Our clinic is engaged in examination, treatment and rehabilitation measures for pinched, inflammation and injuries of the nerves of the legs (sciatic, tibial, peroneal and their branches). You will need to be examined by a neurologist. if any studies have been previously performed, be sure to take their results for consultation, incl. the x-rays themselves . If the studies have not been performed, we will do everything necessary in our clinic or with our colleagues in other clinics.
- What are the causes of damage to the tibial and peroneal nerves?
- Symptoms of Tibial and Peroneal Nerve Suffering
- Diagnosis of neuropathies of the tibial and peroneal nerves
- Treatment of damage to the tibial and peroneal nerves at the Echinacea clinic
- When is surgery necessary?
How the treatment will be structured:
- Let's establish the location and cause of nerve damage. We perform electromyography of the peroneal, tibial and other leg nerves and ultrasound of the nerves. The potential benefit of non-surgical treatment or strict indications for surgery (risk of complete nerve loss) can be determined using needle myography.
- We will find out and discuss with you the possibility of non-surgical treatment and the prospects for restoring nerve function. Medicines can be used here, incl. administration of anti-inflammatory and absorbable drugs directly to the point of compression or damage to the nerve. For the rehabilitation treatment of the sciatic, tibial and peroneal nerves, magnetic stimulation of the nerves of the legs is very effective: improvement is noticeable immediately or several days after the procedure.
- If the chances of restoring the peroneal or tibial nerve without surgery are low, we recommend surgical treatment . We perform most of the operations on an outpatient basis. You will be able to go home on the day of surgery. The budget for surgery without hospitalization is significantly less. If hospitalization is required, we will refer you to a trusted specialist. After surgical treatment, we will offer a course of rehabilitation treatment.
What are the causes of damage to the tibial and peroneal nerves?
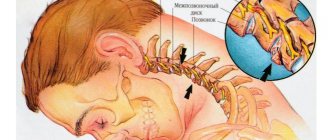
The tibial and peroneal nerves pass through narrow canals formed by bones, ligaments, tendons and muscles. Nerve tissue is very delicate and vulnerable. Often we detect nerve suffering even with slight narrowing or deformation of the nerve canal. Narrowing or deformation of the tibial and peroneal nerve canals occurs:
- In case of injury (bone fracture, bruise, hemorrhage, sprain or wound); Often, when injured, the nerve is pulled into scarred tissue or compressed by a bone fragment; nerve injury can also be represented by a nerve bruise, partial or complete interruption.
- If there is compression in an uncomfortable position (a tucked or compressed leg while wearing uncomfortable shoes, position, unconsciousness or intoxication, under anesthesia);
- With thickening and deformation of the knee and ankle joints and ligaments , with chronic injury and overload of the joints, often associated with the type of activity (sports, walking, forced posture, vibration, weight). Very often, such changes are facilitated by diseases and deformities of the spine. These types of neuropathy are called tunnel syndromes of the ulnar, radial and median nerves;
- For foot deformities due to flat feet (tarsal tunnel syndrome, meralgia) .
The function of nerves is to conduct electrical impulses from the brain to muscles and organs, and to the brain from sensory receptors in the body. Any damage to the nerve leads to disruption of the conduction of excitation along the nerve, which means disconnection of the affected part of the body from the brain.
Therefore, if the tibial and peroneal nerves suffer, the following are possible:
- Decreased strength and weight loss of leg muscles, twisting of the foot when walking and even fractures;
- Decreased sensitivity (numbness)
- Pain along the nerve or in the foot, fingers.
Symptoms of the disease
Pathology can manifest itself in different ways; if the pathology is acute, then the symptoms appear sharply, but if the disease is chronic, the clinic progresses. In general, the development of the disease may be indicated by:
- disorder of extension of the foot and fingers;
- man walking. The patient has to strongly bend his leg at the knee joint;
- lowering the foot onto the toes, and then onto the rest of the foot;
- inability or difficulty walking on your heels or raising the edge of the sole;
- pain on the outer part of the foot or lower leg;
- sensory disorders;
- amyotrophy.
Diagnosis of neuropathies of the tibial and peroneal nerves
The most successful treatment for neuropathy is treatment directly at the point of nerve damage. For successful treatment, your treating doctor will find out:
- At what exact point is the nerve damaged (compressed); this helps us provide targeted treatment;
- What exactly led to the nerve suffering (trauma, scar, compression);
- The degree of nerve suffering (complete or partial damage, the presence of a recovery process, the presence of complete death of the nerve, etc.).
