Craniopharyngioma is a rare type of brain tumor. It is localized in the pituitary gland. It is mainly first diagnosed in children aged 5-14 years or in adults over 40. The survival rate for craniopharyngioma for 10 years is about 90%. For a long time, the neoplasm does not manifest itself with any symptoms, but over time, multiple abnormalities develop: endocrinological, visual, hormonal.
Reasons for development
Craniopharyngioma develops due to excessive proliferation of epithelial cells in Rathke's pouch. It is formed in the fetus in the first trimester of pregnancy and is the basis for the future pituitary gland. If development occurs normally, then after the formation of the pituitary gland, Rathke cells are no longer produced. Craniopharyngioma appears only if this tissue continues to divide.
Typically, pituitary craniopharyngioma occurs due to a hereditary predisposition. A mutation of chromosomes occurs, which leads to the formation of a tumor. It can also occur due to intrauterine development disorders in the first trimester of pregnancy - this is when all the fetal organs are formed. This can be affected by taking medications, exposure to radiation, poisons and toxins.
Intrauterine infection and early severe toxicosis significantly increases the likelihood of craniopharyngioma. Chronic diseases of the mother, such as kidney pathologies, diabetes mellitus or tuberculosis, can contribute to the development of a tumor in a child.
Craniopharyngioma in children
Craniopharyngioma is uncommon in children. It is diagnosed in only 4% of all brain tumors. Typically, the first signs of the disease are diagnosed at the age of 5-14 years; craniopharyngioma occurs equally often in boys and girls. Initially, the pathology does not manifest itself with any obvious signs. Over time, the patient begins to complain of the following symptoms:
- Frequent headaches, worse in the morning;
- Nausea and vomiting;
- Delayed sexual and physical development;
- Violation of hormonal and endocrine functions;
- Change in behavior;
- Confusion;
- Visual impairment;
- Decreased appetite, increased thirst;
- Impaired motor functions;
- Increasing epilepsy;
- Swelling of the fundus;
- Altered psychopathological state.
Depending on the location of the tumor and its size, the manifestations of the disease may vary. It is important for parents to monitor the condition of their child, because timely diagnosed craniopharyngioma responds well to treatment.
Craniopharyngioma in adults
Craniopharyngioma is a benign tumor in the brain. Usually it begins during embryonic development and is localized in the hypothalamic-pituitary region. Due to the growth of the tumor, numerous cysts often form, inside which fluid from proteins and cholesterol accumulates. In this case, the papillary form of craniopharyngioma is mainly diagnosed in adults.
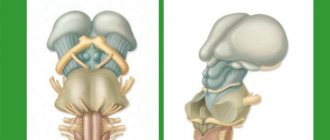
Suprasellar and intrasuprasellar craniopharyngioma
The initial classification of craniopharyngiomas was developed by V. Grekhov at the Institute of Neurosurgery named after. Burdenko. In the future, it was repeatedly detailed and changed. Today it is customary to distinguish the following topographic variants of craniopharyngiomas:
- Suprasellar
. Such tumors grow within the sella turcica, displacing the diaphragm. They can spread supra- and parasellar. The neoplasm develops from the remnants of the epithelium, which is preserved at the level of the pituitary gland; - Stem
. They spread in the area of the pituitary gland stalk, gradually affecting the bottom of the 3rd ventricle. They are localized above the sella turcica, displacing its diaphragm down; - Intra-extraventicular
. They develop at the level of the pituitary infundibulum and spread into the cavity of the third ventricle. This type of craniopharyngioma is associated with the accumulation of embryonic epithelium in the infundibulum area.
Adamantimatous and papillary craniopharyngioma
Craniopharyngiomas vary in structure. They may contain cysts or consist of dense tissue. Cystic formations are characterized by slow growth, extremely rarely their diameter exceeds 5 centimeters. Typically, such tumors have up to 50 cysts, in rare cases their number reaches 200. The formation itself is dense, with a strong capsule, and quickly connects with brain tissue and blood vessels.
NB!
Under the influence of various factors, the tissue structure of craniopharyngioma can change.
