Possible symptoms of a concussion
- Brief confusion or loss of consciousness. With a strong blow, the moment of injury disappears from memory.
- Dizziness even at rest, and when turning, bending or other changes in body position, the symptom intensifies.
- Severe headache, nausea and vomiting.
- Double vision, inability to concentrate on one point.
- Increased sensitivity to light and sounds.
- Impaired coordination of movements.
- Reaction inhibition - the victim gives an answer to the question after some time.
- Pale skin, weakness, sweating.
Important! A concussion is not always accompanied by visible head injuries, so the absence of wounds does not exclude brain injury.
Clinical picture and diagnosis
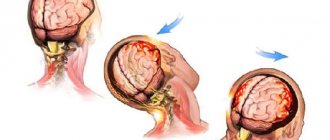
Traumatic swelling of brain tissue can develop almost immediately after injury, or at a later date, as well as after the start of treatment. The clinical manifestations of the injury itself are quite typical and known to everyone - this is a violation of the integrity of the skin, often massive bleeding, and loss of consciousness. With an open head injury, brain matter is visible in the wound, which literally protrudes from the wound during swelling. Bone fragments are visible, and clear cerebrospinal fluid often leaks from the nasal cavity or external auditory canal immediately after the injury.
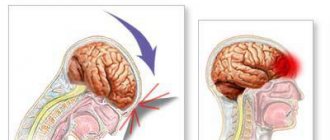
With a closed injury, swelling of the brain tissue develops after a certain period of time and is characterized by three groups of signs: general cerebral signs, symptoms of damage to the cortex, subcortical substance and brain stem, consequences of herniation of individual structures into the foramen magnum.
Among the general cerebral symptoms of traumatic brain injury, headache comes first.
Its intensity is quite high at the time of injury, after which a person may feel short-term relief. As cerebral edema increases, the intensity of the pain syndrome increases; often the pain has a bursting character, covering not only the site of injury, but the entire head.
After an increase in headache, a person complains of so-called cerebral vomiting or central origin. In this case, there is no nausea, vomiting is profuse, and the person does not feel any relief after it.
Already at the initial stage of cerebral edema, there is a disturbance of consciousness as a result of increased intracranial pressure.
A person, as a rule, becomes drowsy, lethargic, and answers questions in monosyllables and with difficulty. Disorientation in time and space is often observed: a person cannot answer simple questions, for example, where he is, who his relatives are, and so on. Consciousness gradually fades away until a cerebral coma occurs.
Another leading sign of cerebral edema is the occurrence of convulsive syndrome. Usually the cramps are generalized, that is, they cover all muscle groups. An objective sign of edema of brain tissue is congestion of the optic nerve head, sluggish reaction of the pupils to light, which is easily detected during a medical examination.
Displacement (dislocation) of the brain is manifested by various focal neurological symptoms, that is, it is determined by compression of individual brain centers. Usually these are disturbances in eye movement, motor and sensory disorders.
After all stages of development of cerebral edema in its final stage are completed, a person exhibits a certain posture (the tone of the extensor muscles predominates), respiratory disorders (shortness of breath or shallow, irregular breathing) and cardiac activity (decreased heart rate and blood pressure, arrhythmia) are noted. impaired swallowing, the appearance of pathological reflexes (they are absent in a healthy state).
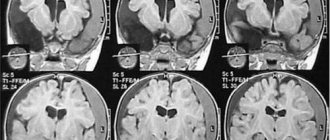
In addition to clinical diagnostics, instrumental research methods such as computed tomography and magnetic resonance imaging are used to confirm the diagnosis.
It is strictly forbidden to do a lumbar puncture, since after it is performed, the displacement of brain structures may increase even more. Often, right during the puncture process, herniation of the cerebellum into the foramen magnum develops and the death of the patient.
Swelling of brain tissue does not tend to heal spontaneously, and therefore can cause death. It is important to establish the onset of this complication as early as possible and emergency care should be started immediately.
The onset of edema is characterized by certain symptoms that appear in a clear sequence. At the first stage, the victim suffers from severe headaches, after which a disturbance occurs at the level of consciousness and unconsciousness. After this, an increase in hydrostatic pressure in the vessels and cavities (hypertension) is observed, and the heart rhythm is disturbed (bradycardia). The next stage is impaired breathing and displacement of brain structures. The patient then dies.
Violation of the level of consciousness, in turn, can be divided into several main stages:
- moderate stun.
- deep stun.
- stupor or depression, accompanied by loss of voluntary, but intact reflex activity.
- coma.
After first aid for a traumatic brain injury, the patient may experience a condition called a lucid gap. It can last for several hours. During this period, the patient begins to feel better, but this condition is deceptive, since negative changes have already begun to occur in the brain. The amount of brain fluid increases, and attacks of severe headache appear. This condition portends the development of edema. If the injury was serious, then the moment of clarity is not always observed, and the symptoms of edema are similar to the condition after a concussion, which significantly complicates the primary diagnosis of cerebral edema.
A neglected state is characterized by the fact that a person begins to lose higher psychological functions.
The victim falls into a comatose state, there is no reaction to external stimuli. Only the blood circulation process and the ability to breathe are preserved. Such patients are connected to a ventilator. In this case, cardiotonic drugs (drugs that selectively stimulate the heart), which are administered intravenously, are used as drug treatment. These methods are necessary to maintain the patient's breathing and blood pressure at proper levels.
In this condition, intracranial pressure is so elevated that blood may stop flowing into the cranial cavity, which leads to an interruption of blood supply to the brain. This phenomenon is called de-animation (empty skull phenomenon). After this, the person is no longer considered alive. According to foreign written sources, such human bodies, which are not yet recognized as corpses, but are no longer living, are called neomorts.
