What types of brain tumors are there?
Based on the primary site of occurrence , brain tumors are divided into:
- A primary brain tumor is one that arises directly from brain cells, its membranes, or cranial nerves.
- A secondary brain tumor is one that formed in some other organ (for example, the lung) and metastasized through the bloodstream to the brain.
According to histological properties , they are usually named according to the type of cell from which they develop:
- Neuroepithelial tumors – from the brain epithelium (astrocytoma, glioma);
- Meningeal - from the cells of the membranes of the brain (meningioma);
- Tumors of the cranial nerves – neuromas;
- Dysembryogenetic tumors develop due to disruption of the development of the neural tube in the prenatal period.
Are there any features of brain tumors?
Brain tumors are truly special, and the reason for this is the so-called blood-brain barrier (BBB).
The BBB is a physiological barrier between our blood and the cells of the nervous system. It is he who regulates the flow of various substances from our bloodstream into the cerebrospinal fluid and nervous tissue. This barrier protects our brain from microorganisms, toxins and, of course, cancer cells formed in other organs and metastasized to the brain. But it is the BBB that becomes an obstacle in the treatment of primary tumors, since it does not “let through” not only toxins, but also drugs.
Another characteristic of brain tumors is that sometimes benign tumors are as difficult to treat as malignant ones, depending on their size and location in the brain.
In addition, their peculiarity lies in the distribution by stages (more on this below, in the section “Brain cancer, stages” )
What are the causes of brain cancer?
Let’s not say anything new; the exact cause of brain cancer, like cancer of other organs, is not fully known. But with all types of cancer, there is a change in the most important macromolecule for humanity - DNA.
DNA is the macromolecule that makes up our genes. Namely, genes control the work of our cells - when to divide and when it is time for them to die.
A tumor is a collection of atypical (“bad”) cells that quickly divide and do not perform any functions.
There are two types of genes in the human body:
- Oncogenes - their activation “stimulates” cells to quickly divide and, as a result, a tumor forms.
- Tumor suppressor genes/antioncogenes are genes that, on the contrary, control cell proliferation, preventing them from dividing randomly.
Cancer occurs when oncogenes turn on and anti-oncogenes turn off.
According to epidemiological and experimental studies, there are several factors that play a significant role in the occurrence of brain tumors:
- Genetic - that is, if a parent has a DNA “breakage” with antioncogenes, then there is a risk of transmitting this DNA to the child;
- Environmental factors, in particular aromatic bicarbonates;
- Viruses;
- Radioactive agents;
- Biological – puberty or aging.
Brain cancer, stages
As mentioned earlier, one of the peculiarities of these tumors is that they are not divided into stages according to the generally accepted TNM system.
- T (tumor – tumor) – in the case of brain cancer, its size is not as important as its location and what it comes from;
- N (nodus – lymph node) – there are no lymphatic vessels in the brain;
- M (metastasis - metastases) - occur slowly and rarely.
Therefore, they are divided according to the WHO classification proposed in 2007 into four degrees of anaplasia. It is based on a combination of histological, genetic and patient survival data and includes four stages:
- Brain cancer, stage 1 – this includes neoplasms with low proliferative activity (divide slowly), they are treated surgically.
- Brain cancer, stage 2 – tumors are infiltrative in nature (grow into nearby tissues), have a low ability of cells to divide, and often recur.
- Brain cancer, stage 3 - the tumor grows quickly, spreads to nearby tissue, and the tumor cells are very different from normal cells.
- Brain cancer, stage 4 - defined as cytologically malignant, almost always recurs, has an unfavorable prognosis, and widely grows into adjacent brain tissue.
What are the symptoms of brain cancer?
Common signs of brain cancer. Any tumor formed in the brain puts pressure on the brain tissue, which causes increased intracranial pressure and contributes to the occurrence of the following symptoms:
- Headache, often of a bursting nature;
- Nausea, vomiting, which provides temporary relief;
- Double vision;
- Dizziness;
- Impaired consciousness;
- Hemiparesis (paralysis of the arm and leg on one side);
- Cramps.