If craniopharyngioma has been present in the body for a long time, there is a risk of necrosis. This contributes to the rapid formation of cysts. Inside they are filled with liquid with a high lipid content. Craniopharyngiomas can vary in cytological structure. The following types of such tumors are distinguished:
- Adamantine-like
. Occurs in most cases. Mostly diagnosed in children. A neoplasm of this type consists of remnants of embryonic tissue. They mainly consist of cysts. Adamantine-like craniopharyngiomas are characterized by polymorphism; - Papillary
. It is mainly diagnosed in people over 40 years of age, and practically never occurs in children. Such a tumor consists of metaplastic cells, with virtually no fossilization. Papillary craniopharyngiomas can consist not only of epithelial but also epidermal cells. In such tumors, degenerative processes occur and cysts and stroma develop.
Craniopharyngioma
Craniopharyngioma is a histologically benign extra-axial slow-growing tumor that is localized primarily in the sellar and suprasellar regions.
Despite the benign histological characteristics, sometimes the manifestations of craniopharyngioma are similar to malignant tumors. Craniopharyngiomas can metastasize, and patients may have severe symptoms that usually require surgery or radiation (and in some cases intracystic chemotherapy). Cases of recurrence, both local and with metastasis along the meningeal membranes and along the surgical approach, have been described. Typical radiological findings can help in the differential diagnosis of craniopharyngiomas and other tumors of the chiasmal-sellar region. Craniopharyngioma was first described by Zenker in 1857. [1, 2, 3, 4, 5]
Epidemiology
Although craniopharyngiomas occur at any age, there are two peaks of incidence: at the age of 10-14 years, the highest incidence of the adamantinomatous type of craniopharyngiomas occurs, the second, smaller one, in people over 50 years of age, is mainly the papillary subtype.
Clinic
The clinical picture depends on the location and size of the tumor and includes:
- headaches and increased intracranial pressure
- visual impairment in 20% of children
- 80% in adults
Pathology
Currently, it is believed that craniopharyngiomas originate from Rathke's pouch and not from the crest cells of the craniopharyngeal duct, as previously believed. Histologically, two subtypes are distinguished, which also differ in their characteristic visualization.
Adamantinomatous subtype
- mainly in children
- contain reticular epithelial cells (resembling the enamel pulp of developing teeth)
- may have one or more cysts filled with an oily fluid rich in proteins, breakdown products of hemoglobin, and/or cholesterol
May contain single or multiple cysts filled with contents rich in proteins, breakdown products of hemoglobin and/or cholesterol. Calcifications occur in ~90% 3.
Papillary subtype
The papillary subtype occurs almost exclusively in adults and is formed by masses of metaplastic squamous cells. Cysts are less characteristic, and the tumor is more solid. Calcification is considered rare.
Diagnostics
In the vast majority of cases, craniopharyngiomas have a large suprasellar component (95%) with suprasellar and intrasellar distribution (75%). Large tumors spread in all directions, often causing displacement of the chiasm or compression of the midbrain, ultimately leading to compressive hydrocephalus.
Choosing a modality
CT and MRI are the modalities of choice. [6, 7] Computed tomography can reliably detect the presence of calcifications and determine the size of the tumor, while MRI is extremely good at not only determining the size, but also assessing the spread of the tumor and the degree of damage to the third ventricle. MRI can confirm the cystic nature of the tumor. Fluid-attenuated (FLAIR), gradient echo (GRE), and diffusion-weighted imaging sequences, along with MR spectroscopy, can be used to confirm or correct the diagnosis [8, 9, 10]. X-rays can reveal changes, however, despite the changes detected, CT or MRI will be necessary. CT or MR angiography can help in the differential diagnosis between craniopharyngioma and anterior communicating artery aneurysm. In the postoperative period, CT and MRI are performed to obtain initial results necessary for subsequent dynamic observation [11, 12, 13, 14, 15, 16, 17, 18, 19, 20]. In the absence of typical signs of MR, the study should be supplemented with non-enhanced CT to detect calcifications. Papillary lesions may be missed on CT or MRI unless there is a characteristic cystic component or the lesion does not enhance after intravenous contrast (which occurs in approximately 10% of patients).
CT scan
On computed tomography, the adamantinomatous tumor type appears as a predominantly cystic tumor with a solid component (in 90% of cases). The solid component has an isodense density and usually contains calcifications (in 80% of cases). An increase in the size of the sella turcica may be observed. Depending on the location of the tumor, hydrocephalus may occur. The location of the tumor in the sellar or suprasellar region in this type is a characteristic feature of the tumor.
