What does the word lumboischialgia mean?
Sciatica is pain in the lower back that extends to one or both lower limbs. It is a reflex syndrome and belongs to the non-radicular phase of lumbar osteochondrosis, as well as lumbodynia and lumbago. Therefore, it would be more correct to say that there is lumboischialgia syndrome on the right or lumboischialgia syndrome on the left.
What is “discogenic lumboischialgia”?
If during diagnosis it is established that the cause of such complaints is a disc herniation or protrusion, then we can say that this is discogenic lumboischialgia.
How is it going?
If the pain occurs acutely and is of a pronounced nature, then this is acute lumboischialgia. If the pain is moderate and bothers you for a long time, periodically exacerbating, this is chronic lumboischialgia.
What can lumboischialgia be?
Depending on the nature of neurological disorders, vascular, muscular-tonic, and muscular-dystrophic forms of lumboischialgia are distinguished.
What causes lumboischialgia syndrome to appear?
Vertebrogenic lumboischialgia syndrome most often occurs after hypothermia, as well as after increased stress on the muscles of the lower back and legs. As a result, tonic muscle strain occurs and pain appears in the lower back and leg.
Causes of pain
5 pairs of nerve roots in the lumbosacral region combine to create the sciatic nerve. Beginning at the back of the pelvis (sacrum), the sciatic nerve travels behind the buttocks and down through the hip joint into the lower extremities. Nerve roots are not separate structures, but part of the body's overall nervous system, capable of transmitting pain and sensations to other parts of the body. Radiculopathy is caused by nerve root compression, disc rupture, or bone growth between the nerve root and the sciatic nerve.
Symptoms of lumbar sciatica and diagnosis of lumbar sciatica
The main complaints are pain in the lower back and legs. Both lumbar sciatica on the right and lumbar sciatica on the left are equally common, but bilateral lumbar sciatica is much less common. The pain is usually not as severe as with lumbago and the radicular stage of lumbar osteochondrosis (radiculitis). However, they are more intense than with chronic lumbodynia. Most often, the pain is severe or moderate in nature.
According to the subjective characteristics, it is aching, burning, squeezing, localized in the lower back or leg.
What to do in case of an attack of pain?
At the first stage, first of all, you should observe bed rest, limit any movements, it is better to take a pose with support on your healthy leg. When lying on your back, it is recommended to place a small pillow under your lower back and knees. If you cannot lie down, you should shift your weight from one leg to the other alternately and move more often. With light dynamic movements, the muscles relax faster. Take pain medication as prescribed by your doctor.
At the second stage, you can use dry heating (a warm heating pad, a heat-retaining blanket) or a compress with herbal tinctures on the affected area. It is not recommended to use heat at elevated temperatures. In the absence of contraindications, you can perform a massage with rubbing and kneading of the lumbar region and limbs.
To prevent relapses, it will be useful to wear a fixing corset, and for pregnant women, a prenatal bandage if there is a noticeable increase in the abdomen. All intramuscular injections should be performed by trained medical personnel and placed only in the unaffected leg.
Vascular disorders in lumboischialgia
Vessels are narrowed
Studies have shown that the vascular tone of the legs in patients with lumboischialgia is most often increased. This is a vasospastic variant of this syndrome. In other words, the vessels are narrowed in this case.
And if vascular tone is increased, then patients note chilliness in the leg. She may be paler and colder to the touch than healthy. And the temperature in the lower leg and foot of the diseased leg is slightly lower than the healthy one. The most interesting thing is that after physical activity the temperature difference only increases. On the sore leg, the temperature drops even more, while under normal conditions it should rise. Temperature asymmetries are detected not only on sore and healthy legs. In some cases, even in a limited area of the affected leg, the temperature may be different at nearby points.