Focal symptoms of brain cancer, depending on location:
- Ataxia (impaired coordination) in the limbs, tremor, nystagmus towards the affected side (cerebellar tumors)
- Violation of statics, muscle hypotonicity (tumors of the cerebellar vermis)
- Hearing impairment, motor coordination, paresis of facial muscles (tumors of the cerebellopontine angle)
- Swallowing disorders, tongue deviations, sensitivity disorders of the pharynx, face (trunk tumors)
Let's look at the symptoms of several common tumors:
Glioblastoma, signs (IV stage) . Glioblastoma is a malignant brain tumor that arises from astrocytes (the supporting cells of the nervous system). Clinical symptoms progress quickly, after 2-4 months general and focal symptoms are mixed, epileptic seizures and psychopathological personality changes are observed.
Sarcoma of the brain , formed from the connective tissue of the brain. Symptoms of brain sarcoma are similar to those of other brain tumors and may include:
- Headache;
- Nausea;
- Impaired consciousness;
- Mental changes;
- Convulsions; Speech disturbances.
Pituitary adenoma - most often develops from the anterior lobe of the pituitary gland and is characterized by hormonal disorders that lead to the following symptoms:
- Hypersecretion of adrenocorticotropic hormone - high blood pressure, increased blood glucose levels, stretch marks on the hips, amenorrhea in women, impotence in men, osteoporosis, increased male pattern hair growth.
- Hypersecretion of prolactin – amenorrhea in women, milk secretion in women, infertility in men.
- Hypersecretion of somatotropic hormone - an increase in the size of the limbs and tongue, increased sweating.
Discussion
In 90% of cases, SY occurs before the age of 20 years, with the peak incidence occurring between 5 and 13 years of age [8].
SY is rarely described in older patients. In a series of 14 observations described by K. Desai et al. [13], the youngest patient was 18 months old, the oldest was 40 years old. The average age of patients was 14.5 years, and in the vast majority of cases the disease manifested itself before the age of 30 years. In the literature [25], there is the only description of a case of SI of the skull in a 54-year-old patient. The disease is more often observed in male patients. According to the literature [8], the ratio of men to women is 1.6:1–1.8:1.
In our series, the male to female ratio was 1.2:1.
Primary SY most often affects the diaphysis of long bones (47%), pelvic bones (29%), ribs and vertebrae (12%). Cranial involvement in SY occurs with a frequency of 6 to 9%. The tumor most often affects the frontal and parietal bones. Less commonly, the pathological process involves the squama of the temporal bone and the mastoid process, the ethmoid bone, the orbit, and the pyramid of the temporal bone [1, 3, 7, 9].
Isolated cases of damage to the skull base by both primary ES and its metastases have been described. Since the beginning of the last century, only 36 cases of primary SI of the skull have been described. Of these, the base of the skull was affected in 13 (36.1%) cases [13]. In this group, damage to the temporal bone pyramid was observed in 6 cases, the orbit - in 4, the mastoid process - in 2, and the ethmoid bone - in 1 [13].
SY has a high tendency to metastasize. In 75-80% of cases, metastases appear within the first 2 years after detection of the primary tumor. They most often occur in the lungs (57%) and bones (34%) [24, 28]. Metastases to the central nervous system occur in 10–37% of cases [5, 13]. A. Colak et al. [5] reported 16% of cases of CNS metastases, most of which were spinal. A. Kulick and J. Mones [15] report 32% of cases of central nervous system damage and note that cerebral manifestation usually occurs within the first 2 years in 90% of patients.
Diagnosis of SJ of the skull base is complex. Anamnesis plays a key role in the differential diagnosis between primary and metastatic ES [4]. In all the described observations of metastatic lesions of the skull, there was a history of damage to one or another part of the body of the SC and the treatment performed [5].
There are no pathognomonic radiological signs to differentiate primary from metastatic ES [6]. Craniography and CT scanning of the skull reveal destruction of bone structures in the bone window [10]. Radiologically, the “onion skin” sign, characteristic of SI of long bones, is practically not observed in cases of damage to the skull [10, 11].
