Doctors distinguish several types of vegetative-vascular dystonia (VSD):
- cardiac;
- hypotonic type;
- according to the hypertensive type;
- respiratory;
- abdominal;
- mixed.
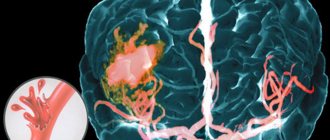
The cardiac form of VSD is manifested by symptoms of cardiac dysfunction: heart pain, burning in the chest, tachycardia or bradycardia, arrhythmia. Chest pain may resemble pain caused by angina pectoris. In all cases of chest pain due to VSD, doctors at the Yusupov Hospital, using the latest instrumental and laboratory research methods, exclude acute myocardial infarction, stop the vegetative crisis and carry out treatment aimed at preventing heart pain.
Causes of pain in the heart in the cardiac form of VSD
There are several risk factors that can cause cardiac dysfunction in VSD:
- aggravated hereditary predisposition;
- primary deviations in the functioning of the autonomic nervous system;
- emotional and psychological stress.
Chest pain, freezing, heart tremors, neurotic pain in the chest with VSD are caused by the following predisposing factors:
- endocrine diseases;
- neurological disorders;
- fatigue, physical and mental stress.
Doctors at the Yusupov Hospital first establish the cause of the cardiac form of VSD, eliminate it, influence the mechanism of development of symptoms of cardiac dysfunction, and relieve the symptoms of the disease.
Symptoms of the cardiac form of VSD
VSD of the cardiac type is difficult to distinguish from other forms of vegetative-vascular dystonia, since all its varieties are characterized by cardiac disorders. A distinctive feature of VSD is pain in the heart area. How does the heart hurt with VSD? Pain in the heart area during VSD can be pressing, stabbing and burning. The patient experiences discomfort in the chest during an attack. They are similar in nature to signs of coronary heart disease. When examining patients with such complaints, doctors do not detect signs of myocardial infarction or other cardiac pathology.
For heart pain due to VSD, most patients are not helped by nitroglycerin preparations. The lack of a positive result after taking medicinal heart is due to the fact that nitroglycerin lowers blood pressure, the levels of which in VSD are already below normal. Against the background of such effects of cardiac drugs, the patients’ well-being only worsens. Nitroglycerin does not relieve pain associated with myocardial infarction. For this reason, despite the obvious nature of chest pain during VSD, doctors at the Yusupov Hospital must register an electrocardiogram for patients, and patients are advised by a cardiologist.
Symptoms of the cardiac form of VSD can manifest themselves with varying severity. The pain syndrome does not have a clear area of localization; the pain spreads throughout the entire heart and differs in intensity. Patients often note disturbances in the rhythm of the heartbeat, extrasystoles with VSD. They experience a rapid heartbeat (tachycardia). Patients complain of freezing, heart palpitations, and tachycardia after breakfast. A low pulse may be detected with VSD. Nocturnal tachycardia with VSD causes a feeling of fear in patients and can cause a panic attack.
Signs of VSD of the cardiac type intensify in stressful situations and with hormonal changes that occur during puberty in adolescents, as well as in women upon the onset of menopause or when bearing a child.
The course of the disease is accompanied by the periodic occurrence of signs of one of the syndromes:
- cardialgic - aching, stabbing, bursting pain in the chest, burning in the heart area;
- tachycardic – increased heart rate up to 90 beats per minute or more, decreased performance;
- bradycardic – slowing down the heart rate to 60 beats per minute or less, increased sweating, headache, dizziness, malaise;
- arrhythmic - extraordinary cardiac contractions (extrasystoles), heart beats.
Depending on the leading syndrome of the cardiac form of VSD, doctors at the Yusupov Hospital draw up a treatment regimen for the patient. Doctors discuss complex cases of cardiac pathology, manifested by pain in the heart area, changes in heart rate and blood pressure, and extrasystole at a meeting of the Expert Council, in which candidates and doctors of medical sciences take part.
