Trigeminal and facial neuralgia
Neuralgia is a disease in which damage or compression of the trigeminal nerve and/or its branches occurs. This causes a sharp piercing pain that occurs suddenly and brings physical and psychological discomfort to the patient. Despite the fact that the term “neuralgia” can be literally translated as “nerve pain,” the matter is not limited to pain. Trigeminal and facial neuralgia are radically different in symptoms. The facial nerve contains mostly motor fibers, so neuralgia leads to dysfunction of the facial muscles (the degree depends on the severity of the disease), and can also cause lacrimation, dry eyes and partial loss of taste. Pain in facial neuralgia is usually concentrated in the area of the parotid gland (the patient complains that the pain radiates to the ear), but there may be no pain at all. It is because of the lack of pain that some experts use the term “neuropathy” when talking about damage to the facial nerve. With the trigeminal nerve it’s exactly the opposite, since it contains many sensory fibers.
Symptoms and diagnosis
Fothergill's disease manifests itself with the following symptoms:
- extremely severe paroxysmal acute pain comparable to an electrical discharge;
- the attack lasts on average 10-15 seconds, but no more than 2 minutes;
- at peak moments, twitching of the facial muscles, lacrimation, increased salivation, and local redness of the skin are observed.
Usually the pain is localized on the right side; left-sided or bilateral neuralgia is less commonly diagnosed.
Based on location, the following common forms of the disease are distinguished:
- Auriculotemporal neuralgia (Frey's syndrome) .
Acute pain is concentrated in the area of the anterior wall of the ear canal, inner ear, temple, and often the pain radiates to the lower jaw. The attack is accompanied by redness of the skin and severe sweating in the temple area. - Nasociliary (Charlin's syndrome) . Pain sensations are concentrated above the eyebrow and at the outer edge of the eye. The patient suffers from recurrent conjunctivitis and photophobia.
- Neuralgia of the auricular nerve . The patient experiences severe pain in the ear, the disease is accompanied by decreased hearing, auditory hallucinations, impaired coordination of movements, and headaches.
To treat the disease, the patient turns to a neurologist, who conducts an initial examination and prescribes a number of diagnostic procedures.
The diagnostic complex includes:
- MRI . The procedure helps to identify or exclude the presence of multiple sclerosis or neoplasms in the cranial cavity.
- Magnetic resonance angiography . The study makes it possible to identify impaired blood supply and pinching of the trigeminal nerve.
- Examination by a dentist . The doctor examines the teeth for caries and improperly installed fillings and dentures.
- Electromyography . The test shows the ability of nerve endings to conduct electrical impulses.
- A blood test is also necessary to diagnose pathology. The test allows you to identify or exclude a viral infection that could cause the development of pathology.
Read more about the symptoms and diagnosis of trigeminal neuralgia here.
Symptoms of neuralgia
- Facial pain (prosopalgia). A characteristic sign of neuralgia. Sharp and sudden, reminiscent of an electric shock. Usually lasts from 5 to 15 seconds, is paroxysmal in nature and can occur at any time. During periods of remission, the number of attacks decreases. Most often, pain occurs in the area of the cheekbones and lower jaw (both right and left), and can be localized in almost all areas of the face.
- Impaired sensitivity. A severe form of neuralgia can lead to partial or complete loss of sensitivity of the skin.
- Nervous tic of the eyelid (nystagmus), spasms and twitching of facial muscles.
- Loss of coordination and motor skills are rarer manifestations of severe forms of the disease.
- Headaches, fever, chills and weakness are syndromes caused by viruses and infections.
Symptoms
The intensity of pain from trigeminal neuropathy varies depending on the type of neuropathy, and can range from sudden, severe and stabbing to constant, aching, burning. Intense attacks of pain may be triggered by vibration or contact with the cheek (for example, when shaving, washing the face or applying makeup), while brushing teeth, eating, drinking water, talking, or being exposed to wind. The pain may involve a small area of the front of the face or may cover a large area. Attacks of pain rarely occur at night when the patient is sleeping.