Tumors of the papillary type are usually solid, isodense, and rarely contain calcifications. Sometimes with craniopharyngioma there is an intraventricular homogeneous soft tissue component without calcifications [14].
Contrast enhancement of the solid component and cyst walls occurs in 90% of cases. Displacement of the A1 segment of the anterior cerebral artery or optic chiasm may be visualized. The cystic component extends anteriorly and/or laterally and usually surrounds the solid component. The solid component, on the contrary, extends laterally and posteriorly.
The degree of reliability for CT is high, since CT can detect calcifications and determine the cystic nature of the tumor: for example, Rathke's pouch cysts rarely calcify, while more than 90% of craniopharyngiomas contain calcifications.
Key points:
- Adamantinomatous subtype of cysts are close in density to cerebrospinal fluid
- are large in size
- dominate over the solid component
- occur in 90% of cases
- soft tissue density
- determined in 90%
- small cysts
- soft tissue density
- are rare
Magnetic resonance imaging
The adamantinomatous type is a predominantly suprasellar tumor with a cystic component. Calcifications may not be visualized on MRI, but granite echo (GRE) sequences, due to the magnetic susceptibility effect, may allow their visualization. The cystic component has a hyperintense MR signal on T2WI and FLAIR, and a heterogeneous iso- or hypointense MR signal from the solid component [12, 14, 16, 18, 22, 8]
The change in MR signal intensity on T1-weighted images varies depending on the cystic content, which can give a hyperintense signal when the content is rich in proteins, hemoglobin breakdown products and/or cholesterol (in the classic adamantinomatous type). In the capillary type, the solid component is characterized by an isointense MR signal on T1-weighted images. .
MR spectroscopy is characterized by an increased peak of the lipid spectrum (about 1 ppm) in the cystic contents. Diffusion-weighted images are characterized by variable MR signal intensity due to cystic content.
Remodeling and increase in the size of the sella turcica and hydrocephalus may occur. The presence of compression of the third ventricle makes it possible to differentiate craniopharyngioma from Rathke's pouch cyst or pituitary adenoma. Sometimes craniopharyngioma appears as an intraventricular, homogeneous, soft tissue tumor without calcifications. It may contain areas of low MR signal intensity, as observed in the papillary subtype.
Sometimes craniopharyngiomas have both an intra- and suprasellar component, which is manifested by the “snowman” sign [8]. Adjacent brain parenchyma may have increased MR signal on T2/FLAIR-weighted images, which may indicate compression edema, gliosis, or tumor invasion. Recurrence of the tumor in the bed and along the surgical approach is the result of implantation of craniopharyngioma into the tissue. Thus, postoperative MRI is necessary even if the tumor was completely removed [18, 8].
Key points:
- Adamantinomatous subtype T1 are iso- or hyperintense to the brain parenchyma
- T2 in 80% hyperintense
- has a pronounced contrast enhancement
- sequences with magnetic susceptibility are required
- displacement of the ACA and/or chiasm
- high lipid peak
- T1 hypointense
- T1 iso- or slightly hypointense signal
- cyst contents do not have a high lipid peak
Differential diagnosis
- Astrocytoma/glioma of the hypothalamus or optic nerve is usually solid with areas of necrosis
- rarely calcifies
- pronounced contrast enhancement
- rarely calcifies
- minimal contrast enhancement
- contains fat
- does not have a solid component
- microadenoma is rare in children
- rarely calcifies
- has a dural tail sign
Symptoms
Craniopharyngioma of the pituitary gland is characterized by the development of endocrine and metabolic disorders, and intracranial hypertension syndrome. Because of this tumor, the balance of many hormones in the body is disrupted: gonadotropin, LH, ACTH, STH. This leads to the development of hypothyroidism, hypogonadism, hypocortisolism, and diabetes insipidus. Over time, hypothalamic-pituitary disorders occur, such as:
- Constant feeling of thirst;
- Polyuria, enuresis;
- Developmental delays, decreased growth rates in children;
- Rapid increase in body weight;
- Increased fatigue, muscle weakness;
- Menstruation irregularities, decreased libido.
