Causes of ganglioneuritis
The very first cause of this disease is an infectious process. The causative agents can be:
- acute infections: measles, dysentery, sepsis, diphtheria, tonsillitis or influenza;
- chronic infectious diseases (syphilis, tuberculosis, rheumatism).
The cause of ganglioneuritis of the pterygopalatine node can be complicated dental caries, and adnexitis or prostatitis (in men) can provoke sacral ganglionitis. In rare cases, ganglioneuritis can be provoked by a tumor (ganglioneuroma or secondary metastatic process), then the disease is toxic in nature.
Risk factors for the occurrence of ganglioneuritis will be nervous overstrain, hypothermia, constant fatigue, alcohol addiction, and operations performed in the ganglion area.
Details of ganglioneuritis
You need to understand that an isolated anomaly that affects one sympathetic department in the field of neurology is called ganglionitis, and if the pathology has spread to nearby areas of the peripheral nerve, doctors call this process ganglioneuritis. If a person is diagnosed with problems in the nodes and spinal region, then the disease is ganglioradiculitis. In addition to these varieties, doctors distinguish truncitis, an inflammatory process that occurs in several sympathetic areas.
General symptoms of ganglioneuritis
Symptoms of ganglioneuritis depend on the level of damage; it has a complex clinical picture. Pain syndrome will be the main symptom in the clinical picture. The pain is characterized by a strong burning and bursting character, patients also note a feeling of pulsation.
Patients often cannot accurately indicate the source of pain because the disease is diffuse. Patients describe pain in the entire half of the body, focusing on the fact that the pain is constant and does not change with movement. Increased pain occurs when the weather changes, stressful situations, or after eating.
In addition to the pain syndrome with ganglioneuritis, there is also a loss or partial impairment of sensitivity in the form of hyperesthesia (increased sensitivity) or, conversely, hypoesthesia (decreased sensitivity). Sometimes paresthesia (a feeling of numbness, a sensation of “pins and needles”, tingling or lethargy) is also noted.
There are cases of neurotrophic and vasomotor disorders that are expressed in the area of localization of the affected ganglion and the nerve fibers associated with it. If the disease is long-term, sleep disturbances, emotional instability, and the development of neurasthenia, asthenia, and hypochondriacal syndrome may occur.
The big picture
One of the most noticeable symptoms during the progression of inflammatory activity is the formation of pain. It can manifest itself in the form of pulsation or swelling of the injured areas. In the course of multiple work with people suffering from the presented illness, patients quite often could not report with 100% confidence the exact location of the painful sensations and with what strength it manifests itself. In some situations, patients say that the pain flows over the entire half of the body or moves to the opposite part.
The main feature of the described disease is that during human physical activity, the pain syndrome does not increase the level of impact. Many say that an increase in the degree of discomfort occurs after eating food, changing weather conditions, emotional shock and other events. Along with the above symptoms, people complain of disruptions in the functioning of their sensory abilities. For example, some experience numbness in the limbs, a sensation of goosebumps, slight tingling, etc. Patients experience sleep-related problems, the development of neurasthenia, asthenia and other unfavorable processes.
Ganglioneuritis of the upper cervical ganglion
The clinical picture of ganglioneuritis of the upper cervical ganglion is characterized, first of all, by the symptoms of Bernard-Horner syndrome. The inflammatory process in this ganglion provokes the development of Pourfur du Petit syndrome (enlarged palpebral fissure, exophthalmos). The inflammatory process affects the functionality of the thyroid gland and causes the appearance of hyperthyroidism. Secretory and vasomotor disorders are observed (hyperhidrosis, redness in half of the face, decreased intraocular pressure). Sensitivity disturbances are observed in the area of the second rib. Possible voice changes or laryngeal paresis. Sometimes patients feel severe pain spreading to the jaw area. Due to the inability to pinpoint the exact source of pain, people often mistakenly resort to dental treatment, which for known reasons does not produce any results.