NTN is characterized by attacks of pain that stop for a while and then return, but the disease can progress. Attacks of pain often get worse over time and pain-free periods become shorter. Eventually, pain-free intervals disappear and medications used to control pain become less effective. The disease is not fatal, but can be debilitating for the patient. Due to the intensity of the pain, some patients may avoid daily activities or social contacts because they are afraid of the sudden onset of an episode of pain.
Causes
Unlike neuritis, neuralgia is not an inflammatory disease. Fever, fever, swelling and other symptoms of the inflammatory process are not associated with this disease. However, if the trigeminal nerve is damaged due to neuritis, pain sensations that fit the description of neuralgia may well occur. To avoid confusion and differentiate the two pathologies, it is necessary to consider their etiology.
The cause of neuritis (like any other inflammatory disease) is viruses and infections that cause gradual destruction of the membrane and nerve trunk, and classical neuralgia in the vast majority of cases occurs due to mechanical effects on the nerve. Today, experts identify dozens of factors that provoke the development of the disease.
Main causes of neuralgia
- Head injuries leading to changes in the cranial structure and displacement of bones.
- Benign and malignant tumors that, as they grow, compress the trigeminal nerve.
- Various bite pathologies and other dental anomalies.
- Pathologies of the structure and diseases of blood vessels located in close proximity to the nerve (atherosclerosis, aneurysm, vasodilatation, etc.).
- Sinusitis and otitis in chronic form.
- Trigeminal neuralgia after tooth extraction. Occurs during a traumatic or incorrectly performed extraction procedure.
- Damage as a result of infection resulting from a number of diseases: periodontitis, periodontitis, stomatitis, herpes, syphilis.
Trigeminal neuralgia from hypothermia occurs rarely. However, this factor contributes to the development of the disease and complicates treatment. The same can be said about decreased immunity, metabolic disorders, neurosis, diabetes and other complicating factors.
- Surgery
- Oncology
- Neurosurgery
- Radiology and Radiation Therapy
- Gynecology and new reproductive technologies
- Traumatology and Orthopedics
- Cardiology
- Neurology
- Laser surgery
- Urology, andrology and microsurgery
- Plastic surgery
- Mammalogy
- Lithotripsy
- Psychological support service
- ECO
- Weight loss
- Pressure chamber
- Endovascular surgery
- Pituitary adenomas
- Arnold-Chiari malformation and syringomyelia
- Parkinson's disease
- Hydrocephalus
- Hemifacial spasm
- Herniated discs
- Violent movements
- Brain tumors
- Vascular diseases of the brain
- Trigeminal neuralgia
- Glossopharyngeal neuralgia
- Essential tremor
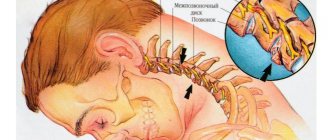
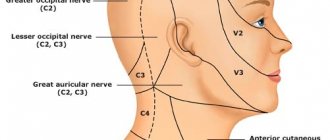
The trigeminal nerve (V pair of cranial nerves) contains sensory, motor and autonomic fibers (Fig. 1). The nuclei of the trigeminal nerve are located in the brain stem, at the exit from which the fibers that make up the large root reach the top of the pyramid of the temporal bone, where the trigeminal ganglion (Gasserian ganglion) lies, from which 3 branches extend: the orbital (sensory) nerve leaves the skull through the superior orbital gap, innervates the upper eyelid, conjunctiva of the eye, skin of the forehead and scalp in front; the maxillary (sensitive) nerve leaves the skull through the round foramen, penetrates the pterygopalatine fossa, innervates the skin of the lower eyelid, cheeks and nose, mucous membrane of the nasal cavity, upper jaw, etc.; The mandibular nerve (the small root of the trigeminal nerve, containing motor fibers, joins it) leaves the skull through the foramen ovale, innervates the skin of the lower part of the face, the mucous membrane of the cheeks, tongue, lower jaw, masticatory muscles, etc. The trigeminal nerve takes part in many reflexes ( corneal, mandibular, etc.). Fig. 1 Anatomy of the trigeminal nerve and its branches. Trigeminal neuralgia is a disease accompanied by paroxysmal intense unilateral facial pain in the area of the chin, lips, gums, cheeks, eyes, lasting several seconds or minutes. As a rule, middle-aged and elderly people suffer. A characteristic feature is the ability to cause pain by touching a specific area of the face or mouth.
