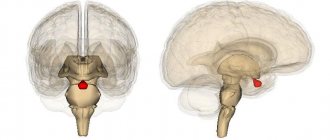
The organ of the endocrine system, the size of which does not normally exceed 15 mm, controls many physiological processes in the body, including regulating metabolism, responsible for the formation of the skeleton, muscular system, functionality of the reproductive system, and also provides resistance to stress. Pituitary adenoma accounts for about 10% of all intracranial neoplasms diagnosed in neurosurgery. The age at risk when the tumor develops most often is between 25 and 50 years, but in recent years there has been a trend toward younger age of the disease. Pituitary adenoma is becoming increasingly common in childhood and adolescence.
Classification
Adenomas are classified according to tumor size as follows:
- 16–25 mm – small formations;
- 26–35 mm – medium-sized tumors;
- 36–59 mm – major pathologies;
- more than 50 mm – giant lesions.
Microadenomas are formations up to 10 mm in size that do not cause changes in the size of the sella turcica. Tumors are divided into hormonally inactive forms (not producing hormones) and hormonally active forms, that is, producing hormones in excessive amounts. Depending on what hormone is produced by the adenoma, the following formations are distinguished:
- prolactinomas (synthesize the hormone prolactin);
- thyrotropinomas (thyroid-stimulating hormone is produced in excess, changing the normal functioning of the thyroid gland, resulting in the development of the disease thyrotoxicosis);
- gnadotropinomas (stimulate the synthesis of human chorionic gonadotropin);
- somatotropinomas (excess somatropic hormone provokes the disease acromegaly);
- adenocorticotropinomas (excessive amounts of adrenocorticotropic hormone cause improper functioning of the adrenal glands, resulting in the development of Cushing's disease).
In addition to the listed types of adenomas, there are formations in the pituitary gland that stimulate the production of several hormones at once. Hormonally inactive tumors and adenomas that synthesize the hormone prolactin account for about 40% of the total number of diagnosed neoplasms in this category.
According to the nature of their spread, hormonally active adenomas can be:
- endosellar (do not extend beyond the pituitary fossa);
- endoextrasellar (extend the contours of the sella turcica) and spread
- in one of the following ways:
- into the cranial cavity;
- under the dura mater;
- towards the sinuses;
- into the area of the ethmoid labyrinth or orbit;
- in the region of the posterior cranial fossa.
According to histological characteristics, neoplasms can be chromophobic, basophilic, acidophilic, or adenohypophyseal.
Pituitary microadenoma
Description of pituitary microadenoma
Pituitary microadenoma is a tumor with a diameter of up to 10 mm. Pituitary adenomas can secrete hormones, but most adenomas are clinically inactive. Pathology of the pituitary gland may be accidentally detected when examining a patient for other neurological diseases. Anomalies of the pituitary gland identified in this way are also called “incidentalomas”. Such microadenomas detected by magnetic resonance imaging cause clinical problems.
In patients with hyperprolactinemia, magnetic resonance imaging reveals unchanged areas of pituitary microadenoma.
Pituitary microadenoma can be identified in patients with diagnosed hyperprolactinemia syndrome, acromegaly, or when diagnosing a patient with Cushing's syndrome. Non-hormone-secreting microadenomas are non-functioning pituitary adenomas (NFPAs) in 90% of cases, although there may be other types of cysts, vascular, neoplastic, hyperplastic or inflammatory processes that will not manifest clinically.
Pathophysiology of pituitary microadenoma
Most pituitary tumors are not permanent. Some may be part of a genetic syndrome, such as multiple endocrine neoplasia type 1 (MEN1), McQueen-Albright syndrome, or Kern complex. Clinical analysis of the obtained cells (cytological examination) shows that in their origin they are all monoclonal mutations of the same cell.
Prolactinomas are the most common of hormone-producing tumors. Other hormone-secreting tumors may secrete:
- corticotropin, which causes Cushing's disease
- growth hormone (somatotropin), which causes acromegaly
- gonadotropin, the clinical manifestations of which depend on its level and less often the gender of the patient
- thyroid-stimulating hormone (TSH), which can cause hyperthyroidism (rare)
Most clinically nonfunctioning pituitary adenomas (NFPAs) are gonadotropic in origin and secrete alpha and beta fragments of the gonadotropin peptide.
