Intercostal neuralgia is a disease in which irritation or compression of the intercostal nerves occurs. This can happen for various reasons. The disease is relatively rare, its main manifestation is pain along the affected nerve.
Our expert in this field:
Lashch Natalia Yurievna
Neurologist of the highest category, candidate of medical sciences, associate professor. Laureate of the Moscow City Prize in the field of medicine.
Call the doctor Reviews about the doctor
How are intercostal nerves arranged? What functions do they perform?
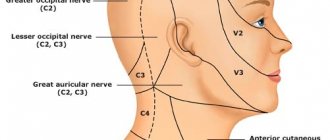
Two nerve roots emerge from the spinal cord: the anterior one is formed by the processes of motor nerve cells, the posterior one - by sensory ones. Then, while still inside the spinal canal of the spine, these roots are connected to form the spinal ganglion. Two spinal nerves depart from it: anterior and posterior.
In the thoracic spinal cord, the anterior branches of the spinal nerves pass into the intercostal nerves. They pass in the spaces between the ribs - each of them is located along the lower edge of the corresponding rib - and, unlike the anterior spinal roots, are mixed, that is, they are responsible for both movement and sensitivity:
- provide movement of the chest muscles involved in the breathing process;
- provide sensitivity to the skin of the chest and upper abdomen.
Treatment of back neuralgia
Did you know that...
Next fact
Typically, neuralgia of any type responds well to treatment in the early stages . A timely visit to a specialist will help to avoid complications, so do not put off talking with a doctor for too long. There are a huge number of methods to combat this disease, so the doctor will be able to choose exactly the course that is suitable in your case.
Drug treatment
Treatment of any disease, including neuralgia, is largely determined by the individual situation of the patient, so there is no universal set of drugs. For each stage and degree of neglect of neuralgia, special therapy is selected.
The following medications may be prescribed during treatment::
| Anti-inflammatory drugs |
|
| Antiepileptic drugs |
|
| Vitamins B |
|
| Antihistamines |
|
| Muscle relaxants | — |
| Anti-inflammatory ointments |
|
| Anticonvulsants |
|
| Novocaine blockades of various kinds | — |
Important! Each of the drugs listed here has an extensive list of side effects and contraindications; using them without medical supervision is strictly prohibited.
Exercises, massage, exercise therapy for back neuralgia
For neuralgia of the back, various types of therapeutic physical exercises, massage, manual therapy and even acupuncture are used with great success..
All of these treatments must be prescribed by your doctor. Only a specialist will be able to prescribe you the correct therapeutic course, which includes sessions of physical education, therapeutic massage and manual treatment. It is prohibited to exercise or massage on your own, as you can aggravate your condition, which will lead to irreversible consequences.
Traditional methods of treatment
In addition to traditional therapeutic methods, there are a number of folk recipes that can help you relieve acute pain and cope with attacks of neuralgia.
Important! Alternative treatment should in no case be taken as a basis in this case, since, despite all its harmlessness, neuralgia can be very dangerous in advanced cases. Recipes can only be used as a supplement or first aid.
Here are a few alternative medicine recipes that can help cope with a pain attack:
- Prepare a healing ointment from Vaseline and lilac buds. Make a thick decoction of lilac buds and mix it with Vaseline in a ratio of 1 to 3. This ointment relieves pain and fever;
- Apply a compress of potatoes, honey and horseradish to the sore nerve. This lotion will warm up the muscle well and reduce pain;
- Drink lemon balm and mint tea. This tea will help you relax and relieve muscle tension, and therefore inflammation;
- You can also try taking a bath with pine cone extract to relax;
- If you notice severe swelling, we advise you to apply a salt compress to it;
- In order to improve blood circulation in the inflamed area, apply a compress of beetroot or horseradish juice;
- A compress made from ordinary burdock turns out to be quite effective. Simply tie a fresh, clean burdock leaf to the sore area;
- Ointments using beeswax and propolis are also effective. But here you need to be careful. An allergic reaction is possible.
Once you have used one or more of the recipes, wrap the affected area as warmly as possible. At the same time, you should not allow strong drafts in the apartment or strain the inflamed muscle.