Sinus rhythm and sinus tachycardia
Normally, the heart rhythm is set from the sinus node, so the sinus rhythm of the heart is the norm. Sinus tachycardia is a rapid heart rate (more than 90 beats per minute), set, as expected, from the sinus node. Sinus tachycardia in children is determined by other indicators of heart rate - according to the age norm, since the normal heart rate in children is higher than in adults.
Palpitations - a feeling of rapid or increased heartbeat. Often combined with tachycardia. Palpitations are a subjective symptom. Some people periodically feel even normal heartbeats, while others may not feel serious rhythm disturbances. Therefore, the feeling of heartbeat itself is not a sign of heart disease.
Increased heart rate is a normal reaction of the body to physical activity and stress, which is felt as palpitations and tachycardia. As a rule, this is sinus tachycardia, which occurs as a result of complex regulatory mechanisms of the cardiovascular system and, above all, an increase in the sympathetic influence on the cardiac pacemaker - the sinus node. The increased sinus rhythm of the heart allows the tissues to be supplied with oxygen and nutrients more actively, since during physical activity energy needs increase significantly. Sinus tachycardia of the heart after rest goes away on its own and does not cause discomfort.
Only in combination with other symptoms can a heartbeat indicate deviations from the norm. The symptoms that accompany palpitations depend on the disease of which they are a manifestation.
Relief of heart pain during VSD
Therapy for the cardiac form of VSD consists of a set of therapeutic measures in different directions:
- drug treatment;
- power control;
- moderate physical activity;
- normalization of work and rest schedules;
- psychotherapy sessions;
- physiotherapeutic procedures.
Pain in the heart during VSD, symptoms of cardiac dysfunction disappear after taking twenty drops of Corvalol, Valocordin, and motherwort tincture. If the patient is bothered by a slight aching pain in the heart, accompanied by depression, but not affecting physical activity, menthol or regular valerian can be used as a distraction. If burning, prolonged pain of varying intensity occurs, sometimes too strong to endure and requiring emergency care, non-steroidal anti-inflammatory and sedative drugs are taken.
In case of paroxysmal, prolonged pain that occurs unexpectedly, but quickly spreads throughout the chest and is not relieved by taking nitroglycerin, you should immediately call an ambulance. Pain in the heart area that occurs during periods of exacerbation of VSD, which accompanies any physical activity, intense walking and can continue during a period of rest, requires complex therapy. If short-term paroxysmal pain lasts no more than 20 minutes, appearing against the background of emotions or experiences.
Short-acting beta blockers (anaprilin) help with palpitations. They should not be taken if there is severe bradycardia. In this case, belladonna preparations will help. Rhythm disturbances (extrasystoles) with VSD go away on their own. If heartbeats occur frequently and cause discomfort, contact a cardiologist.
To improve the condition and reduce the severity of the symptoms of the disease, it is necessary to positively influence the autonomic system of the body and influence the signs of illness. To achieve the desired effect, the patient is recommended to change lifestyle, attend psychotherapy sessions, take tonics and follow the recommendations of the attending physician.
Any tension of a neurotic nature can be relieved by massage, taking sedatives and sedatives. If there is a fear of death provoked by VSD, psychotherapists work with the patient. Psychoanalysis and Gestalt therapy have a high effectiveness rate. A revolutionary psychotherapeutic method used for VSD is EDMR therapy. It gives amazing results in combination with Ericksonian hypnosis.
Prevention of attacks of heart pain during VSD
Heart pain, fading, and tremors of the heart during VSD do not threaten the patient’s life. Sometimes the attack lasts for several days, but is well treated with validol and sedatives. If discomfort in the chest increases, or a feeling of cardiac arrest occurs during VSD, the patient is provided with rest, a comfortable body position, fresh air and sedatives. If a connection is noticed between increased pain in the chest during deep exhalation and inhalation, the patient is taught to normalize breathing using breathing exercises.