The role of genetic mutation is emphasized in the case where patients from four Irish families who had a pituitary tumor had the same mutation as an 18th century patient with a pituitary tumor who suffered from gigantism.
Epidemiology of pituitary microadenoma
Incidence of pituitary microadenoma
In 10–14% of autopsies performed, pituitary adenomas were identified, almost all of which are microadenomas. A meta-analysis of autopsies revealed 22% microadenomas, and 14% with tomography. Pituitary microadenomas occur at any age, regardless of gender.
Previously, when microadenomas were not detected during life, an increase in prolactin was often observed during laboratory blood tests. Now, with the help of magnetic resonance imaging, it is possible to identify pituitary microadenomas that were not previously suspected in the study of patients.
The high incidence of pituitary microadenomas and low incidence of macroadenomas in autopsies indicates that microadenomas rarely progress to the stage of macroadenomas, and macroadenomas manifest themselves clinically during a person’s lifetime.
In 3048 autopsies performed in the United States, studies showed in 316 cases (10%) the presence of one or more pituitary adenomas, their size was less than 3 mm. The immunological test for prolactin was positive in 40% of cases. International studies also record similar results.
Signs of development of pituitary adenoma
The clinical manifestations of pituitary adenoma directly depend on the type of tumor. Significant disturbances in the functioning of the body are observed with adenomas that synthesize hormones.
The consequences of the disease are pathologies such as acromegaly and gigantism, manifested by a disproportionate increase in the size of the limbs, disproportions of the skeleton and skull. Hyperprolactinemia is characterized by decreased sexual function, infertility in women, and impotence in men.
Itsenko-Cushing's disease, which is also included in the list of common pathologies that develop as a result of pituitary adenoma, leads to atrophy of muscle tissue, uneven obesity, and weakening of the walls of blood vessels. The pathology is easy to identify by external signs: moon-shaped face, rosy cheeks, saggy belly, changes in the appearance of the skin.
In case of dysfunction of the thyroid gland caused by a pituitary adenoma, there is increased nervousness, causeless anxiety, increased appetite, tearfulness, mood swings, heart rhythm disturbances, and increased sweating.
In hormonally inactive forms of pituitary adenoma (PAA), the most common signs of the development of the disease are decreased visual acuity (up to complete blindness), attacks of severe headache that cannot be eliminated after taking analgesics, and short-term disturbances of consciousness. These symptoms become more severe as the tumor grows and puts more pressure on nearby brain tissue, most often affecting the optic nerve.
Adenomas differ in the degree of aggressiveness: there are tumors that quickly increase in size and compress tissue, while other neoplasms are not prone to growth. Rare cases include malignant transformation of neoplasms with the formation of metastatic foci in the brain.
All hormonally active pituitary adenomas affect certain target organs, disrupting their functioning due to pathological changes in hormonal levels. Secondary pathologies are similar in symptoms to other endocrine diseases, so differential diagnosis is necessary to establish the correct diagnosis.
Causes of development of pituitary adenoma
Medical science has not established exactly what causes lead to the development of pituitary adenoma. This area continues to be under the radar of researchers. The list of factors that can most likely lead to the onset of the disease includes:
- head injuries;
- infections affecting the brain;
- intrauterine infections;
- frequent cases of pregnancy;
- heredity;
- long-term use of hormonal drugs;
- exhaustion of the nervous system, frequent stress.
Pituitary adenoma in women occurs 1.8–2.3 times more often than in men.
Diagnostics
Comprehensive diagnostics is the basis for correct diagnosis. To determine the hormonal status, a blood test is prescribed with an assessment using the RIA method (radioimmune assessment of hormones). The analysis allows you to determine the level of pituitary tropic hormones.