Disease prevention
As with any other disease associated with pain in the joints and muscles, there are a number of preventive measures that can help avoid the appearance of neuralgia :
Pay attention to the rules for preventing back neuralgia. Try to avoid severe stress, as well as drafts and severe hypothermia;- Watch your diet, enrich it with vitamins, minerals, refrain from too spicy, salty and fatty foods, as well as alcohol;
- Strengthen your immune system. Walk in the fresh air as often as possible, move, watch your posture;
- Don't start spinal diseases. If you notice any symptoms that may indicate impending problems, it is better to immediately contact a specialist and not create additional problems for yourself.
Treatment of intercostal neuralgia
How to treat intercostal neuralgia? Therapy is carried out in two directions:
- It is necessary to alleviate the main symptom of the disease - chest pain.
- At the same time, it is necessary to identify the cause - the disease that led to compression or irritation of the nerve - and treat it.
In the acute stage of the disease, the doctor prescribes bed rest and recommends sleeping on a flat and firm bed. To combat pain, non-steroidal anti-inflammatory drugs are used, and various ointments help. In case of severe pain, a novocaine blockade is performed: the place where the affected nerve is located is injected with an anesthetic solution. There are also special patches with anesthetics.
Vitamins are prescribed to improve the condition of nervous tissue, muscle relaxants to relieve muscle spasms. Prolonged pain leads to a person becoming overly excitable and nervous, in which case sedatives are prescribed. Physiotherapy procedures help: Sollux, electrophoresis, UHF. A neurologist can prescribe massage and acupuncture sessions.
Is it possible to cope with the disease on your own? Over-the-counter pain medications and folk remedies can help relieve pain for a while. But in order to prescribe truly effective treatment for intercostal neuralgia on the right or left, you need to understand what causes it. Improper self-medication can be harmful.
We will call you back
Message sent!
expect a call, we will contact you shortly
The main symptom of intercostal neuralgia is pain. It spreads along the rib, as if encircling the right or left half of the chest, and can be sharp, stabbing, burning, or dull, aching. The pain intensifies during inhalation, because of this the person cannot breathe deeply. Movements, changes in body position, coughing, and sneezing also lead to aggravation.
Painful sensations occur if you press on certain points between two adjacent ribs along their course. This symptom is checked by a neurologist during an examination.
Other possible symptoms of intercostal neuralgia on the right and left (as well as pain, occur in the area of the affected nerve):
- twitching of the chest muscles;
- increased sweating;
- redness or paleness of the skin;
- numbness.
With intercostal neuralgia on the left, a person may complain that his heart and stomach hurt. Pain may radiate under the shoulder blade, to the collarbone area.
Similar chest pains can occur with diseases of the heart, lungs, pleura, and spine. An incorrect diagnosis and lost time can lead to serious consequences.
Intercostal neuralgia in women & Intercostal neuralgia in men.
Intercostal neuralgia in men occurs as often as in women, but at the same time, intercostal neuralgia in women has its own characteristics. For example, women often perceive pain due to intercostal neuralgia as a manifestation of breast disease, and not as neuralgia. And it is clear that such thoughts can only cause additional anxiety and worry. But there is one consolation - although pathology of the mammary glands is indeed common, even if it is present, the vast majority of pain is not associated with it, but with the spine, nerves and muscles. This does not cancel periodic examinations with a mammologist, but it does mean that you should never panic. And most importantly, keep in mind that in medicine there is such a concept - a disease “in disguise”, when one disease is masked by another. Let's look at the insidiousness of this problem using our example. Pathology of the mammary glands is a psychological dominant that causes much more concern than intercostal neuralgia. Accordingly, if a woman simultaneously has thoracic intercostal neuralgia and pathology of the mammary glands, then all her thoughts will be focused on the glands. The rest will fade into the background. And it is quite natural that in this situation a woman, first of all, will turn to a mammologist. If the mammologist turns out to be knowledgeable, he will quickly figure out what is causing the pain: glands or neuralgia. And, if it is neuralgia, he will refer the patient to a chiropractor. By the way, it is the chiropractor who is the main doctor for intercostal neuralgia (but we’ll talk about this later). And if a mammologist comes across an inexperienced or over-insurer, what will he do? Most likely, having discovered his own profile pathology in the patient, he will also focus on this pathology and will not “dig” deeper. Consequently, if in reality the patient was bothered by pain due to intercostal neuralgia, and the pathology of the mammary glands was only a background that did not cause pain, then treatment by a mammologist will not solve the problem. The pain will remain. And this will cause the woman even more anxiety. Her faith in doctors will suffer. Your nerves and time will be wasted. This is what the disease turns out to be “under the mask.” Meanwhile, intercostal neuralgia in women very often occurs under the guise of mammary gland pathology. Be sure to remember this!