The severity of such deviations depends on the location of the craniopharyngioma, its size and the age of the patient. Early symptoms of a tumor also include visual disturbances: decreased visual acuity, development of blindness. If the tumor is located in the third ventricle and compresses its openings, intracranial pressure increases - the patient complains of a constant headache.
NB!
The intensity of manifestation of pituitary craniopharyngioma depends not only on the size and location of the tumor. If the tumor is large, but it does not compress neighboring areas, the symptoms of the pathology may be minor.
2. Symptoms of the disease
The symptomatic picture is determined by the characteristics of the tumor localization, namely their close proximity to the pituitary gland and hypothalamus, optic nerves and chiasm, as well as to the pathways of cerebrospinal fluid movement. Neoplasms can be asymptomatic for a long time, appearing most often when the patient is between ten and twenty years old. The main symptoms of a tumor are:
- diabetes insipidus;
- the lag of the patient’s actual growth from the passport height;
- visual disturbances (up to complete loss of vision);
- hydrocephalus (headaches, nausea, vomiting);
- mental and personality disorders;
- obesity.
Visit our Neurosurgery page
Diagnostics
To diagnose craniopharyngioma, several studies are performed at once. This helps determine the possible cause of the pathology, its exact location, and the degree of damage to surrounding tissues. Standard diagnosis of craniopharyngioma includes the following measures:
- Anamnesis collection, visual examination of the patient
. The doctor will learn about the symptoms that concern the person, clarify the general state of health, and the presence of risk factors; - Biochemical and general blood tests
. Determine the concentration of vital blood components; - General urine analysis
. Determines kidney function, rate of urine excretion; - Hormonal blood test
. Determines the content of biochemically active substances and identifies deviations from the norm. The test allows you to diagnose endocrine disorders; - Neurological examination
. The function of the brain, spinal cord, and nerve endings is assessed. The doctor needs to check the person’s muscle strength, memory, vision, hearing, reflexes, and coordination; - CT and MRI
. Diagnostic imaging techniques that provide accurate images of the brain. This helps determine the size and location of the tumor and what tissues it has affected. MRI when determining pituitary craniopharyngioma gives a clearer picture; - Biopsy
. The most accurate examination method for craniopharyngioma. A portion of the tumor is removed using a needle for further histological examination. This determines the exact nature of the tissues.
NB!
When diagnosing pituitary craniopharyngioma, blood and urine tests are of high diagnostic value. Your doctor will need to check your electrolyte levels to help diagnose diabetes insipidus. It is also necessary to exclude germ cell tumors, for which the levels of alpha-fetoprotein (α-FP) and beta human chorionic gonadotropin (β-hCG) are determined.
Treatment
The basic treatment for pituitary craniopharyngioma is chemotherapy. It is carried out both as the main part of therapy and as an auxiliary part during surgical excision of the tumor. The radioactive drug is injected intravenously or into the spinal canal (in the case of surgical removal of a tumor, in its bed). Craniopharyngiomas cysts are filled with interferon preparations: they have a cytotoxic effect. Due to this, the process of self-destruction of tumor cells is started.
Craniopharyngiomas are prone to recurrence. And even after surgical interventions, many patients may develop a new formation within the first year. Because of this, they always undergo postoperative radiation therapy, which reduces the risk of such a consequence by 2 times. Today, the following methods show the greatest effectiveness in the treatment of pituitary craniopharyngiomas:
- Proton therapy
. Heavily charged particles are used that release all the energy into the tumor. Due to such targeted irradiation, it is possible to stop the growth of the tumor and also destroy some of the cells. The advantage of this technique is its highly precise action: the surrounding brain tissue is not irradiated; - Intracavitary radiotherapy
. This is one of the methods of radiotherapy in which the radiation source is located directly in the tumor. This avoids damage to the cranial nerves, blood vessels, pituitary gland and hypothalamus.
Therapy for pituitary craniopharyngioma in children
If pituitary craniopharyngioma is detected in children under 3 years of age, and the tumor is accompanied by the spread of numerous cysts, then a catheter is implanted in the pituitary gland area. Drainage of the cyst is organized, due to which its size is reduced. Nearby tissues and blood vessels are no longer compressed, and the symptoms of the pathology disappear.