Vessels are dilated
When vascular tone is reduced, this is a vasodilatory variant of lumbar ischialgia syndrome. However, this manifestation is much less common. But if vascular tone is reduced, then a feeling of heat or warmth appears in the affected limb, and its temperature rises. (V. P. Veselovsky)
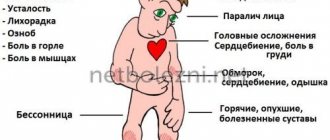
MAIN SIGNS OF SCIATIAL NERVE SCHIALGIA:
- pain pierces the leg along the entire length of the nerve, involving the buttock, thigh, pit under the knee, calf muscle and foot;
- movement is limited, a person cannot stand, sit, or bend over;
- if the patient tries to move his leg, the pain becomes stronger;
— it is difficult to lift the foot, the leg bends poorly;
— periodically strong tingling and “goosebumps” appear in the leg;
- pain does not disappear even when the leg is absolutely motionless;
- in some cases, the lower part of the leg loses sensitivity;
- the pain decreases slightly if the patient, while in a supine position, pulls his leg bent at the knee towards him.
Autonomic disorders in lumboischialgia
When examining patients, a large number of autonomic disorders are determined. Initially, there is limited pallor of the nail phalanges of the toes. But in the future, the entire foot may turn pale. This process is often accompanied by a feeling of numbness, as well as other unpleasant sensations: burning, tingling, distension. In some cases, the pallor of limited areas of the skin of the leg is replaced by moderate cyanosis. These disorders are clearly identified after hypothermia, especially after work associated with high humidity.
Factors contributing to the occurrence of lumboischialgia
If a person is bothered by chronic vertebrogenic lumboischialgia, then diseases of various internal organs and the central nervous system are often detected. On the part of the central nervous system, these are, as a rule, residual effects of inflammatory and traumatic brain damage. Based on experimental studies, it has been established that the creation of additional foci of damage even outside the spine contributes to the occurrence of lumbar osteochondrosis. These lesions can be in the brain, muscles and internal organs. (V. P. Veselovsky)
Reflex curvature of the spine with lumboischialgia
In addition to pain and various autonomic disorders, patients with lumboischialgia often have reflex deformities of the lumbar spine. This manifestation is called antalgic scoliosis. It was believed that in most cases it was of a protective nature, as if helping to reduce irritation of the sinuvertebral nerve.
However, quite often, especially in young people, these curvatures remain for a long time, even after a significant reduction in pain. Therefore, reflex deformation of the spine cannot be considered as a physiologically useful mechanism. And also consider that this mechanism is aimed at reducing irritation of sensitive nerve formations, which are the source of pain. It would be more correct to say that there is vertebrogenic lumboischialgia with reflex muscular-tonic syndrome.
Treatment of lumboischialgia
Before talking about how lumbar sciatica is treated, it is important to note that drug treatment, physiotherapeutic procedures, and exercises for lumbar sciatica are best determined individually. And you need to proceed from the characteristics of each specific case and stage of the process.
- To relieve pain, drug therapy and physiotherapy are prescribed. If there are indications, then medical therapeutic blockades are used. They are performed by a doctor. The medicine is injected paravertebrally, as well as into trigger points on the sore leg. As a rule, droppers with decongestants and anti-inflammatory drugs are prescribed.
- It is recommended to fix the lumbar spine using an orthopedic semi-rigid dynamic corset. This also helps reduce pain, because it reduces the load on the spine.
- Functional disorders (blocks) in the functioning of the spine must be identified. This is done by a chiropractor. And this is necessary because it is the incorrect functioning of the spine that leads to the development of osteochondrosis, and ultimately to the appearance of protrusions and herniations of intervertebral discs. First, manual diagnosis is performed, and then manual therapy. Typically, there are an average of seven to ten procedures per course.
- In order to stimulate recovery processes, physiotherapeutic procedures, reflexology, and massage are prescribed.
- Physical therapy is very important.