Dear women, the best advice for pain in this area is to contact two specialists at once. A mammologist will give you confidence and relieve fears, and a chiropractor will cure intercostal neuralgia. After all, as we have already said, a chiropractor is the key doctor for intercostal neuralgia. This approach is the most reasonable. It will save you both time and nerves.
Intercostal neuralgia in men also has its own characteristics, and these are not always differences. For example, very similar psychological aspects. So, if in women intercostal neuralgia often occurs under the guise of mammary gland pathology, then in men it occurs under the guise of heart disease. By the way, it is precisely the “disguise” as heart disease that distinguishes left intercostal neuralgia from intercostal neuralgia on the right side. Do you know how to distinguish intercostal neuralgia from a heart attack at home? Very simple. Heart pain is relieved by nitroglycerin, but neuralgia is not.
According to statistics, intercostal neuralgia on the left in the heart area equally often causes a false alarm in both men and women. Moreover, in women, both the heart and the mammary gland come under suspicion. But, right intercostal neuralgia is “suspicious” only for women. Men immediately understand that this is intercostal neuralgia.
How to distinguish the signs of intercostal neuralgia from the symptoms of other diseases?
It is especially important to distinguish in time between irritation of the intercostal nerves and angina pectoris, a condition in which the heart muscle does not receive enough oxygen-rich blood. Main differences:
- With intercostal neuralgia, pain persists for a long time. With angina pectoris, they last about 5 minutes and go away if you take nitroglycerin.
- With neuralgia, pain intensifies during deep inspiration, movements, sneezing and coughing, but with angina pectoris this does not happen.
Other dangerous conditions that need to be distinguished from intercostal neuralgia are myocardial infarction and PE ( pulmonary embolism) . Typically, a heart attack occurs after physical exertion or after a person becomes very nervous. The pain is accompanied by signs of dysfunction of the cardiovascular system:
- The man turns pale. Fingertips, nose, lips may become bluish.
- Sticky cold sweat appears.
- Shortness of breath that persists even when the person is resting - lying or sitting.
- Blood pressure drops.
- The fear of death arises.
You should not engage in self-diagnosis - erroneous conclusions are fraught with serious consequences. See your doctor. Get examined at the clinic. In any case where there is a suspicion of a heart attack, it is better to play it safe and immediately call an ambulance.
What to do for back pain of various types
Back pain can be different: acute, radiating to different parts of the body, deep, aching, very strong, constant or wave-like. It can also be located on different parts of the back: in the neck, chest, lower back, sacrum and coccyx. Even after a complete examination, it is not always possible to find out the cause of back pain, and then they say that it is nonspecific.
Such pain is called noceceptive, associated with irritation of pain receptors in tissues (muscles, ligaments, bones). Irritants can be mechanical (injury), physical, chemical and inflammatory in nature. Moreover, the degree of changes in the spine does not always correspond to the intensity of pain. Nonspecific pain accounts for about 80% of all back pain syndromes.
Neuropathic pain syndrome is associated with damage to nerve roots and nerve trunks. These pains account for 7–8% of all pain syndromes; their feature is the high possibility of confirming the diagnosis during instrumental studies.
The third type of pain - specific pain syndromes (for example, with spinal tuberculosis) are relatively rare.
Severe back pain due to coronavirus and other acute respiratory viral infections
With any acute respiratory viral infection, accompanied by a sudden onset and fever, muscle pain in the back, aches throughout the body and severe weakness may appear. These painful sensations are associated with general intoxication of the body. During a coronavirus infection with a high temperature, back pain may be one of the first manifestations.
When coronavirus pneumonia appears, pain in the back increases due to damage to the pleura, which has many nerve endings, as well as due to constant tension of the spinal muscles during obsessive coughing. A large amount of lactic acid accumulates in the back muscles, causing irritation and pain.