Clinic and diagnostics.
The first attack of pain seems subjectively so pronounced and unexpected that, as a rule, patients well remember all the circumstances of the initial paroxysm even after many years. Sometimes the disease begins gradually with a slight unpleasant feeling of twitching, “electrification” in a certain area of the face, or with a toothache, which forces you to seek help from a dentist. Only the characteristic paroxysmal pain that subsequently appears allows a correct clinical diagnosis to be made and appropriate examination and treatment to be carried out. Trigger zones for the development of an attack (trigger zones) with trigeminal neuralgia are localized close to the midline, covering the lips, wings of the nose, eyebrows and chin, in rare cases located in the external auditory canal. Localization of trigger zones on the gums, tongue and palate makes it impossible to eat, talk, and perform basic hygiene requirements. Some patients with a similar arrangement of the trigger zones and severe pain lose weight, become weak and fall into a depressive state, sometimes leading to suicide attempts. The attacks recur day and night for several weeks, and then often subside. After some time, the disease appears again, and after a few years the attacks become permanent. The diagnosis of trigeminal neuralgia is confirmed by relief of pain when taking carbamazepine drugs (finlepsin, tegretol). After several years of taking carbamazepine, the effectiveness of the previous dosage usually decreases and there is a need to increase the dose of medication. Some patients cannot tolerate this drug due to side effects such as drowsiness, dizziness and staggering when walking, pain in the liver, suppression of white blood cells (leukopenia). The cause of such facial pain in most cases is compression of the trigeminal nerve root by an arterial vessel at the level of the posterior cranial fossa. Less commonly, trigeminal neuralgia can be caused by brain tumors or multiple sclerosis. Trigeminal neuralgia in multiple sclerosis, tens of times lower in frequency than typical trigeminal neuralgia, occurs as a result of demyelination of trigeminal sensory structures, mainly the entrance zone of the sensory root and the descending tract of the trigeminal nerve. It is likely that the subsequent replacement of foci of demyelination by glial cells, causing an increase in the excitability of neighboring sensory fibers, also contributes to the persistence of the pain syndrome. In addition, the development of trigeminal neuralgia in patients with multiple sclerosis may be due to vascular compression of the trigeminal sensory root. Trigeminal neuralgia in brain tumors can occur with tumors of the posterior and middle cranial fossa, pituitary tumors, epidermoids in the case where tumor growth leads to direct compression of the trigeminal nerve root or changes the spatial relationship of vessels and nerves in such a way that one of the vessels leads to compression of the trigeminal nerve root (Fig. 2). Fig. 2 Trigeminal neuralgia with epidermoid tumor. Intraoperative photography. 1 – tumor. 2 – trigeminal nerve root. To exclude a brain tumor, vascular pathology, or multiple sclerosis, all patients undergo magnetic resonance imaging (MRI) of the brain. Often in such photographs you can see the “culprit” vessel compressing the trigeminal nerve root.
Treatment.