Sciatica syndrome, sciatica treatment, sciatica syndrome
Sciatica (sciatica) is pain in the lower back, spreading along the back of the thigh to the lower leg and foot. Typically, the cause of sciatica is a degenerative change in the intervertebral disc, which prolapses sideways, compressing the lower lumbar or upper sacral spinal nerve roots. Pain may develop suddenly during unsuccessful lifting of an object or turning of the torso. The back becomes extremely painful, and its mobility decreases significantly. A person may experience a feeling of numbness and weakness in the leg. Often, with strict adherence to bed rest, the pain gradually subsides, but in some cases there is a need for surgical intervention.
6 main causes of sciatica Various diseases of the lumbar spine can cause sciatica. Sciatica is often described as mild to intense pain in the legs. It is caused by compression of one or more of the five pairs of nerve roots in the lumbar spine. Sometimes doctors call sciatica radiculopathy. Radiculopathy is the medical term used to describe pain, numbness, tingling and weakness in the arms or legs caused by nerve root problems. If the nerve problem is in the cervical region, the condition is called cervical radiculopathy. Since sciatica affects the lumbar region, it is also called lumbar radiculopathy.
The causes of pain of the 5 pairs of nerve roots in the lumbosacral region are combined with the creation of the sciatic nerve. Beginning at the back of the pelvis (sacrum), the sciatic nerve travels behind the buttocks and down through the hip joint into the lower extremities. Nerve roots are not separate structures, but part of the body's overall nervous system, capable of transmitting pain and sensations to other parts of the body. Radiculopathy is caused by compression of the nerve root by a ruptured disc or bone growth in the space before it connects to the sciatic nerve.
Sciatic Nerve Compression Certain types of spinal disorders can cause spinal nerve compression and sciatica or lumbar radiculopathy. The 6 most common ones are listed below: disc herniation; lumbar spinal stenosis; spondylolisthesis; injury; piriformis syndrome; spinal tumors.
Sciatica or sciatica syndrome is lumbosacral radiculitis with a predominance of damage to the roots of the sacral region, from which the sciatic nerve is formed. The main symptom of sciatica is a shooting pain along the sciatic nerve from the lower back to the buttocks and moving down to the back of the legs (usually just one leg). This pain may be mild or severe and may be uncomfortable and may worsen if you sit for long periods of time.
Other common symptoms of sciatica include: Numbness in the leg along a nerve – this numbness in one part of the leg may be accompanied by pain in various other parts of the leg; tingling sensation in the legs and fingers.
If the symptoms of sciatica are mild and do not last longer than four to eight weeks, then you most likely have acute sciatica and medical examination is not necessary, as it usually goes away on its own. A complete medical history can help make a diagnosis.
The doctor will ask you to do certain exercises that stretch the sciatic nerve and will pay close attention to your legs. Shooting pain in the lower leg during these exercises usually indicates sciatica. If the pain persists for more than four to eight weeks, then tests such as X-rays or MRI may be needed to determine the cause of the pinched sciatic nerve and sciatica.
Treatment of sciatica
Most cases of acute sciatica are prevented by self-medication. It is possible to use painkillers that relieve pain symptoms - non-steroidal anti-inflammatory drugs (such as ibuprofen or paracetamol are recommended). But not all painkillers are suitable for every patient; you should definitely consult your doctor.
Exercises such as walking or gentle stretching exercises are recommended. Hot or cold compresses can help relieve pain, especially if you alternate them. When treating chronic sciatica, a combination of self-medication and physical therapy is usually used.
Painkillers are prescribed - amitriptyline, codeine, most often in combination with paracetamol, and if the symptoms of sciatica are severe, then diazepam is used. Physical therapy can help strengthen muscles and improve their elasticity to reduce sciatica symptoms.