What will help: you can take Paracetamol orally - it is an analgesic and antipyretic. Taking any NSAIDs orally and applying them to the skin in the form of ointments and gels will also help.
Severe pain in the upper back (cervical spine)
Acute pain syndrome can be of a mixed nonspecific and neuropathic nature. Nonspecific aching pains are often associated with an incorrect forced position at the table during work, tension in the muscles of the back and neck. A short-term painful attack can appear with angina and radiate to the left arm.
Neuropathic pain has an acute, burning nature, radiates to the arm and shoulder blade on the affected side and is associated with pinched nerve roots of the cervical spine.
How can I help you:
- for pain due to spinal diseases - NSAIDs;
- heart attack - Nitroglycerin tablet under the tongue; if the pain does not go away within a minute, take another tablet and call an ambulance.
Severe pain in the chest and shoulder blades
The back in the thoracic region and between the shoulder blades most often hurts due to a sedentary lifestyle and the body being in an uncomfortable position for a long time. Very often, this condition appears in those who sit at the computer for several hours a day. Weakened muscles cannot withstand the load and hurt.
The development of a child can be impaired due to incorrect posture - a lateral curvature of the thoracic spine occurs - scoliosis. If measures are not taken in time, the vertebrae become displaced and a compression fracture may occur.
Severe pain between the shoulder blades can occur when the roots of the spinal nerves of the thoracic spine are pinched. It can radiate into the intercostal spaces or into the left arm and resemble an attack of angina, but it is not relieved by Nitroglycerin.
Acute pain in the area of the shoulder blades can appear due to various diseases of the internal organs: heart, stomach, pancreas, lungs (with damage to the pleura), kidneys, gall bladder.
How can I help you:
- in case of damage to the musculoskeletal system - NSAIDs (see section “How to alleviate your condition yourself”);
- for spasm of the arteries supplying the heart muscle (angina attack) - a Nitroglycerin tablet under the tongue;
- for diseases of internal organs - only a doctor can decide; in some cases, taking painkillers can lead to serious complications, for example, with appendicitis or cholecystitis, pain that indicates the need for surgery can be removed.
If you don’t understand what hurts, it’s better to call an ambulance.
My lower back hurts a lot
Acute lumbar pain syndrome is most often associated with the condition of the spine, is nonspecific in nature and accounts for about 80% of all pain in this area.
Neuropathic pain syndrome accounts for about 7 – 8%. Thus, acute sudden pain in the lower back (lumbago) is usually associated with pinching of the spinal roots in the lumbar spine. Acute sudden pain in the buttock, radiating to the back of the thigh (sciatica) is pinched or inflammation of the sciatic nerve.
The lower back can also hurt with diseases of the kidneys, urinary tract, and genital organs.
How can I help you:
- for myositis - NSAIDs;
- for neuropathy - NSAIDs do not always relieve pain, you need to consult a doctor to prescribe a full course;
- for diseases of internal organs - depends on the diagnosis, which can only be established by a doctor.
Severe back and stomach pain
Such pains are dangerous, most often they are associated with diseases of the internal organs. When they appear, they first think about acute pancreatitis. Acute pain syndrome is girdling in nature, accompanied by nausea, vomiting and requires emergency hospitalization of the patient. If this is not done, necrosis of the pancreatic tissue may occur and the patient will die.
Less commonly, girdle pain occurs with kidney disease. This condition also requires medical attention. With cholecystitis and an attack of cholelithiasis, pain may occur on the right side, radiating upward to the collarbone.
Acute girdle pain can occur with intercostal neuralgia caused by pinching of the spinal roots of the lower parts of the thoracic spine. The pain is so severe that it deprives the patient of sleep.
How can I help you:
- for intercostal neuralgia - NSAIDs;
- for diseases of internal organs - immediately call an ambulance; Before the doctor arrives, you can take 2 tablets of No-shpa.
Severe back pain that radiates to the leg
Irradiation of acute pain in the buttock and the back surface of the right or left leg to the knee indicates infringement of the nerve roots of the lumbar region with the involvement of the sciatic nerve in the process. The pain syndrome is especially strong, has the character of an electrical discharge and is accompanied by painful convulsive twitching.