To minimize the risk of recurrence of attacks of pain in the heart during VSD, patients are advised to adjust their lifestyle:
- Sleep at least eight hours a day;
- Regularly engage in physical labor of moderate intensity;
- If your professional activity requires a sitting position, you should do gymnastics 1-3 times a day;
- Eat as natural a diet as possible with a predominance of raw vegetables and fruits;
- Eliminate psycho-emotional stress, learn to have a neutral attitude towards failures and problems;
- Get regular check-ups with a cardiologist.
If you have heart pain, nocturnal tachycardia, increased heart rate after eating and other signs of VSD, call +7. Doctors at the Yusupov Hospital will relieve an attack of heart pain and other symptoms of VSD and will provide comprehensive treatment aimed at preventing vegetative-vascular cardiac crises. In the rehabilitation clinic, patients are individually selected the most effective physiotherapeutic procedures, gymnastic exercises, and are taught breathing exercises. Psychotherapists use innovative methods to support the patient during an attack of pain and in the inter-attack period.
Why does tachycardia occur with VSD?
Vegetative-vascular dystonia is traditionally classified as a neurological pathology.
But a patient with this nosology can turn not only to a general practitioner or family doctor; sometimes patients go straight to a cardiologist or gastroenterologist. It all depends on the leading symptoms. Why are the manifestations of VSD so diverse? Let's first delve a little deeper into the anatomical subtleties of the problem under discussion. Our nervous system is divided into somatic, which is responsible for skeletal muscles (and therefore movements), as well as autonomic, which controls the activity of internal organs and the vascular bed. Therefore, any failures or insufficiency in the functioning of the latter will lead to disruption of the functioning of almost the entire organism. Hence the diversity of the clinical picture in patients with VSD.
The autonomic department, in turn, is divided into sympathetic and parasympathetic. The first “enters the arena” during wakefulness and in stressful moments (it is this that causes the appearance of tachycardia), and the second, on the contrary, dominates during periods of rest.
Normally, these antagonists are in harmony, alternately replacing each other. But there is such a disease as VSD, in which the physiological balance is disturbed. The course of the pathology is most often paroxysmal. Paroxysms are accompanied not only by increased heart rate, but also often by pain in the stomach, a lump in the throat, a feeling of lack of air, trembling in the body, and sweating. Simply put, they are manifested by a whole “bouquet” of symptoms, which for each patient make up their own unique clinical picture.
As a result, the imbalance described above occurs is currently not known with certainty. We can only state the fact of a decrease in the influence of the cerebral cortex on the autonomic system, which is why it begins to “live its own life.” Most doctors are inclined to believe that the key role in the development of nosology belongs to psychogenic factors, that is, it is formed against the background of emotional disorders.
For more information about the causes, symptoms and treatment of VSD, watch the video at the link below.
If you feel tachycardia, you should not immediately attribute it to dystonia. After all, it can occur against the background of physiological conditions, for example, pregnancy. And often an increased heart rate accompanies anemia, osteochondrosis, increased body temperature due to infectious diseases, etc.
What types of tachycardia with VSD are most common?
During an attack of vegetative-vascular dystonia of a cardiac nature, that is, manifested by cardiac symptoms, two types of tachycardia are observed (increased heart rate more than 80 beats/min). These are sinus, in which impulses come from the physiological pacemaker, and paroxysmal supraventricular. The latter is characterized by the presence of a pathological focus of excitation generation along the path of the discharge from the atria to the ventricles.
Both of them rarely occur as an isolated symptom. In most cases, a sympathoadrenal crisis is accompanied by a bursting headache, severe nausea leading to vomiting, fear, and tremors in the hands.
In this section of the article, I would like to answer one of the frequently asked questions: can VSD and the tachycardia associated with it become a “get rid of” the army. In some cases, pathology is indeed an obstacle to service. But only when paroxysms occur at least once a month and are accompanied by a vivid clinical picture (fainting, heart pain, which does not decrease after taking medications). And, most importantly, all of the above must be recorded in writing by doctors, and also supported by all kinds of examinations.