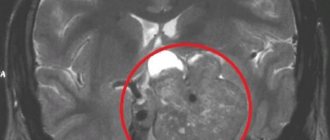
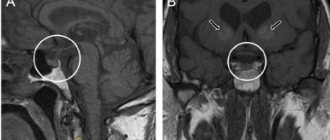
MRI is the main diagnostic method used to detect pituitary adenomas of various sizes. Computed tomography is used less frequently and mainly in cases where it is necessary to visualize hard tissues, the walls of the sella turcica and formations that have spread beyond its boundaries.
CT angiography is one of the most important diagnostic methods performed before planned operations for the removal of large pituitary adenomas. The surgeon must know how the formation is located in relation to the cerebral arteries and optic nerve. Imaging protocols are used directly during surgery.
Dynamic contrast-enhanced magnetic resonance imaging is considered the most informative method for assessing small formations in the pituitary gland. Using a tomograph, you can determine the boundaries and size of the tumor, while ensuring high resolution resolution in the image.
Somatotropinomas in children
Somatotropinomas in children occur in approximately 9%. Most often they are diagnosed in children 12-15 years old. The clinical manifestations of this type of adenoma in children are quite striking: a pronounced acceleration in growth rates, leading to gigantism; a third of patients experience acromegaloid changes in appearance; in puberty girls, the disease is accompanied by menstrual irregularities.
Most often, tumors reach significant sizes, which is accompanied by corresponding neurological symptoms in the form of headaches and visual disturbances.
Currently, most researchers are inclined to neurosurgical tumor removal. Considering the fact that in approximately half of children somatotropinoma has invasive growth, the choice of approach is especially important. Transsphenoidal or transcranial removal of adenomas is used. In addition to neurosurgical treatment, dopamine agonists (bromocriptine, cabergoline, dostinex, etc.) are used. The use of long-acting somatostatin analogues is also effective.
Thus, if the above-described symptoms appear in children, you should immediately contact a neurosurgeon or endocrinologist.
It is necessary to conduct a comprehensive hormonal examination to determine the type of hormonal activity of the tumor, as well as x-ray of the skull, computer and/or magnetic resonance imaging of the brain, and then choose the most adequate treatment method.
After treatment for pituitary adenoma, long-term observation by specialists is necessary in order to timely identify possible relapses of the tumor, as well as select hormone replacement therapy.
Timely and adequate replacement therapy can significantly improve the condition and quality of life of patients treated for pituitary adenomas in childhood.
Questions have arisen. Need specialist advice? Contact me.
Treatment of hormonally active tumors
Treatment of pituitary adenoma is developed on an individual basis and only after receiving accurate diagnostic findings. The main methods are surgery, drug therapy and radiation therapy.
For example, prolactinoma is treated conservatively, with the use of dopamine antagonists. If therapy does not produce results, surgery is prescribed. Radiation is indicated in cases where the above methods of therapy did not achieve the planned result or the operation was not performed effectively enough (tumor fragments remained). Radiation therapy continues until the tumor begins to shrink in size and its tissue disintegrates, which is accompanied by the restoration of physiologically normal hormonal balance.
In the treatment of pituitary adenoma, stereotactic methods are used, when the radio beam is directed directly to the area where the tumor is localized with precise focusing. This approach allows you to keep the surrounding tissues healthy.
Radiation therapy is divided into several methods:
- radiological surgery (radiation exposure is applied during one session);
- radiotherapy (a set of procedures is prescribed at a certain interval).
Radiosurgical treatment of pituitary adenoma is carried out, depending on the indications and capabilities of the clinic, using Gamma Knife medical equipment, remote gamma therapy, a proton beam, and a linear accelerator.
Somatotropinoma, complications of which are acromegaly, gigantism and obesity, is treated mainly surgically. The main surgical method is endoscopy with endonasal access (through the sinuses). Conservative treatment is prescribed as part of the preparation program for surgery, as well as in cases where the operation was not radical enough. Six months after surgery, re-diagnosis using MRI is indicated to detect a possible relapse.
Corticotropinoma, which causes excessive accumulation of the hormone cortisol, which is synthesized by the adrenal glands, occurs most often in women aged 20–45 years. In the absence of adequate treatment, complications such as diabetes mellitus, heart failure, obesity, osteoporosis and other dangerous pathologies develop. Surgical removal of a tumor up to 1 cm in size leads to complete restoration of health.