Ganglioneuritis
The main clinical sign of ganglioneuritis is severe pain. It is characterized by widespread burning pain, which may be accompanied by a feeling of pulsation or fullness. Patients with ganglioneuritis cannot accurately indicate the location of pain due to its diffuse nature. In some cases, with ganglioneuritis, pain spreads to the entire half of the body or to the opposite side. A distinctive feature of pain with ganglioneuritis is the absence of its intensification with movement. Most patients indicate that increased pain may occur in connection with food intake, weather changes, emotional stress, etc.
Along with pain syndrome, ganglioneuritis is manifested by various sensory disturbances. This may be a decrease in sensitivity (hypoesthesia), increased sensitivity (hyperesthesia) and paresthesia - discomfort in the form of numbness, crawling sensations, tingling, etc. Ganglioneuritis is also accompanied by neurotrophic and vasomotor disorders expressed in the innervation zone of the affected ganglion and nerves. Long-term ganglioneuritis is often accompanied by increased emotional lability of the patient and sleep disturbance; the development of asthenia, hypochondriacal syndrome, and neurasthenia is possible.
Depending on the group of sympathetic ganglia affected, ganglioneuritis is classified into cervical, thoracic, lumbar and sacral. Cervical ganglioneuritis, in turn, is divided into upper cervical, lower cervical and stellate.
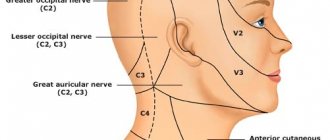
Cervical ganglioneuritis
Ganglioneuritis of the upper cervical ganglion is characterized by Horner's syndrome: ptosis, miosis and enophthalmos. When this ganglion is irritated, Pourfur du Petit syndrome develops (widening of the palpebral fissure, mydriasis and exophthalmos), and a stimulating effect on the thyroid gland occurs, leading to the occurrence of hyperthyroidism. Secretory and vasomotor disorders of upper cervical ganglioneuritis are manifested by hyperhidrosis and redness of the corresponding half of the face, and a decrease in intraocular pressure.
Changes in sensitivity with cervical ganglioneuritis are noted above the 2nd rib. Possible paresis of the larynx, accompanied by hoarseness. In cases where ganglioneuritis of the upper cervical ganglion is accompanied by a pronounced pain syndrome affecting the dental area, patients are often unsuccessfully treated by a dentist and even go through the mistaken extraction of teeth.
Ganglioneuritis of the lower cervical ganglion is accompanied by the spread of sensitivity disorders to the 6th rib. These disorders also affect the hand, leaving only its inner surface intact. In the hand there is a decrease in muscle tone, cyanotic coloration of the skin (diffuse or only the fingertips). The corneal, conjunctival, jaw, pharyngeal and carpo-radial reflexes are reduced. With lower cervical ganglioneuritis, prolapse of the auricle on the side of the affected node is possible.
Ganglioneuritis of the stellate ganglion is manifested by pain in half of the chest on the affected side. The area of pain and sensitivity disorders has the appearance of a “half-jacket”. Often the pain radiates to the upper limb, while the pain syndrome resembles an attack of angina and requires differential diagnosis with coronary heart disease. There is a violation of the motor skills of the fifth finger on the hand.
Thoracic, lumbar and sacral ganglioneuritis
Gangleoneuritis of the upper thoracic sympathetic nodes is manifested not only by sensory disturbances and pain, but also by vegetative-visceral disorders. Possible pain in the heart area, difficulty breathing, tachycardia.
Ganglioneuritis of the lower thoracic and lumbar sympathetic nodes is characterized by pain, sensory disorders, vascular and trophic disorders of the lower torso and lower extremities. When the sciatic nerve is involved in the inflammatory process, pain radiates to the corresponding thigh with a characteristic clinical picture of sciatic nerve neuropathy. Vegetative-visceral disorders manifest themselves in the abdominal organs. Sacral ganglioneuritis may be accompanied by itching of the external genitalia and dysuric disorders. Women may experience menstrual irregularities and acyclic uterine bleeding.