The diagnosis of neuralgia is confirmed by relief of pain when taking carbamazepine drugs (finlepsin, tegretol). After several years of taking carbamazepine, the effectiveness of the previous dosage usually decreases and there is a need to increase the dose of medication. Some patients cannot tolerate this drug due to side effects such as drowsiness, dizziness and staggering when walking, pain in the liver area. Surgical treatment is indicated for patients who cannot tolerate carbamazepine drugs or when their effectiveness decreases. Our center is a leading institution in Russia performing all types of surgical interventions for trigeminal neuralgia with more than 20 years of experience in the diagnosis and treatment of this disease. A method of treating pathology that has proven to be highly effective is percutaneous radiofrequency trigeminal rhizotomy, an operation that involves partial destruction of the trigeminal nerve root under local anesthesia. The procedure is carried out as follows: a) a thin needle is passed through the face to the base of the skull under X-ray control (Fig. 3). Fig. 3 Percutaneous high-frequency trigeminal rhizotomy in a patient with trigeminal neuralgia of the I-II branches. Intraoperative radiography (lateral projection), confirming the correct position of the curved electrode b) stimulation of the root is carried out, which is accompanied by a pain attack in the “sick” area of the face. This stage of surgery is the most unpleasant for patients. c) partial destruction of the root is carried out due to setting an increased temperature at the tip of the needle until sensitivity in the desired area of the face decreases. Such an operation may be preferable for elderly people, those who are afraid of open surgery, and those with multiple sclerosis. In most patients, after a few years (on average 5–7 years), the numbness in the face disappears, and facial pain reappears. A more physiological operation that does not lead to numbness in the area of innervation of the trigeminal nerve is the operation of vascular decompression of the facial nerve root (Microvascular decompression). This is a microsurgical operation performed under general anesthesia, in which, after performing a small trepanation behind the ear on the side of pain, the vessel is diverted from the trigeminal nerve root in the posterior cranial fossa (Fig. 4 and 5). The effectiveness of this technique is more than 90% if patients are correctly selected for surgery. Fig. 4 Intraoperative photo of a patient with trigeminal neuralgia. The arrow indicates compression of the input zone of the trigeminal nerve root by the loops of the superior cerebellar artery (V - trigeminal nerve, SMA - 2 branches of the superior cerebellar artery, CV - petrosal vein) Fig. 5 Intraoperative photo: decompression of the input zone of the trigeminal nerve root at the brain stem was performed (V - trigeminal nerve, SMA - loop of the superior cerebellar artery, M - fragment of muscle tissue) The recovery process after microvascular decompression surgery rarely takes more than a week, after which patients are discharged home and forget about their disease forever.
Classification of the disease
Due to the occurrence
- Primary (idiopathic) trigeminal neuralgia. A classic type of neuralgia, so to speak. Occurs due to compression of the trigeminal nerve.
- Secondary trigeminal neuralgia is a consequence of other diseases and viruses.
By coverage
- Unilateral (one branch of the trigeminal nerve is affected).
- Bilateral (more than one branch is affected).
Neuralgia can affect the 1st, 2nd, 3rd branches of the trigeminal nerve. The first branch is responsible for the orbital zone, the second for the median zone (including the nose and upper lip), and the third for the lower jaw. Most often, damage to the third branch is diagnosed, so the pain affects the area of the lower jaw, and an attack often occurs during hygiene, eating or shaving.
Treatment
Treatment options include medication, surgery, and multimodal treatment.
Medications
Anticonvulsants, used to block nerve stimulation, are generally effective in treating type 1 NTN but are often less effective in treating type 2 neuropathy. These drugs include carbamazepine, oxcarbazepine, topiramate, gabapentin, pregabalin, clonazepam, phenytoin, lamotrigine, and valproic acid.
Tricyclic antidepressants such as amitriptyline or nortriptyline may also be used to treat pain. Analgesics and opioids are usually not effective for treating acute, recurrent pain caused by T1, although some patients with T2 respond to opioids. Ultimately, if treatment does not relieve pain or results in significant side effects such as cognitive impairment, memory loss, excessive fatigue, bone marrow suppression, or allergies, then surgery may be recommended. Because trigeminal neuropathy is most often a progressive disease that becomes drug-resistant over time, patients often seek surgical treatment.
Surgery
Several neurosurgical techniques are generally used to treat NTN, depending on the nature of the pain, the wishes of the individual, physical health, blood pressure and the presence of previous operations. Some procedures are performed on an outpatient basis, while others, which are performed under general anesthesia, are performed in a hospital setting. After these surgical procedures, there may be some reduction in the face and it is not uncommon for NTN to recur, even if the procedure was initially successful. Several procedures will be used. These are like:
- Rhizotomy is a procedure in which nerve fibers are damaged to block pain. Rhizotomy to treat NTN always causes some degree of sensory loss and facial numbness.
- Glycerin injections are an outpatient procedure that is performed after light anesthesia. This form of rhizotomy usually results in pain relief within 1-2 years. However, this procedure can be repeated several times.