How can I help you:
- Call an ambulance as soon as possible, and before that take NSAIDs and apply anesthetic ointment, but this is not very effective.
My back hurts when I inhale too much
Painful breathing most often occurs:
- with intercostal neuralgia - pain intensifies from any movement, including inhalation and coughing;
- for acute diseases of the lungs and bronchi involving the pleura - pleuropneumonia, lung cancer.
How can I help you:
- call a doctor to your home and sort out the problem; It is impossible to do this on your own.
My back hurts a lot under my ribs
This localization is often associated with diseases of internal organs:
- sharp, strong pain that does not subside and cannot be relieved, radiating to the stomach and spreading to the opposite side of the back; accompanied by nausea and vomiting – in acute pancreatitis;
- acute paroxysmal pain, often radiating to the groin area - with urolithiasis during the passage of a stone through the urinary tract.
How can I help you:
- call an ambulance - this is an emergency situation that often requires hospitalization; No-spa can reduce the pain a little.
Back side pain
Acute pain on the sides of the back can also be associated with diseases of the musculoskeletal system and internal organs. Based on the location and nature of the pain, one can assume its origin. If there is pain in the right side:
- Location in the right middle back:
- acute pain radiating along the intercostal nerves - it can be assumed that the nerve roots of the thoracic spine are pinched;
- aching local – muscle inflammation;
- deep, aggravated by deep inspiration and coughing - often associated with diseases of the pleura - pleurisy, lung cancer with germination into the pleura.
- Localization on the right side under the ribs:
- intercostal neuralgia due to infringement of the right nerve root;
- diseases of the pancreas, liver and biliary tract.
- Pain in the left side:
- Severe burning pain along the ribs at any level is neurogenic pain associated with spinal pathology.
- Acute, sudden, short-term pain in the upper and middle back, often radiating to the left arm - an attack of angina.
How can I help you:
- for spinal diseases - NSAIDs;
- for angina pectoris - Nitroglycerin under the tongue;
- for attacks of pancreatitis, cholecystitis, urolithiasis - take 2 tablets of No-shpa.
If the pain does not go away, you need to call an ambulance.
Back muscles hurt a lot
Back muscle pain appears with a cold, acute respiratory viral infections, or after a long workout. In people who lead a sedentary lifestyle, muscles may ache even with little physical activity.
Any disease of the spine (osteochondrosis, disc herniation, scoliosis, etc.) is always accompanied by tension in the back muscles, as they protect the spinal column from any negative influences. At the same time, tension in the muscles increases pain in the back.
How can I help you:
- contact a neurologist, undergo an examination and find out the cause of the pain; You can relieve severe pain on your own using an ointment or gel with NSAIDs, but it will be difficult to completely get rid of pain.
Back pain severely at night and in the morning
Night and morning back pain is a serious symptom, one of the signs of the inflammatory process. As a rule, pain is combined with other symptoms: age up to 40 years, gradual onset, morning stiffness of movements for up to half an hour or more, elimination of pain after the start of physical activity.
This is a serious symptom that deprives patients of sleep and develops in diseases such as ankylosing spondylitis (ankylosing spondylitis), reactive arthritis, psoriatic arthritis, juvenile chronic arthritis, arthritis associated with chronic inflammatory bowel diseases.
How can I help you:
- nothing on your own, you need to contact a rheumatologist, conduct an examination and treat the identified pathology.
Severe back pain during pregnancy
Pain syndrome during pregnancy is mechanical in nature. A growing fetus increases the load on the muscles and ligaments of the back. In the back muscles, with constant tension, an increased amount of lactic acid is produced, which leads to the appearance of aching muscle pain.
The pain syndrome can also have an acute, paroxysmal nature, which indicates infringement of the spinal roots against the background of a high load on the spine. A pregnant woman experiences severe pain, is deprived of sleep and is constantly in a state of stress.
How can I help you:
- contact a neurologist or a antenatal clinic therapist, he will conduct an examination and prescribe the necessary treatment; You cannot take medications on your own: many NSAIDs are contraindicated during pregnancy;
- Wearing a bandage to support the abdomen is indicated.