First aid for concussion
- If one or more symptoms are present, immediately call an ambulance or take the victim to a doctor.
- Treat a wound on the head if it appears as a result of an impact.
- For an hour or until the doctor arrives, it is important not to fall asleep, but to remain at rest.
- If you lose consciousness, lay the person on his side, bend his knees, and put his hands under his head.
- If symptoms of a concussion do not immediately appear, it is recommended to rest and not begin vigorous activity.
Moderate brain contusions
This injury usually involves a fracture of the skull bones and is accompanied by subarachnoid hemorrhage. She shows herself:
- loss of consciousness for 1–3 hours, psychomotor agitation;
- amnesia;
- severe dizziness;
- nausea;
- vomiting;
- intense headaches;
- high blood pressure, rapid heartbeat;
- increased body temperature;
- meningeal symptoms;
- severe focal neurological symptoms (changes in muscle tone, paresis, loss of sensation in the limbs, epileptic seizures, speech impairment, etc.).
Signs of moderate brain contusions persist from several weeks to 2 months. The consequence of this condition may be irreversible changes that occurred during the injury.
Recommendations for the treatment of concussions
If hospitalization is not required, with the permission of a doctor, a mild concussion can be treated at home:
- Bed rest and rest are required, no work. Long sleep is very important.
- You cannot read, watch TV, play computer games or use gadgets.
- Under no circumstances should you play sports.
- You are allowed to listen to music, but not through headphones.
- You can use herbal sedative drops or herbal infusions.
- In your diet, you should give preference to dairy and plant products, limit salt intake - to prevent increased pressure, including intracranial pressure.
If the patient seeks medical help in a timely manner and all recommendations are followed, recovery will occur quickly and without complications.
Treatment of concussion
The first few days after injury, the patient is simply observed by doctors in the hospital, a pastel regime is prescribed, and painkillers are prescribed for severe headaches. Monitoring is necessary to identify concussion symptoms that indicate its severity. Diagnostics are also carried out, including MRI. And only on the basis of this is treatment prescribed.
The effectiveness of shock wave therapy
Services of a private clinic in Yeysk
Rest in Yeysk, and quality medical care
Examination of temporary disability in LKK "Sensitive"
Medical certificate for entry into civil service
New rules for a medical certificate for weapons
Why enter into a voluntary health insurance agreement?
"Infanrix" - a three-component vaccine
Brain contusion
Brain contusion. There are mild, moderate and severe brain contusions. Mild brain contusion is observed in 10-15% of patients with traumatic brain injury. It is characterized by a loss of consciousness after an injury lasting from several to tens of minutes. After restoration of consciousness, typical complaints are headache, dizziness, nausea, etc. As a rule, retro-, con-, and anterograde amnesia is noted. Vomiting, sometimes repeated. Moderate bradycardia or tachycardia may be observed, and sometimes systemic arterial hypertension. Breathing and body temperature without significant deviations. Neurological symptoms are usually mild (clonic nystagmus, slight anisocoria, signs of pyramidal insufficiency, meningeal symptoms, etc.), often regressing within 2-3 weeks. after injury. Fractures of the calvarial bones and subarachnoid hemorrhage are possible.
Moderate brain contusion is observed in 8-10% of victims. It is characterized by a loss of consciousness after an injury lasting from several tens of minutes to several hours. Amnesia is pronounced (retro-, con-, anterograde). The headache is often severe. Repeated vomiting may occur. Mental disorders are sometimes observed. Transient disorders of vital functions are possible: bradycardia or tachycardia, increased blood pressure, tachypnea without disturbing the rhythm of breathing and airway patency, low-grade fever. Often, meningeal and brainstem symptoms, dissociation of muscle tone and tendon reflexes along the body axis, bilateral pathological signs, etc. are detected. Focal symptoms are clearly manifested, the nature of which is determined by the localization of the brain contusion; pupillary and oculomotor disorders, paresis of the limbs, disorders of sensitivity, speech, etc. These symptoms gradually (within 3-5 weeks) smooth out, but can persist for a long time. With moderate brain contusion, fractures of the bones of the vault and base of the skull, as well as significant subarachnoid hemorrhage, are often observed.
Severe brain contusion is observed in 5-7% of victims. Characterized by loss of consciousness after injury lasting from several hours to several weeks. Motor agitation is often pronounced. Severe disturbances in vital functions are observed: arterial hypertension (sometimes hypotension), bradycardia or tachycardia, disorders of the frequency and rhythm of breathing, which may be accompanied by disturbances in the patency of the upper respiratory tract. Hyperthermia is pronounced. Primary brainstem neurological symptoms often dominate (floating movements of the eyeballs, gaze paresis, tonic nystagmus, swallowing disorders, bilateral mydriasis or ptosis, divergence of the eyes along the vertical or horizontal axis, changing muscle tone, decerebrate rigidity, suppression or increase in tendon reflexes, reflexes with mucous membranes and skin, bilateral pathological foot signs, etc.), which obscures focal hemispheric symptoms in the first hours and days after injury. Paresis of the limbs (up to paralysis), subcortical disorders of muscle tone, reflexes of oral automatism, etc. can be detected. Generalized or focal epileptic seizures are sometimes observed. Focal symptoms regress slowly; gross residual effects are frequent, primarily in the motor and mental spheres. Severe brain contusion is often accompanied by fractures of the vault and base of the skull, as well as massive subarachnoid hemorrhage.