- Radiofrequency thermal ablation is most often performed in an outpatient setting.
- Stereotactic radiosurgery (using Gamma Knife or CyberKnife) uses CT scanning to deliver highly focused radiotherapy to the area where the trigeminal nerve exits the brain stem. This causes slow nerve damage, which disrupts the transmission of sensory signals to the brain. Patients who have had this procedure can go into remission for up to three years.
- Microvascular decompression is the most invasive of all surgeries for treating NTN, but it also has the best long-term results and the lowest likelihood of pain recurrence. About half of people who have this procedure will experience periodic pain for 12 to 15 years.
- A neurectomy, which involves a partial incision of the nerve, can be performed at the nerve's entry point into the brainstem while attempting microvascular decompression. A neurectomy can also be performed by cutting the superficial branches of the trigeminal nerve on the face.
Surgical management of T2 is usually more problematic than for T1, especially where vascular compression is not detected on neuroimaging.
Additional treatments
Some patients benefit from combining medications with other treatment methods. These methods have varying degrees of effectiveness. Some patients find that gentle exercise, yoga, creative visualization, aromatherapy, or meditation can help. Other treatment options include acupuncture, chiropractic care, biofeedback, vitamin therapy, and nutritional therapy. Some patients note a certain effect from the use of botulinum toxin.
Types of trigeminal neuralgia
There is an additional classification that can also be used in making a diagnosis.
Acute
Acute trigeminal neuralgia, accompanied by frequent and severe attacks.
Chronic
Chronic trigeminal neuralgia is a consequence of an untreated disease. The patient has been observed for a long time: remissions alternate with exacerbations.
Atypical
Atypical trigeminal neuralgia occurs against a background of stress and nervous exhaustion (psychosomatics).
Postherpetic
Postherpetic trigeminal neuralgia occurs after a history of herpes and its symptoms differ from the classic type. The pain is usually burning and may not go away for two to three hours.
Kinds
There are 2 types of trigeminal neuralgia:
- primary (true) - is a separate pathology, which is characterized by compression of the trigeminus or a disorder of the blood supply in the area of its passage;
- secondary – a consequence of other pathological processes (neoplasms, infections, bone transformations, destruction of the myelin sheath of nerve fibers).
The pathological process can involve all three branches of trigeminus or only one or two.
Diagnosis of the disease
Modern medicine has in its arsenal many diagnostic techniques that make it possible to determine the type of neuralgia and the cause of its occurrence:
- visual examination and questioning of the patient;
- X-ray of the jaw;
- MRI of the brain and blood vessels;
- laboratory analysis of urine and blood;
- electromyography.
Diagnosis is carried out by a neurologist, but additional examinations by other specialists are often required: dentist, ophthalmologist, otolaryngologist. Particular attention is paid to differential diagnosis, since neuralgia may resemble other diseases in its symptoms, in particular glaucoma, otitis media, ethmoiditis, Slader syndrome, etc.
Treatment of trigeminal neuralgia
Treatment and drugs
For successful treatment, complex drug therapy is used. First of all, these are anticonvulsants (carbamazepine, finlepsin or clonazepam), which are included in the mandatory rehabilitation program and relieve the main manifestations of neuralgia. The dosage and duration of treatment are determined strictly by the attending physician.
For additional effect, antihistamines and local pain relievers may be prescribed. To compensate for the lack of gamma-aminobutyric acid (a kind of mediator between the brain and the nervous system), baclofen, phenibut or gabapentin are prescribed. In the stage of exacerbation of neuralgia, specialists often prescribe antidepressants to eliminate psychological discomfort (the most common remedy is finlepsin). If the cause of the disease is a virus or infection, antiviral and antibacterial agents, as well as NSAIDs, are prescribed. During the recovery period, it is recommended to take B vitamins.
Physiotherapy
To eliminate pain, novocaine blockades and sodium hydroxybutyrate injections are actively used. The most popular and effective physiotherapeutic techniques: acupuncture, ultraphonophoresis, magnetic therapy, and low-frequency laser therapy. Massage for trigeminal neuralgia is also a good addition to general treatment and allows for better blood circulation.