Treatment of symptoms of intercostal neuralgia on the right and left
The leading symptom of the disease – pain – is helped by painkillers (non-steroidal anti-inflammatory drugs), anesthetic patches, novocaine blockades, and physiotherapy.
But coping with the symptoms does not mean curing the disease. Therefore, treatment should also be aimed at the cause. A thorough diagnosis must first be carried out - this is only possible in a clinical setting.
Take care of yourself, book a consultation now
Message sent!
expect a call, we will contact you shortly
“Intercostal neuralgia” is not one specific diagnosis, but a collective term. It refers to different conditions that lead to damage to the intercostal nerves and, as a result, to chest pain.
Why is it important to understand the cause of this condition in each specific case? This will allow you to prescribe effective treatment that will help you recover or keep your chronic disease under control.
What is neuralgia?
Muscular neuralgia is a condition in which peripheral nerves are affected. Inflamed tissue in the interosseous spaces begins to compress the nerve, causing the person to feel severe pain. Very often, neuralgia is localized between the ribs on the back or in the lumbar region (neuralgia of the back).
Classification of the disease
Neuralgia (as a general disease) has several types. In modern medicine, it is divided into primary (also called typical, idiopathic and essential) and secondary (also called symptomatic).
In addition to division by origin, there is a classification in terms of localization of muscle spasm.
In this case, neuralgia is divided into :
- trigeminal neuralgia;
- occipital (and facial) neuralgia;
- intercostal neuralgia (one of the most common);
- neuralgia of the external cutaneous nerve of the thigh.
There are different types of neuralgia, depending on which nerve was damaged
Clinical picture of neuralgia of the back
Pain in the back muscles is the most common in patients. This disease affects people with low immunity. It was once believed that neuralgia was the lot of older people, but in the modern world there is a sharp “rejuvenation” of this disease .
Symptoms almost always appear in acute form , so it is simply impossible not to notice them. The back begins to hurt, and the pain is quite sharp, acute, burning. Symptoms often begin to appear after a person has experienced stress.
Painful sensations occur in paroxysms, as if you were “shocked by an electric shock . Typical pain sensations may become stronger or disappear abruptly, while atypical pain sensations are constant and affect large areas of nerves.
Since neuralgia damages the nerve ending, the pain is similar to an electric shock
Typically, neuralgia of the back begins with a slight muscle spasm. For example, during heavy physical activity or sudden movements. Also, very often a spasm occurs during awakening from sleep (when sleep took place in an uncomfortable position).
In addition to these reasons, you can also name drafts (the nerve can get cold), sneezing or a strong cough, or a very deep breath.
An attack of neuralgic disease is accompanied by high sweating, muscle tremors and anemia (hyperemia) of the skin.
Prevalence and significance of the disease
Neuralgia in various forms (including neuralgia of the back) is a very common disease . It affects both middle-aged and elderly people, as well as young people, and even children. There can be many reasons for the appearance of severe muscle pain, ranging from a sedentary lifestyle to a decrease in immunity.
Despite the prevalence of the disease, it is difficult to treat in advanced cases, so at the first symptoms it is better to consult a specialist and start treatment. This way you can prevent sudden sharp pain and cope with the problem with a minimum of discomfort.
Video: “How to recognize neuralgia?”
The main causes of intercostal neuralgia
Most often, the following reasons lead to compression and irritation of the intercostal nerves:
- Osteochondrosis. A degenerative disease that primarily affects the intervertebral discs. Their height decreases - the distance between adjacent vertebrae decreases, this leads to compression of the nerve roots.
- Hypothermia, exposure to drafts.
- Intense physical activity, sudden awkward movements.
- Working in an awkward position when your back is constantly under tension.
- Injuries to the chest and thoracic spine, previous surgeries.
- Frequent and severe stress.
- Viral infections. The most common cause is a cold, shingles.
- Chronic spasm of the back muscles. It promotes irritation of nerve receptors.
Most often, intercostal neuralgia occurs in older people, when the causes of the disease are layered with age-related changes in the spine and blood vessels.