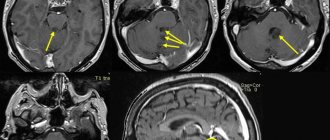
According to MRI, the tumors have a predominantly heterogeneous multinodular structure, contain many cysts, foci of hemorrhage and necrosis. The tissue is hyperintense relative to the brain and hypointense relative to the cerebrospinal fluid on T2 mode, hypointense relative to the brain and hyperintense relative to the cerebrospinal fluid on T1 mode. With intravenous contrast, the tumor inhomogeneously intensively accumulates the contrast agent [23].
The clinical picture is determined by the location and extent of the tumor and does not have much specificity, depending on whether the tumor is primary or metastatic [5, 6]. According to the literature [11, 13], if, with convexital localization of the tumor, symptoms such as headache (100%), increased intracranial pressure (75%), and swelling in the scalp come to the fore, then when the base of the skull is affected, the clinical picture appears mainly by damage to the cranial nerves. Damage to the pyramid is characterized by paresis of the facial nerve and hearing loss. When the tumor is localized in the area of the sphenoid bone, symptoms of damage to the oculomotor nerves and trigeminal nerve are noted. Rarely, when the tumor is localized in the posterior cranial fossa involving the condyle of the occipital bone and the jugular foramen, symptoms of damage to the caudal group of nerves are observed [24].
An accurate diagnosis is established on the basis of a pathological examination confirmed by the results of immunohistochemical and genetic studies [16].
Differential diagnosis should be carried out with intracranial tumors with round cells, such as primitive neuroectodermal tumor, rhabdomyosarcoma, metastatic neuroblastoma, lymphomas [10, 22].
The characteristic histological signs of SY are round cells arranged in the form of solid layers, scanty cytoplasm, protruding nuclei, lack of rosette formation, mitoses, and the presence of bone structures [13]. The patient's age and tumor location facilitate diagnosis. Immunohistochemical examination reveals the expression of vimentin and CD99 with characteristic membranous staining [19]. Studies reveal negative results regarding the expression of desmin, S-100 protein, chromogranin (neural marker), lymphoid markers CD20, CD3. SY differs from neuroblastoma, rhabdomyosarcoma, lymphoma, and others by the lack of expression of synaptophysin, desmin, leukocyte antigen, and other markers [12, 18].
Diagnostic and prognostically important factors are immunohistochemical and FISH studies that determine the translocation characteristic of SY [(t(11; 22) (q24; q12)] [12, 16].
Immunohistochemical study makes it possible to clarify the nature of the tumor; in all cases, expression of the CD99 protein was observed [2, 17].
It is important that primary and metastatic tumors practically do not differ in immunohistochemical parameters—expression of the same proteins was observed in both groups [15, 16].
However, there were indirect factors that distinguished primary tumors from metastatic ones. In metastatic tumors, a higher Ki-67 labeling index and a large number of mitoses are observed, which correlates with more aggressive and malignant tumor growth and a shorter life expectancy of patients compared to the group of primary SJ [12, 16].
Currently, combined treatment of both primary and metastatic ES is considered optimal [21].
The goal of neurosurgical intervention is to reduce the size of the tumor as much as possible.
In those described by K. Desai et al. [13] in 2000, 14 cases with primary skull tumor were subjected to subtotal tumor removal in 9 cases and total tumor removal in 5 cases. Recurrence occurred in only one case after total tumor removal. Therefore, tumor resection should be as radical as possible within acceptable safety limits [6].
The choice of surgical approach is mainly determined by the location of the tumor. If for convexital lesions only transcranial access is used, then for lesions of the base of the skull, especially with lesions of the chiasmal-sellar region, endoscopic transnasal interventions are possible [21].
Treatment for SY is multimodal; it involves maximal tumor removal followed by radiation therapy and chemotherapy [1, 24].