Cognitive behavioral therapy helps treat chronic sciatica by teaching people to respond to pain differently. If symptoms do not respond to treatment and continue to worsen, then surgery may be necessary. Surgical options include: lumbar laminectomy relieves pressure on nerves; dysectomy - partial or complete removal of a damaged disc.
buttocks along the back or outer surface of the leg. Pain can have both myofascial and neurological origin. The source of sciatica may be myofascial TP in the posterior part of the gluteus minimus muscle. This source of pain can be easily overlooked if muscle testing is not done. As a rule, the cause of sciatica is considered to be nerve compression. The most common occurrence is entrapment of the sciatic nerve and/or posterior cutaneous nerve of the thigh by the piriformis muscle at the site where the nerve exits through the greater sciatic foramen.
Other neurogenic causes of sciatica include compression of the nerve root due to a tumor, spinal stenosis, or, in rare cases, the presence of fascicular bundles. In addition, sciatica is caused by compression of the cauda equina by a herniated disc in the lumbar spine (radiculopathy). The cause of compression and pain may be an aneurysm. Negrin and Fardin published long-term results of observation of 141 patients with acute sciatica and EMG signs of monoradicular denervation. Of these, 19 patients underwent surgical treatment, and 22 received conservative treatment.
After 3-8 years, in operated patients with initially severe movement disorders, complete recovery was noted in 33% of cases and a significant improvement in motor functions was noted in 30% of cases. In the group of patients receiving conservative treatment, the initial muscle weakness remained almost at the same level. However, there were no significant differences in the disappearance of pain between the two groups. Patients paid more attention to pain rather than to movement disorders. In these patients, pain was caused as much by TT or other muscular or fascial lesions as by nerve compression. Sheon et al suggest that in the absence of sensory and motor disorders, it is more correct to use the term “pseudo-sciatica” rather than *sciatica.” In such cases, the causes of symptoms appear to be bursitis and myofascial pain. As mentioned in Section 1, Kellgren found that in 50 of 70 cases of sciatica, the pain was due to ligament or muscle damage. Other authors have noted that in many patients with suspected sciatica in the absence of neurological symptoms, the pain is most likely of myofascial origin.
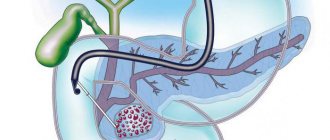
Disc protrusion or herniation Disc protrusion is a condition when the central gel-like part of the disc (nucleus pulposus) protrudes towards the spinal canal, without compromising the integrity of the outer wall of the disc (annulus fibrosus). A disc herniation occurs when the nucleus pulposus extends beyond the annulus fibrosus. With protrusion or herniation of the disc, the protruding part of the disc can compress the adjacent nerve root and cause sciatica. The consequences of a herniated disc are worse. In this case, the prolapsed disc core not only causes direct compression of the nerve root, but at the same time the disc substance contains an acid, a chemical irritant (hyaluronic acid), which causes inflammation of the nerve. Nerve compression and irritation cause inflammation and pain, often leading to limb numbness, tingling, and muscle weakness.
Lumbar spinal stenosis Spinal stenosis manifests itself as compression of the nerve and most often affects people of mature age. Pain in the lower extremities, similar to sciatica, may be the result of spinal stenosis of the lumbar spine. The pain is usually positional, occurring with changes in body position, standing or walking, and relieved by sitting. The nerve roots branch from the spinal cord and exit through the foramen, bounded by bones and ligaments. Nerve roots emerge from these foramina and innervate other parts of the body. When these openings become narrow and cause compression of the nerve, the term foraminal stenosis is used.
Spondylolisthesis Spondylolisthesis most often affects the lumbar spine. In this case, the overlying vertebra is displaced in relation to the underlying one. When a vertebra slips and becomes displaced, a nerve root is pinched, causing sciatica pain in the legs. Spondylolisthesis is divided into congenital and acquired (due to degenerative changes, trauma, physical activity or heavy lifting.
The injury Sciatica may result from direct nerve root compression caused by external forces on the lumbosacral spine. For example, in case of a road traffic injury, fall, etc. This impact can damage nerves when broken bone fragments cause nerve compression.