Causes of intercostal neuralgia and risk factors
Intercostal neuralgia can develop for a variety of reasons. Among them are:
- injuries to the thoracic nerves, chest and spine;
- surgical interventions, long-term immobilization of a person in a certain position;
- poisoning with chemicals, prolonged use of medications;
- congenital developmental anomalies, hereditary diseases;
- infectious processes (shingles, tuberculosis, brucellosis and others);
- some neurological diseases, such as radiculitis and multiple sclerosis;
- diseases of the spine (osteochondrosis, deforming spondylosis, herniated intervertebral discs);
- compression of nerve branches in the bone-connective sheaths, for example, in the presence of scar changes, benign or malignant neoplasms;
- immunodeficiency (HIV infection, cancer, etc.);
- allergic reactions;
- diabetes;
- various metabolic disorders in nervous tissue and its hypoxia;
- lack of B vitamins in the body;
- alcohol abuse;
- osteoporosis;
- pathology of nearby anatomical structures (aorta, lungs, pleura);
- various systemic diseases (atherosclerosis, rheumatism, anemia, thyrotoxicosis, etc.).
More often, chest neuralgia appears due to several causes. Therefore, it is typical for older patients with vascular, degenerative and metabolic disorders. Sometimes symptoms of neuralgia appear after excessive physical activity, sudden movements or prolonged stay in one position. They can also occur after hypothermia or severe stress.
More often, intercostal neuralgia is observed on the left or right; less often, there is a bilateral lesion. In most cases, the pathogenesis is based on muscle spasm, leading to compression of nerve fibers. Pain occurs in response to nerve damage.
In children, signs of intercostal neuralgia are rare. When they appear, parents should definitely show the child to the doctor, as this may be a signal of the presence of a serious pathology. The doctor will determine the possible causes and explain how to cure intercostal neuralgia in this case.
What other diseases lead to girdle pain in the chest?
Often people tend to dub “neuralgia” any girdle pain along the ribs. But this symptom may have other causes, including:
- Spondylosis is an inflammatory disease that causes damage to the vertebral bodies and deformation of the spinal column.
- Hormonal spondylopathy is a pathology that develops in older people, for example, in women after menopause. The spine is deformed, and disorders occur in the vessels that supply it.
- Malignant tumors - those that arise in the spine itself or metastases from other parts of the body.
- Ankylosing spondylitis is a chronic inflammatory process that leads to decreased mobility in the spinal column.
- Gastritis and other diseases of internal organs.
How does the treatment of intercostal neuralgia depend on the cause?
With intercostal neuralgia, it is not enough to eliminate the main symptom of the disease - pain. You should always look for and treat the underlying cause. The doctor prescribes therapy individually, depending on the pathological changes detected during examination and examination, and the final diagnosis.
Make an appointment at the Medica24 International Clinic - get a consultation with an experienced neurologist and undergo an examination using our modern equipment. This will help to quickly and accurately establish a diagnosis and prescribe the correct treatment in a timely manner.
Get a consultation with a doctor
Message sent!
expect a call, we will contact you shortly
The main manifestation of intercostal neuralgia – chest pain – can also occur with many other diseases. And figuring out the correct diagnosis is not always easy.
The diagnostic process begins with a visit to a neurologist. The doctor will ask you some questions:
- When did you first experience pain? How did this happen? What preceded this?
- What is the nature of the pain, when does it usually occur, how often, how long does it last?
- Do you have chronic lung or heart diseases? Are you monitoring your blood pressure?
- What infections have you had? Have you had any chest injuries or surgery?
- What other symptoms bother you?
You may be asked to complete a special “pain questionnaire”. The doctor will perform a complete neurological examination to rule out other neurological diseases. You will then be given an examination.
To understand the causes of irritation or compression of the intercostal nerve, the doctor may prescribe x-rays, CT, MRI, and, if necessary, other studies.
Symptoms of intercostal neuralgia
It is believed that the main symptom of intercostal neuralgia is pain in the intercostal space. But how can one distinguish intercostal neuralgia from one symptom, even such a striking one? After all, pain in the ribs also occurs with other pathologies. Obviously, for an accurate diagnosis, more signs of intercostal neuralgia are needed. Therefore, we decided to talk about the symptoms and causes of intercostal neuralgia in more detail.