Radiation therapy is used after surgery as an adjuvant method for primary and metastatic tumors. The recommended radiation therapy regimen is 1.5–2 Gy/day, 5 days a week, with an SOD of 40–50 Gy [12].
Previously, when the only treatment options were surgery and radiation therapy, the prognosis for ES was unfavorable and the 5-year survival rate did not exceed 8–15% [8]. In 1974, Rosen introduced a combination of multimodal chemotherapy after surgery and radiation therapy. After this, the 5-year survival rate increased from 10 to 55-60%. Until 1990, round cell chemotherapy (RCT)-I was used, which consisted of 6 cycles of cisplastin with etoposide, vincristine, doxorubicin and cyclophosphamide given at 3-week intervals. After courses of chemotherapy, radiation therapy was performed with an SOD of 40–50 Gy. When using the RCT-I regimen, the 5-year survival rate was 20%. Since 1993, the RCT-II protocol has been used, which has increased the 5-year survival rate to 50%. This protocol consists of an induction phase of two cycles of iodophosphamide with etoposide and vincristine with doxorubicin and cyclophosphamide given at 3-week intervals. 8-9 weeks after completion of induction therapy, radiation therapy is used at a dose of 40-50 Gy. Maintenance chemotherapy consists of 6 cycles of vincristine, doxorubicin, cyclophosphamide and dactinomycin and is subsequently prescribed at 3-week intervals [1, 14, 25].
Prognostically, the most unfavorable factor in SY is the presence of distant metastases at the time of diagnosis [26]. Other unfavorable factors are the patient’s age over 10 years, tumor size greater than 200 ml, “median” lesion (for example, pelvis and spine), low efficiency of chemotherapy treatment [14].
Treatment outcomes for patients with SY improve over time. According to the Mayo Clinic, from 1950 to 1968, the 5-year survival rate was only 21.8% [15, 23]. According to data from 2000, the 5-year survival rate for SY in the same clinic reached 74%. Another large case series reported 50–80% 2-year disease-free survival after complex treatment [14].
Primary SI of the skull base has a more favorable course than metastatic tumor. Of the 14 patients, 8 (57.1%) lived more than 5 years. This is a good result compared to literature data. Patients with cranial metastases usually survive no more than 5 years, regardless of treatment methods [1].
Conclusion
At the base of the skull, both metastatic and primary SY occur with almost equal frequency. Primary tumors are typical before the age of 3 years, while metastatic lesions occur after 11 years. In all cases of metastasis to the base of the skull, there is anamnestic evidence of a primary tumor. The clinical picture consists mainly of symptoms of damage to the cranial nerves. There are no radiological pathognomonic signs that distinguish primary SY from metastatic one. On pathological examination, the only difference is a higher Ki-67 labeling index in metastases. Treatment for both primary and metastatic tumors is combined, carried out according to a single scheme and allows achieving relatively good results. The prognosis is more favorable for primary SY.
A comment
Being the second most common malignant tumor of the skeletal system, Ewing's sarcoma (ES) affects the skull bones in 9% of cases. In the practice of a neurosurgeon, it is extremely rare. Literature data on lesions of the skull with J are mainly limited to descriptions of isolated cases. It is known that SY has a fairly aggressive course and in 30% of cases manifests itself multicentrically.
This work is interesting in that it provides a detailed comparative analysis of metastatic and primary SJ of the skull base in patients operated on in the same clinic. It is part of the problem of skull base surgery. Despite the achievements of modern neurosurgery, it is not always possible to radically remove tumors of the skull base.
The authors analyzed 9 cases of SJ of the skull base, operated on at the Research Institute of Neurosurgery named after. acad. N.N. Burdenko. Moreover, in 5 cases the tumor was primary, in 4 cases it was of metastatic origin.
The issue of differential diagnosis of primary and metastatic SJ of the central nervous system is relevant from the point of view of prognosis of the disease, since it is known that the prognosis for metastases of SJ in the central nervous system with all treatment methods is not very favorable and the life expectancy of patients does not reach 5 years. In primary ES, the use of radiation therapy in combination with polychemotherapy can prolong the life of patients by more than 5 years.
