydrase inhibitor for benign intracranial hypertension (see another article).
In conclusion, I would like to emphasize that, despite the desire to provide in this article the most complete information about increased intracranial pressure, you should not resort to self-diagnosis and self-medication, since, as practice shows, this can not only cause a blow to your health, but also cause a waste of time and material resources.
If you are concerned about the state of your health or the health of people close to you, do not put off visiting a doctor (neurologist).
What is magnetic resonance imaging of the brain
The brain can be considered one of the most difficult organs for the early detection of pathologies, anomalies and disorders. Not every hardware diagnostic method can handle it. Thus, thick cranial plates do not allow examining the head structures of an adult using ultrasound of the head. Radiography shows the condition of the skull bones well, but it is impossible to obtain detailed results of the condition of the white and gray matter, the vascular bed and the pituitary gland. Therefore, magnetic resonance imaging plays an invaluable role in diagnosing brain pathologies.
This method uses harmless magnetic fields and radio waves and allows you to see the area under study in three dimensions. During the examination, the patient's body is exposed to electromagnetic waves. This causes the vibration of a hydrogen atom in the brain cells, which is picked up by the tomograph's computer, digitized and turned into a series of three-dimensional images. The examination procedure itself is absolutely safe, since it does not involve radiation exposure, unlike CT. Since the brain is 80% water, there is a very strong resonance effect, and MRI images of the brain have very good tissue contrast. The information content of the method is so high that it allows identifying possible pathological changes up to 1 mm in size.
The process of performing an MRI of the skull
The MRI equipment itself is a cylindrical machine with a tunnel in the middle, which is surrounded by a magnet. A table slides into this tunnel and the patient lies on it.
- To perform an MRI of the skull, the patient is placed on a table and secured to it with special belts and ties. For convenience and immobility, there are bolsters that secure the body.
- After fastening, the head is prepared for examination. Wired sensors that conduct and receive radiomagnetic waves are attached to it. It is these signals that provide information to the computer, which is then processed by the program and shows all sorts of pathologies and causes of intracranial pressure.
- Contrast-enhanced MRI uses contrast material that is injected through a catheter into a vein in the arm. In order to avoid clogging of the veins, which interferes with the passage of the substance, saline solution is poured in front of it.
- After preliminary preparation, the patient is placed on the table in the apparatus tunnel, and all medical staff must leave the room.
- The results of the study are given to the patient immediately after the procedure. If the examination is unsuccessful, the device may produce a blurred image, and a similar examination is carried out. When finished, the doctor removes the catheter.
The standard examination time is 45 minutes. At this time, several pictures are taken (one image - 5–8 minutes).
When scanning the head, magnetic resonance imaging has its own characteristics. In the process, blocks of sections of head tissue are made in layers. One level is 5 mm thick, and in one photo scan information is read from approximately 20 levels.
The accuracy of the survey results is determined by the magnetic field induction (measured in Tesla).
Remember! While the image is being taken, the patient must lie still and do everything the doctor says.
Contraindications
Brain tomography has two main contraindications:
- the presence of ferromagnetic metal in the body, for example, steel prostheses, iron bullets, shrapnel, Ilizarov apparatus;
- the presence of pacemakers whose passports do not contain a mark indicating compatibility with MRI.
Dental implants and crowns are not a contraindication to the examination. You should inform your doctor about their presence, as some of them can sometimes produce light artifacts on images. The magnetic field itself does not negatively affect the composition and material of dental implants and does not lead to cracks, chips or movement. Most braces will also not be a limitation to magnetic resonance imaging. However, it may happen that the light effect from them will be so strong that the quality of diagnosis will decrease, and the doctor will not be able to make a high-quality description of the tomograms. For some, tattoos and permanent makeup can cause discomfort. If pigments containing metal were used during tattooing, the patient may experience a feeling of intense heating of the skin or even a burning sensation in the areas where the ink was injected subcutaneously. If the subject has undergone surgery to install vascular clips, MR examination should be postponed for 6 months after surgery. If you are unsure whether you can have an MRI, always consult your doctor.
How to do an MRI of cerebral vessels
After the patient enters the radiologist's office, the doctor asks several questions about bothersome symptoms and contraindications for the procedure. The patient is asked to remove all metal objects and lie down on the tomograph bed. Normal operation of the tomograph is accompanied by noise, knocking and other loud sounds; this should not be alarmed. In our medical center, each patient is given headphones that play pleasant, calm music during the examination.
Preparation for MRI of the head and blood vessels
The patient is given a special button in his hand, which can be pressed during the procedure to inform the doctor about a sudden deterioration in health.