The name intercostal nerves speaks for itself. They are actually located between the ribs. Starting from the spine, they cover the chest on both sides. The intercostal nerve cannot suffer from a small or even moderate bruise, since it is located deep under the rib. Therefore, the mechanical cause of intercostal neuralgia can be serious injuries, for example, a fracture; a tumor compressing a nerve, or dystrophic pathology of the spine - osteochondrosis, hernia and disc protrusion.
In addition to mechanical ones, there are also infectious causes of intercostal neuralgia, most often a herpetic infection. Due to its characteristics, it often affects these nerves. Herpes, as a sign of intercostal neuralgia, is easily recognized by characteristic rashes that coincide with the area of pain.
Thus, the causes of intercostal neuralgia are infectious and mechanical. But, the connection between intercostal neuralgia and breathing is a myth. Remember, at the beginning of the article we talked about the difference between real intercostal neuralgia and what many people mistakenly consider to be such. For example, the appearance of intercostal neuralgia after a cold is not neuralgia at all, but myofascial syndrome. If you are not aware, myofascial syndrome is a muscle disease in which small painful areas - trigger points - form in the muscles. These points may remain in a latent state for a long time and not manifest themselves in any way. But as soon as they are activated, pain immediately arises. The most common factor in the activation of trigger points is overload of the affected muscles. The intercostal muscles are classified as respiratory muscles, as they are involved in the act of breathing. A cough is a forced exhalation. Therefore, intercostal neuralgia when coughing or after a cold is not neuralgia, as many people mistakenly think, but myofascial syndrome, provoked by overload of the respiratory muscles from coughing. By the way, an indirect sign of how to distinguish intercostal neuralgia from myofascial syndrome is the duration of the disease. True intercostal neuralgia takes a long time to heal. Especially if it is caused by a fracture or tumor. And myofascial syndrome has a shorter treatment period. But it is impossible to say exactly how long intercostal neuralgia lasts without seeing the patient. Firstly, you need to make sure that it is intercostal neuralgia and not some other pathology, and secondly, it all depends on the situation. Agree, neuralgia from herpes and from a fracture will have completely different treatment periods.
Separately, it is necessary to say about the so-called false symptoms of intercostal neuralgia. Muscle tension, muscle twitching, increased pain when coughing, sneezing, turning the body; forced body position to relieve pain, sweating, high blood pressure and a number of other symptoms are not signs of intercostal neuralgia, although they are often attributed to it. These symptoms refer to pathologies similar to neuralgia. Being able to distinguish between similar pathologies is one of the basic skills of a doctor, which is specially taught, and which allows the doctor to make an accurate and correct diagnosis. It remains only to remind you that a doctor for intercostal neuralgia is a chiropractor, or even better, a chiropractor-neurologist.
Instrumental methods for diagnosing intercostal neuralgia
At the Medica24 International Clinic, you can undergo examination using our own diagnostic equipment, which meets the most modern standards. It will help diagnose the disease at an early stage and take timely measures.
First of all, it is important to carry out a differential diagnosis of intercostal neuralgia with certain diseases of the spine, cardiovascular system, and lungs. To do this, if necessary, the neurologist will refer you for a consultation with a cardiologist or pulmonologist.
You may be prescribed an ECG, Holter monitoring, cardiac ultrasound, X-ray, CT and MRI of the chest, biochemical blood test, and bacteriological studies.
Consequences
If you have decided that going to the doctor and taking care of your own health is not your thing, then you should find out what awaits you in the event of an advanced case of the disease.
Since neuralgia most often affects the extensor muscles of the spinal region , as well as the muscles located near the shoulder blades and shoulders, therefore, it will spread with great speed throughout the entire lumbar-thoracic region of the back.
The acute pain that arises will intensify, the attacks will begin to radiate from the lumbar region to the thoracic region, and will become stronger when making the slightest movements of the spine and chest. As a result, weakness of the abdominal muscles, respiratory apparatus, and human stiffness will occur.
There is also a high risk of inflammatory processes in the intervertebral tissues . This is where herpes, shingles and other infectious diseases often begin to appear, characterized by the appearance of painful blisters with fluid on the body.
The body temperature will begin to rise, and the biochemical composition of the blood will change. The disease will go away, but then return with a hundredfold complication and worsening of the condition.
If neuralgia is completely neglected, the risk of developing neuritis will increase, which will serve as an impetus for atrophy of the musculoskeletal system and paralysis.