Cyst catheterization is a minimally invasive method for treating pituitary craniopharyngioma. To increase the accuracy of the intervention, stereotactic settings are used. To remove cysts, a sclerosing agent may be injected into them. The walls of the tumor stick together, the tumor stops accumulating fluid. This technique is used exclusively in young children; in the future, more radical intervention is necessary: radiation therapy or surgical excision.
In older children, craniopharyngiomas are removed with a gamma knife. This is one of the methods of stereotactic radiosurgery, characterized by extreme targeting accuracy. High-dose radiation therapy is performed to remove the tumor. In this case, the surrounding tissues are not affected.
Types of operations to remove craniopharyngioma
Surgical treatment is the most effective method of treating cerebral craniopharyngioma
. The operation is quite complex: it has technical difficulties due to limited accessibility to the tumor. There is also a risk of damage to the pituitary gland, optic nerves, carotid arteries, and the floor of the third ventricle - all of these tissues are located in close proximity. The surgeon needs to remove all tumor tissue and not affect healthy cavities.
Radical tumor removal reduces the risk of relapse by up to 20%. In the future, postoperative radiation therapy can minimize the likelihood of future tumors. Currently, the following surgical techniques are used for pituitary craniopharyngioma:
- Surgery with craniotomy access with traditional opening of the cranial bones
. All manipulations are determined in advance using computer planning. This allows the operation to be performed as carefully as possible, preserving all surrounding tissues and formations; - Operation with transsphenoidal approach
. This is an endoscopic type of intervention. Small incisions are made under the nose and sinuses of the sphenoid bones, through which a neuroendoscope is inserted into the brain cavity. This minimally invasive intervention is easier for patients to tolerate and the rehabilitation period is shortened. But it must be taken into account that not all craniopharyngiomas are suitable for such an operation. Interventions with a transsphenoidal approach are performed only when the tumor is located suprasellar.
Treatment of brain craniopharyngioma
Treatment of craniopharyngiomas consists of radical removal of pathological foci. Much depends on the location of the tumor, so the choice of treatment tactics depends on the individual characteristics of the patient’s diagnosis. The type of access is selected based on diagnosis and depends on the subtype of the tumor and its topographic and anatomical features. The main goal of surgical treatment is complete (total) removal of brain craniopharyngioma, but not in all cases the craniopharyngioma can be completely excised (subtotal excision).
Total removal of the tumor is called surgical treatment when no remnants of neoplasia are detected during a repeat control examination. Subtotal removal is considered a radical treatment in which it is impossible to remove the tumor completely or, after removal, parts of pathological tissue remain in the brain tissue. As a rule, with subtotal removal, the doctor is forced to leave parts of the neoplasia near the bottom of the third ventricle of the brain, on large vessels and other vital elements.
After removal
After removal of a brain craniopharyngioma, conservative treatment is carried out in the form of radiotherapy and chemotherapy, because treatment should always be comprehensive, which improves the overall outcome of therapy.
Radiation therapy is an auxiliary treatment. It is prescribed in the postoperative period or in the presence of relapses of neoplasia. Radiation has a number of side effects, for example, as a result of radiation treatment, mental development may suffer, endocrine pathologies may increase, vision problems, dementia and other negative phenomena may occur.
Chemotherapy consists of prescribing cytostatic drugs to stop protein synthesis in atypical cells, and some of them die. After tumor removal, the patient may be prescribed glucocorticoids. Treatment with them helps reduce negative signs and swelling. As the condition improves, they are gradually canceled.
Postoperative changes after removal of craniopharyngioma
Almost all patients with craniopharyngioma experience complications that impair quality of life. Such consequences can arise either due to the tumor itself or as a result of treatment. Patients often encounter the following problems:
- Loss of vision;
- The appearance of mood swings;
- Emotional disorders;
- Memory impairment;
- Endocrine dysfunction;
- Development of metabolic syndrome;
- Pathologies of blood vessels.
The pituitary gland is the main gland in the human body. It is she who is responsible for the production of basic hormones, and also controls the work of other organs and endocrine glands. If a person's pituitary gland function is impaired, multiple problems arise: obesity, decreased bone mineral density, deterioration of the lipid profile, decreased fertility. This often occurs even in those patients who adhere to hormone replacement therapy.