The paper describes in detail the pathomorphology of tumors. The authors compared the morphological, immunohistochemical and genetic patterns of primary and metastatic tumors and showed their identity. No differences were found between the two categories, which, on the one hand, indicates the common genetic and pathomorphological basis of the tumors and, on the other, justifies the identity of the treatment regimen.
The treatment tactics for patients were the same - the most radical removal of the tumor was performed, followed by radiation and chemotherapy treatment. Neurosurgeons are, of course, more interested in aspects of surgical tactics - maximum reduction in tumor size. In SS, maximum radical tumor removal is an important condition for successful treatment. However, given the not very favorable prognosis of metastatic lesions, there is probably no need to strive for “crippling” radicalism, which leads only to “treating tomograms”. Perhaps in such cases it is necessary to focus on radiosurgical treatment methods.
G.G. Shahinyan
(Moscow)
How are brain tumors diagnosed?
- Neurological examinations help determine whether the tumor is affecting brain function.
- Magnetic resonance imaging (MRI) is the most common method of imaging almost any brain tumor. MRI signals differ depending on the water, calcium, and fat content of the tumor. The nature of the signal is influenced by the cystic component of the tumor and hemorrhage into the tumor.
- Computed tomography (CT) scan – allows visualization of abnormalities or tumors in the brain. The method can help detect bleeding and enlarged fluid-filled spaces in the brain. In addition, computed tomography allows you to see changes in the bones of the skull. CT can also be used to measure the size of a tumor and in cases where the patient does not have access to an MRI, for example, if a person has a pacemaker for the heart.
- Positron emission tomography (PET) or PET-CT scan - a small amount of radioactive substance is injected into the patient's body. This substance is absorbed by actively dividing cells. Because tumor cells are more likely to actively divide, they absorb more radioactive material. The scanner then detects the substance and creates images.
- A lumbar puncture is a procedure in which a needle is used to remove a sample of cerebrospinal fluid to look for tumor cells, blood, or tumor markers.
- Biopsy + histology. A biopsy is the removal of a small amount of tissue for examination under a microscope. This is the only definitive way to diagnose a brain tumor.
Establishing a diagnosis
Diagnosis of brain sarcomas begins with an examination by an oncologist, who records external oncological signs, that is, the appearance of:
- jaundice on mucocutaneous tissue;
- pale skin color;
- bluish tint of lips;
- swelling in the face and neck;
- increased fulness of veins on the surface of the head;
- severe exhaustion.
Intoxication of the body with sarcoma provokes:
- increased body temperature;
- the appearance of general weakness;
- excessive sweating at night;
- decreased desire to eat.
Instrumental diagnostics of brain sarcomas is carried out. Explore:
- lumbar (spinal) puncture to detect blood elements and atypical cells of different sizes and shapes;
- biopsy - to detect small cells with one large or two small nucleoli, to determine the structure of the cytoplasm. With sarcoma, it will be homogeneous and granular;
- CT scan - to establish the boundaries of tumor formation, outlines, signs of growth in the brain, metastases in the lungs and bone tissue.
One type of brain sarcoma can be confirmed by laboratory tests if:
- networks of thin-walled capillaries;
- atypical cancer cells in the form of bundles directed in different directions;
- cells that have a thin shell and large nuclei after a pathological change;
- acute deficiency of healthy cells in the tissue or their complete absence;
- excess intercellular substance with many hyaline and cartilaginous elements of connective tissue.
Read here: Small cell cancer of the esophagus: features of the tumor
As a result of a cytogenetic study, abnormalities of the chromosomes of oncological cells are revealed. When testing blood:
- it is impossible to identify the type of formation due to the lack of specific tumor markers;
- a general analysis reveals the concentration of hemoglobin, red blood cells, leukocytes, platelets and ESR;
- biochemical analysis reveals the percentage of lactate dehydrogenase. At high concentrations (over 250 U/l), the disease will be aggressive.