If there are contraindications, radiation therapy is performed or medication is prescribed.
Contraindications to surgical treatment
Surgical treatment for pituitary adenoma is in most cases the most effective method. Based on the diagnosis, a tumor removal scheme is developed (open or endoscopic surgery with the choice of optimal access).
Contraindications to radical treatment are:
- advanced age;
- heart and kidney failure in the stage of decompensation;
- diseases of the hematopoietic organs;
- untreated infections of any location;
- post-infarction and post-stroke conditions;
- systemic diseases that occur in severe form.
If surgery is not possible, other methods are prescribed to stop the progression of the pathological process and mitigate the symptoms of the disease.
Non-functioning pituitary adenomas (NFPAs)
Non-functioning pituitary adenomas are benign (not cancerous) growths of pituitary tissue located at the base of the brain. Based on the results of autopsies and MRI or MRI imaging studies of the pituitary gland, it was revealed that in every 6 cases a similar type of pituitary adenoma can occur.
While most pituitary tumors produce hormones, nonfunctioning pituitary adenomas are unable to do so—which is why they are called “nonfunctioning.” According to statistics, up to 30% of pituitary adenomas are non-functioning.
Treatment of hormonally inactive forms of pituitary adenoma
Hormonally inactive pituitary adenomas account for 25% of all adenomas (prevalence rate: 6 cases per 1 million population per year). The rarest disease in adults is craniopharygioma. Other types of neoplasms without hormonal activity (hemangioma, dysgerminoma, harmathroma) are detected somewhat more often.
Symptoms indicating the development of tumors in this group are menstrual irregularities in women and decreased erectile function in men. Other signs of pituitary adenoma are weakness, hypotension, and increased fatigue. If the tumor appears in childhood, growth and sexual development are delayed. Impaired water metabolism and neurological symptoms occur in 75% of patients. With active tumor growth, nausea and vomiting intensify, and the most serious consequence is cranial nerve palsy.
The gold standard of treatment is surgical removal of the tumor. Radiation therapy is prescribed when diagnosing remnants of adenoma or in cases of relapse. After surgery, the patient is observed by a doctor, and six months later an MRI examination is performed. The prognosis depends on the location and size of the pituitary adenoma.
With successfully chosen treatment tactics and correctly performed surgery, complete recovery and restoration of working capacity occur. If, as a result of the progression of the pituitary adenoma, visual functions are lost and persistent neurological disorders appear, then the patient receives permanent disability.
Treatment with prolactin.
Currently, there are two treatment options: surgical removal and the use of dopamine agonists (DA). Transsphenoidal (or transcranial - very rarely) adenomectomy is used as surgical treatment. The choice of surgical intervention method depends on the size, direction of growth and extent of the tumor.
However, today most authors consider the use of dopamine agonists to be the method of choice. With good sensitivity to the drug, even with a large tumor size, a decrease in tumor mass and improvement in condition can occur in the shortest possible time from several days to 1-2 weeks from the start of treatment. However, the choice of treatment method always remains with specialists.
When should you see a doctor?
Pituitary adenoma is accompanied by endocrine disorders, which always cause negative symptoms. Be sure to make an appointment with your doctor if you experience weight loss or gain without changing your diet, blurred vision, changes in the appearance of the skin, headaches, or sexual dysfunction. You will be prescribed a series of tests, based on which a specialist will make an accurate diagnosis. The sooner you contact a medical clinic, the sooner you will receive a conclusion, the shorter and more effective the treatment will be.
First appointment with a therapist. Next, based on complaints and examination results, the specialist will write a referral to a specialized doctor. Women are examined by a gynecologist-endocrinologist, men by an andrologist. Consultations with doctors of other specializations may be required.
The MedCom clinic in Ryazan has everything necessary for the diagnosis and treatment of pituitary adenoma. Experienced doctors will conduct an emergency examination and develop the most effective and safe treatment regimen. Make an appointment by calling +7 (4912) 77–92–02 or using the online contact form. Do not delay your visit to the doctor - pituitary adenoma can be successfully treated in the early stages!