Due to damage to the hypothalamus, multiple hormonal changes also occur. And this affects the quality of life. The patient begins to complain of increased appetite, his body weight rapidly increases, his behavior changes, and his personality becomes emotional. Metabolic syndrome often develops - a group of disorders accompanied by obesity, elevated levels of triglycerides and cholesterol, and high blood pressure. Metabolic syndrome significantly increases the likelihood of strokes and heart attacks.
In most cases, treatment for pituitary craniopharyngioma requires surgery or radiation therapy. After such events, the likelihood of disorders of the blood vessels of the brain increases significantly. The risk of aneurysms and stroke increases, seizures and cognitive impairment often occur.
Due to the high risk of complications associated with pituitary craniopharyngioma, the patient must be under constant medical supervision. Only timely diagnosis will make it possible to identify the deviation at the initial stages and stop it. Social and psychological assistance will help improve the patient's condition. The specialist will tell the person how to competently cope with the experience, how to get rid of anxiety and minimize the risk of depression.
4. Treatment of craniopharyngiomas
The method of treating benign brain tumors is predominantly surgical
. The choice of surgical method depends on many factors, including the nature, size, localization of the tumor, its proximity to vital centers of the brain, etc. The neurosurgeon always strives for complete removal of craniopharyngioma, but the proximity of the tumor to the visual centers and large arteries does not always provide such an opportunity - sometimes it is simply technically impossible.
For endosellar craniopharyngiomas, a transsphenoidal method of surgical intervention
. The essence of this method is endoscopic access to the brain through the nasal passages and removal of the tumor in a gentle manner, without making external incisions. Modern fiber optic equipment helps the operating surgeon make precise movements, controlling his actions using a monitor.
, radiation therapy and hormone replacement therapy can be used to increase the effectiveness of treatment
Prognosis and prevention
At the moment, doctors have not developed an unambiguous system for determining the stage of craniopharyngioma. The tumor can be newly diagnosed or recurrent. This is a benign neoplasm that is not prone to spreading to other parts of the brain. Despite this, they can cause numerous abnormalities in the body’s functioning: disruption of endocrine functions, damage to the optic nerve.
The 10-year survival rate for patients with pituitary craniopharyngioma is 90%. With adequate treatment, it is possible to preserve both the quality and life expectancy of the patient. If after radiation therapy the tumor continues to progress, they are completely removed.
It is impossible to completely protect yourself from pituitary craniopharyngioma. The disease has a hereditary predisposition. The only way to reduce the likelihood of developing pathology is to prevent the exacerbation of diseases in the mother during pregnancy, avoid self-medication with medications, and protect against the influence of toxins and poisons.
Craniopharyngioma: treatment
Despite the fact that this type of neoplasm is benign and transformation into malignant is extremely rare, its uncontrolled growth leads not only to a significant deterioration in the patient’s quality of life, but also to death. Therefore, when a craniopharyngioma is detected, surgery is scheduled to remove it as soon as possible. After surgery, the standard treatment for this nosology is various types of chemotherapy, including targeted chemotherapy. A specific treatment regimen is prescribed taking into account the clinical course of the disease, the patient’s age, especially if we are talking about a child, and other nuances. Radiation therapy (in standard modes), brachytherapy or other forms are also used. Optionally, stereotactic radiosurgery may be recommended. It is this technique that is implemented in the CyberKnife system used by the OncoStop Radiation Surgery Center. The device is adjusted to the affected tissues with an accuracy of fractions of a millimeter, without affecting healthy ones, due to which all brain functions are preserved to the maximum extent possible. The method is non-invasive, does not require anesthesia or a recovery period, and immediately after the procedure the patient can carry out everyday activities.
To clarify the possibility of using CyberKnife in a specific case and to sign up for a consultation, call +7 or 8 (800) 5-000-983.
conclusions
Craniopharyngioma is a benign neoplasm of the pituitary gland. Mostly occurs in children 5-14 years old. The disease develops due to disorders that occur in the fetus in the first trimester of pregnancy. In the initial stages, it is difficult to diagnose, because the pathology does not manifest itself with any symptoms for a long time. Treatment for pituitary craniopharyngioma is mainly surgical.
If you suspect pituitary craniopharyngioma in yourself or cannot recover from this disease, then feel free to contact the doctors of our medical center. They will conduct extensive diagnostics, develop an individual treatment regimen and monitor all stages of therapy.