An x-ray of the sternum may reveal metastasis to soft and bone tissue. A mediastinal tumor may appear round or irregular in shape. Its body varies in size from 1 mm to 10 cm and larger, with a heterogeneous structure.
Is there a cure for brain cancer?
Treatment for a brain tumor is usually complex and may include surgery, chemotherapy, radiation and drug therapy.
Main methods of treatment:
Surgery - a small hole is made in the skull and the tumor is removed;
Radiation therapy - this method uses high-energy radiation from an external or internal source to destroy cancer cells, most often after surgery and in conjunction with chemotherapy. Radiation therapy can slow down the division or stop the growth of malignant cells;
Radiosurgery is an approach to radiation therapy that uses many tiny beams of radiation to target a tumor to kill it. Most often it is used if it is impossible to perform an operation;
Chemotherapy - Chemotherapy drugs are used to kill cancer cells after surgery or to relieve symptoms, or in cases where the tumor cannot be removed;
Carmustine implants are a new way of delivering chemotherapy for certain high-grade tumors where implants are implanted in the brain. Carmustine belongs to a class of drugs called alkylating agents. It works by slowing or stopping the growth of cancer cells in the body.
Treatment methods for sarcomas
After receiving the test results, the doctor makes an accurate diagnosis and develops an individual treatment plan. Treatment tactics for sarcoma are selected taking into account the exact location of the tumor, type of cancer, stage, age of the patient and many other important parameters.
Typically, the treatment protocol involves a combination of three main techniques: chemotherapy, surgery and radiotherapy.
Chemotherapy
One of the main methods of combating various types of sarcomas. It is often prescribed in combination with surgical removal of the tumor, but if surgery is not possible, it can be used as the main method of treatment.
Before surgery, cytostatics reduce the tumor and prepare it for radical removal. After the intervention, drugs are prescribed to destroy metastases and prevent relapse.
The type and dosage of drugs are selected individually. In parallel with chemotherapy courses, maintenance therapy is also prescribed, which reduces side effects and makes it easier to tolerate treatment.
Surgical intervention
The main method of combating this type of oncology. During the operation, the tumor and fragments of surrounding healthy tissue are removed, thereby increasing the chances of completely removing cancer cells from the body. If metastases are found in the lymph nodes, they are also removed during surgery. Source: Surgical treatment of patients with primary soft tissue sarcomas. Baizakov B.T., Shanazarov N.A., Shunko E.L. Tyumen medical journal No. 2, 2010. p. 65-66.
Radiation therapy
Ionizing radiation is often ineffective for this type of cancer. However, in some cases, high-dose radiotherapy is used as an additional treatment before or after surgery. It is also performed in the presence of absolute contraindications to surgical removal of the tumor.
Brain cancer, prognosis
Survival from brain cancer depends on many factors, and only by studying the patient’s medical history can a doctor form a prognosis. To give an overall picture, below are statistics* on five-year survival rates for patients with brain cancer:
- The 5-year survival rate for people with brain cancer or a central nervous system tumor is almost 36%, and the 10-year survival rate is almost 31%.
- Survival rates decline with age.
- The 5-year survival rate for people under 15 years of age is more than 74%.
- For people aged 15 to 39 years, the 5-year survival rate is about 71%.
- The 5-year survival rate for people age 40 and older is about 21%.
But still, you shouldn’t focus on “dry” statistics; everything happens differently for each of us. Therefore, before drawing any conclusions, consult your doctor on this issue.
*-Statistics adapted from the American Cancer Society, Cancer Facts & Figures 2021, ACS website (January 2021)
Prevention
Regular examination by a doctor, undergoing routine medical examinations, taking tests, and timely responding to any changes in health are the main preventive actions.
It is difficult to say how long people with fibrosarcoma live; it all depends on the stage of tumor development. If you feel a deterioration in your health, you begin to lose weight, your appetite has worsened, your body temperature has increased, do not wait until the pain syndrome begins to develop, make an appointment with a specialist.