Piriformis syndrome This syndrome is named after the piriformis muscle and pain is caused when this muscle irritates the sciatic nerve. The piriformis muscle is localized in the pelvic region, connects the femur and is involved in hip rotation. The sciatic nerve passes under the piriformis muscle. Piriformis syndrome occurs when this muscle spasms, thereby compressing the sciatic nerve. Due to the insufficient information content of X-rays and magnetic resonance imaging, diagnosing this pathology is difficult.
Spinal tumors Spinal tumors are characterized by pathological tissue growth and are divided into benign and malignant. The occurrence of spinal tumors is quite rare. However, with the development of a tumor of the lumbar spine, there is a risk of developing sciatica due to compression of the nerve root.
Treatment of sciatica To create a treatment plan, a diagnosis is necessary, including a neurological examination, x-ray and magnetic resonance imaging. Depending on the cause of sciatica, there are several treatment options. Conservative therapy includes changes in activity, physical therapy, anti-inflammatory therapy and various types of blockade to relieve inflammation of the nerve root. Surgical treatment includes removal of the disc herniation through a small incision (microdiscectomy), and in case of stenosis, decompressive surgery with partial or complete removal of the vertebral arch (laminectomy).
The importance of physical therapy
Gymnastics for lumboischialgia should initially be aimed at eliminating muscle spasms. Equally - to relieve muscle swelling and venous stagnation in them and the roots of the intervertebral foramina. Ultimately, the goal of therapeutic exercise is to optimize the movement pattern. In other words, it is necessary to make the spine work more correctly, without overloading any of its segments. This is necessary to ensure that the disks do not fail prematurely. And new hernia protrusions did not appear in them, and old ones did not increase. All physical therapy should be built taking into account the individual characteristics of the patient. This is posture, features of the location of hernias and protrusions of intervertebral discs. Physical therapy exercises in combination with manual therapy are not only the prevention of relapses in chronic vertebrogenic lumbodynia. They are a prevention of the degenerative-dystrophic process (osteochondrosis of the spine), as such.
Treatment at the Energy of Health clinic
If you are faced with a pinched sciatic nerve, the doctors at the Health Energy clinic will come to your aid. We will conduct a comprehensive diagnosis in the neurology department to accurately identify the cause of the pathology and offer comprehensive treatment. At your service:
- modern medication regimens that take into account not only the level of pain and type of pinching, but also the individual characteristics of the body;
- drug blockades for quick pain relief;
- physiotherapy, exercise therapy, manual therapy and massage after relieving an exacerbation.
If necessary, we will organize sanatorium-resort treatment for you, which will prevent new attacks of pain. Regular monitoring by our specialists will make it possible to keep all chronic diseases under control.
Impact of comorbidities
With the development of osteochondrosis, the formation of protrusions and hernias of the spine, concomitant diseases play an important role. This is, first of all, endocrine pathology: diseases of the thyroid and parathyroid glands, adrenal glands, as well as progressive diabetes mellitus. With lumbago, as a particular manifestation of osteochondrosis, it is necessary to check the condition of the kidneys. To do this, you need to perform an ultrasound of the kidneys, do a general blood and urine test.
The syndrome of chronic lumboischialgia is, as a rule, persistent. Constant pain in the lower back significantly limits the ability to work, if not completely deprives it. To prevent this from happening, treatment should begin as early as possible. Moreover, treatment measures must be comprehensive and the entire treatment process must be carried out under the supervision of a doctor.
How to find out if leg pain is sciatica
If you are not sure that the pain in your leg is caused by sciatica, schedule a consultation with a rehabilitation specialist.
He will review your medical history and conduct a clinical examination. X-rays, MRIs, CT scans, and in some cases electromyography (EMG) can help determine the source of the pain.
Conservative treatment, including physiotherapy and hydrotherapy, which takes place in Evexia, is the first step towards your recovery.
Dr. Kandilakis explains that surgical treatment is rarely used except for problems in the bowel and bladder, which contribute to increased pain and weakness.