Other forms
Ganglioneuritis of the pterygopalatine ganglion is accompanied by clinical symptoms of trigeminal neuralgia in the area of the orbit, nose and upper jaw (innervation zone of the second branch), hyperemia of half the face, lacrimation from the eye on the affected side and copious discharge from the nose on the same side. Ganglioneuritis of the geniculate ganglion is characterized by paroxysmal pain in the ear, which often radiates to the back of the head, face and neck. On the affected side, the development of neuritis of the facial nerve with paresis of facial muscles is possible.
Ganglioneuritis of the stellate ganglion
The clinical picture is characterized by the presence of pain in half of the chest on the side of the inflamed node. Sensitivity and motor reflex disturbances are observed in the fingers. The impairment of motor skills is especially noticeable in the fifth finger of the hand located in the affected area. The area of pain, loss or impairment of sensitivity has a so-called “half-jacket” appearance. Often the pain spreads to the chest area, therefore it resembles angina attacks and must be differentiated from coronary heart disease.
How is the diagnosis done?
In order to detect the presence of such an inflammatory process in the patient’s body, doctors rely only on indications obtained from the clinical picture. They are noticeable during a standard examination of the patient for vasomotor and neurotrophic problems identified when testing the neurological status of sensory reflexes.
Typically, people suffering from thoracic and sacral types of illness undergo a long course of therapeutic measures. The treating expert prescribes that they undergo consultation with their colleagues in the field of cardiology (due to the manifestation of cardialgia), gynecology (for pain in the pelvic area) and gastroenterology (for malfunctions of the secretory and motor options of the gastrointestinal tract). For other characteristic symptoms, you need the help of a neurologist. The most popular clinical procedures for studying the body:
Computer testing.- Magnetic resonance scanning.
- Electromyographic examination.
- MSCT.
- Ultrasound examination of the abdominal cavity and gynecological department.
Diagnosis of ganglioneuritis
Diagnosis of ganglioneuritis is a complex process, since the symptoms of the clinical picture are similar to a number of other diseases (otitis media, coronary heart disease, oncological formations, spinal formations, circulatory disorders, various types of neurosis, etc.). The difficulty also lies in determining the variation of ganglioneuritis, since the symptoms of its various types are very similar. Untimely or incorrect diagnosis can significantly worsen the patient’s condition, slow down the treatment process and, accordingly, lead to disappointing prognoses.
If at least some of the above symptoms appear, you should consult a neurologist. The initial diagnosis of ganglioneuritis usually occurs on the basis of an analysis of the clinical picture from the patient’s words and examination of the patient, identifying signs of vasomotor and neurotrophic disorders, and sensitivity disorders.
Diagnostics
Since the picture of the disease is clearly expressed, the disease can be identified based on:
- medical history studies;
- patient interview;
- examination with palpation of the diseased area;
- studying the skin and mucous membranes;
- heart rate and temperature measurements.
To clarify the diagnosis, radiography, ultrasonography, blood tests, and consultation with specialized specialists are prescribed.
Hardware diagnostics of ganglioneuritis
Thoracic and sacral ganglioneuritis are especially difficult to differentiate, and for the accuracy of the diagnosis, the patient undergoes a long examination for the presence of somatic diseases. For this purpose, consultations with a gynecologist, cardiologist, gastroenterologist, and phthisiatrician are prescribed. In order to exclude a number of diseases, radiography of the spine, electromyography, MRI and CT may be prescribed.
The inflammatory process often causes changes in somatic organs, so the patient undergoes MSCT or ultrasound of the abdominal organs, genital organs, and prostate in order to identify these pathologies.
Treatment
Treatment of ganglionitis depends on its etiology. Typically, in the case of inflammatory processes, doctors prescribe desensitizing agents, antiviral and immunomodulatory agents to the patient.
Complex therapy consists of drugs that can reduce the excitability of vegetative formations. These include B vitamins, ganglion blockers (the most effective are ganglerone and pachycarpine). Treatment of neuropathic pain is carried out with special drugs - anticonvulsants and antidepressants. Treatment with drugs is usually long-term; if necessary, it is supplemented with metabolic and vascular agents.
Novocaine blockade of the affected node is also carried out. Sometimes physiotherapy, which includes ultrasound therapy, Bernard currents, salt, radon and hydrogen sulfide baths, therapeutic mud, etc., is also effective for ganglionitis.