Often, to establish the cause of nerve pain, a detailed neurological examination is sufficient , during which the strength of the muscles controlled by the nerve, the possibility of certain movements, sensitivity, the presence of pain points and seals along the nerve are assessed. Auxiliary diagnostic methods are electroneuromyography, radiography and computed tomography.
Electroneuromyography allows you to assess the speed and volume of impulses along the nerve, detect the location of damage/compression, and determine the prognosis for recovery. Electromyography helps us evaluate the effect of certain types of treatment and choose the most suitable ones. The Echinacea clinic uses a modern computer electroneuromyograph.
X-ray and computed tomography of the joints and feet will provide complete information about the deformation of the joints and bone canals of the nerves, the causes and points of compression of the nerve.
Stimulation electromyography of the lower extremities
Treatment and diagnosis
At the beginning of treatment, the doctor collects a complete anamnesis (history from the moment of onset) of the disease, after which an examination of the motor and sensory function of the nerves in the area of the diseased area is carried out. To do this, you should conduct special tests that objectively assess muscle strength. Electromyography and electroneurography and ultrasound of the nerve are used.
Based on the results of the study, treatment for peroneal nerve neuropathy is prescribed. To begin with, the influence of the cause of the disease is reduced, a drug with an anti-inflammatory and analgesic effect, vitamins and antioxidants are used. Physiotherapy, manual therapy and orthopedic prostheses are actively used. In extreme cases, surgery is indicated.
Treatment of damage to the tibial and peroneal nerves at the Echinacea clinic
When it is clear where, how and why nerve compression occurs, local treatment in the form of physiotherapy, therapeutic blockades, massage, and manual therapy becomes much more effective. Therefore, treatment in our clinic begins with finding out the cause and location of nerve damage .
The main goals of treatment for nerve compression:
- Remove nerve compression. To do this, we use powerful resorption therapy: we use enzymes that resolve and soften scar tissue, bone and cartilage growths (Karipazim enzyme, etc.), massage, and injecting medications directly into the site of nerve compression. Sometimes, to release the nerve, manual therapy and massage of the areas of compression of the tibial and peroneal nerves (spine, leg joints, etc.) are sufficient.
- Accelerate healing and restoration of the nerve. To do this, we use modern medications that help restore the nerve that has been released from compression in the scars.
- Restore muscle function and volume. Special exercises, electrical stimulation of muscles, and physiotherapy are used here. The rehabilitator will tell you in detail and show you how to perform rehabilitation procedures at home.
Carpal tunnel syndrome
Tunnel syndromes (compression-ischemic neuropathies) are the result of a conflict of nerve trunks and local musculoskeletal changes against the background of a disturbed motor pattern with myofixation or hypermobility of the affected part of the spine or limbs, leading to temporary or permanent compression of neural structures. Diseases can develop due to habitual forced positions of the body or limbs of a professional, sports or domestic nature, or traumatic changes in musculoskeletal structures. Predisposing factors are neuroendocrine diseases, pregnancy, contraceptive use, alcoholism, renal failure, some systemic diseases and blood diseases. In the area of compression, chronic trauma to the nerve trunk and its ischemia occur due to microcirculatory vascular disorders. In this case, tapping (percussion) of the affected nerve segment is accompanied by numbness, paresthesia, pain in the percussion zone and the corresponding neurotome. Techniques that increase canal stenosis or tension on the nerve and cause ischemia accentuate the symptoms of damage to the nerve trunks and are thus diagnostic. At least 50% of all tunnel neuropathies are caused by carpal tunnel syndrome, and somewhat less frequently – cubital tunnel syndrome. Neuropathies of the radial nerve associated with compression at the level of the elbow joint and shoulder, compression of the common peroneal nerve in the neck of the peroneal nerve (“mannequin disease”). Damage to the brachial plexus of nerves at the level of the upper thoracic outlet occurs regularly. Carpal tunnel syndrome is more common in middle-aged women engaged in intensive manual work. Compression of the nerve is facilitated by the congenital narrowness of the canal and neurodystrophic changes in the transverse carpal ligament. The median nerve enters the carpal tunnel under the fibrous band of the flexor retinaculum and is compressed at this level. Dysesthesia in 1-4 fingers, pain in the hand with radiation to the forearm, hyperhidrosis, swelling of the hand form the basis of the syndrome. Symptoms of the disease increase sharply at night, especially when lying on the affected side. Relief comes from shaking and rubbing the brush. In severe cases, patients cannot fall asleep due to severe pain in the arm. Thenar hypotrophy, weakness of abduction and opposition of the thumb are detected only in advanced cases several months or years after the onset of the disease. For the clinical diagnosis of the syndrome, positive symptoms of Tinel (light tapping of the median nerve at its entrance to the carpal tunnel with a finger) and Phalen (flexion or extension of the wrist at a right angle for 1 minute), elevation and tourniquet tests, which reproduce pain and dysesthesia in zone of innervation of the median nerve. Peroneal nerve tunnel syndrome. This term refers to a lesion of the common peroneal nerve in the osteofibrous canal at the level of its inflection on the outer surface of the neck of the fibula. The superficial location, weak vascularization, and tension of the nerve cause its increased sensitivity to direct (even minimal) trauma, pressure, traction, and penetrating injury. Among the causes that most often directly cause compression-ischemic damage to the nerve, it should be noted that squatting or kneeling (“occupational peroneal neuropathy”), unexpected sharp flexion with an inward rotation of the foot, the habit of sitting with crossed legs, an unsuccessfully applied plaster cast, compression by the boot rubber boot. The nerve can also be compressed when lying on its side on a hard surface of a table, bed, bench, as happens in patients in serious condition, in a coma, during a long operation under anesthesia, or while intoxicated. The uniqueness of the clinical picture of peroneal neuropathy lies in the predominance of the motor defect over sensory impairment. Weakness and atrophy of the extensors and external rotators of the foot develop, which hangs down, turns inward, and flops when walking. Over time, contracture develops with equinovarus foot deformity. Pain syndrome is absent or minimally expressed; paresthesia, sensory disorders are often limited to a small area on the dorsum of the foot. In the case of incomplete damage to the nerve, palpation is accompanied by pain, paresthesia in the innervation zone, and the effleurage symptom is positive. With more severe damage, these signs are absent. A careful examination of the patient by a competent specialist with the identification of carpal tunnel syndrome can hardly be overestimated, since this allows you to save the patient from numerous radiation and invasive studies, develop the correct treatment tactics, and provide him with real help. Conservative treatment is symptomatic and is aimed at improving blood circulation and relieving swelling in the area of nerve compression. Anti-inflammatory and analgesic, vascular drugs are widely used; single or repeated injections of glucocorticoids directly into the corresponding nerve canals and surrounding tissues are an adequate treatment method. A radical method of treatment is surgery to decompress the nerve, and its effectiveness reaches 80-85%.
When is surgery necessary?
In case of nerve injury, it is very important to decide in a timely manner whether conservative or surgical treatment is advisable. The answer to this question can be obtained after conducting needle myography, which will answer the question of what is the degree of damage to the nerve and whether it has a tendency to recover. If during this study it turns out that at least partially the nerve is preserved, we carry out active conservative treatment, after which we must repeat the study to make sure that the treatment had an effect . If, during needle myography, it turns out that the nerve is completely damaged and its restoration is impossible, we resort to the help of a neurosurgeon who suturing the nerve or releasing it from significantly narrowed canals. Then we perform the entire range of restoration procedures.
What you need to know about the disease
This pathology of the lower extremities is also called peroneal neuropathy or compression ischemic neuropathy of the peroneal nerve. Since the peroneal nerve has a specific structure, it is more susceptible to damage during metabolic failures and anoxia. This factor largely influences the prevalence of the disease. It is known that neuropathy (neuritis) of the peroneal nerve occurs in more than 60% of patients who have ever undergone surgery or are being treated in traumatology. A very small percentage (about 30%) is occupied by people whose nerve damage was primary.
Tunnel and post-traumatic neuropathy of the peroneal nerve
Post-traumatic neuropathy of the peroneal nerve is more often diagnosed in young people leading a mobile active lifestyle. Any knee injury can cause scar tissue to develop. It interferes with the normal passage of nerve fibers. Tunnel neuropathy of the peroneal nerve is formed, which is manifested by sagging of the foot, pain in the lower leg, foot, and little toe.
The most common causes of clinical symptoms of traumatic neuropathy:
- surgical operations on the knee joint (plasty of the ligamentous apparatus, removal of the meniscus, endoprosthetics, etc.);
- improper application of a plaster cast, which puts pressure on the tunnel through which the peroneal nerve passes;
- post-traumatic contracture;
- cicatricial deformation of ligamentous, tendon and muscle tissue;
- the formation of a rough callus after a fracture or crack of the head of the fibula (or its lower condyle).
To treat post-traumatic neuropathy, it is necessary to first eliminate the cause of its occurrence. If these are scars or callus, then measures are taken to eliminate them. In case of inflammatory edema or stagnation of lymphatic fluid at the site of a traumatic violation of the integrity of soft tissues, measures are taken to drain excess fluid. To prevent thrombosis and the development of varicose veins of the lower extremities during a long period of decreased physical activity, it is recommended to use special compression garments.