Types of pituitary adenoma
There are various criteria for classifying benign pituitary tumors.
To size:
- microadenoma – tumor size up to 10 mm;
- mesoadenoma - a tumor measuring from 10 mm to 20 mm, located within the sella turcica;
- macroadenoma - a tumor measuring from 10 mm to 30 mm, or extending beyond the boundaries of the sella turcica;
- giant adenoma – a tumor larger than 30 mm.
In a simplified classification, meso- and giant adenomas are classified as medium and giant macroadenomas, respectively.
By nature of distribution:
- endosellar (intrasellar) – the tumor does not extend beyond the boundaries of the sella turcica;
- endosuprasellar - the adenoma grows upward beyond the sella turcica towards the optic chiasm;
- endolaterosellar - spread of the neoplasm into the cavernous sinuses by germination of the lateral wall of the sella turcica;
- endoinfrasellar – pituitary adenoma grows downwards from the sella turcica.
A tumor growing in different directions is called endo-supra-infra-laterosellar.
By origin:
- primary tumors;
- secondary, developed as a result of hypofunction of peripheral endocrine glands;
- adenomas caused by disruption of the hypothalamus, as well as the production of releasing hormones in ectopic formations located in non-endocrine organs.
Based on hormonal activity, pituitary adenomas are divided into active (about 60% of adenomas) and inactive (about 40%). Hormonally active tumors, based on the type of hormones they produce, are divided into:
- somatotropinomas;
- corticotropinomas;
- thyrotropinomas;
- prolactinomas.
Gonadotropinomas are also isolated, which most often do not affect hormonal levels, since they produce biologically inactive hormones. However, sometimes these tumors produce active forms of follicle-stimulating hormone and luteinizing hormone.
There are mixed tumors that produce more than one type of hormones.
Causes and classification
It is not known exactly what causes the disease. The development of microadenoma is associated with a disruption in the production of hypothalamic hormones. The releasing factors of this organ regulate the activity of the pituitary gland. Another version is gene mutations that lead to the degeneration of healthy cells.
The following factors can provoke the occurrence of a pituitary tumor:
- inflammation of the meninges, abscess;
- neuroinfections (tuberculosis, neurosyphilis);
- TBI;
- intrauterine hypoxia;
- psycho-emotional overload;
- damage to the central nervous system during childbirth.
There are hormonally active types of pituitary neoplasia and inactive ones.
| Active neoplastic process | Characteristic |
| Prolactinoma | The most common form. Characterized by increased secretion of prolactin, enhancing lactation |
| Somatotropinoma | Excess somatotropin, which stimulates growth |
| Chromophobe microadenoma | Somatostatin stops growth |
| Thyrotropinoma of the pituitary gland | Causes hypothyroidism due to excess production of thyrotropin |
| Corticotropinoma | Leads to adrenal dysfunction |
| Gonadotropinoma | The rarest tumor of the pituitary gland, leading to disruption of the reproductive system |
Inactive neoplastic processes of the pituitary gland are accompanied by pituitary insufficiency (hypopituitarism).
Causes of pathology
The reasons for the development of pituitary adenoma are factors that directly affect the brain and the gland itself (trauma, neuroinfections), as well as those that have an indirect effect due to the pathology of other glands and organs. The latter include disorders of the regulatory function of the hypothalamus, thyroid gland, gonads, as well as the appearance in organs that are not endocrine glands of areas that produce hormones (for example, such accumulations of cells are found in small cell lung cancer).
In hereditary forms of the disease, mutations in suppressor genes that suppress the process of tumor cell changes play a role in the occurrence of tumors. The causes of the mutation are unknownSource: Pituitary adenomas within hereditary syndromes. Mamedova E.O., Przhiyalkovskaya E.G., Pigarova E.A., Mokrysheva N.G., Dzeranova L.K., Tyulpakov A.N. Problems of endocrinology, 2014. p. 51-59.
Causes
What it is? At the moment, medicine does not indicate the exact causes that can cause pituitary adenoma. But there are a number of factors contributing to the appearance of hypertension:
- traumatic brain injuries;
- pathologies of intrauterine development;
- various neuroinfections - for example, encephalitis, meningitis, polio, brucellosis, neurosyphilis, tuberculosis, brain abscess;
- According to some data, long-term use of oral contraceptives is dangerous.
All the causes of pituitary adenoma can be combined according to their consequences - they all cause hyperplasia (excessive cell proliferation) of pituitary tissue due to hormonal disorders.
Symptoms of pituitary adenoma
Clinical manifestations of the disease can be divided into two groups. With microadenomas or small endosellar tumors, endocrine symptoms come to the fore, varying depending on the hormones secreted.
With large hormonally inactive adenomas spreading beyond the sella turcica, neuro-ophthalmological symptoms prevail, which are different for tumors growing in different directions.
Endocrine symptoms
Somatotropinoma
A tumor that produces somatotropin, or growth hormone. Its manifestations depend on the period of tumor onset. Before the growth of bone tissue is complete (in adolescence and young adulthood), it manifests itself as symptoms of gigantism; in adults, acromegaly.
Gigantism is a proportional increase in bone length and overall height. Women can reach a height of 190 cm, men - over 2 meters.
Acromegaly is characterized by pathological growth of bones, soft tissues, cartilage, and corresponding changes in appearance - the nose, lips, chin, brow ridges, hands, feet increase disproportionately to the rest of the body. Patients experience hyperhidrosis (excessive sweating), hirsutism (excessive hair growth), severe sebum production, and the appearance of papillomas, warts, and nevi on the skin.
In addition, the patient’s internal organs become enlarged, and metabolic and endocrine processes are disrupted. From the cardiovascular system, increased blood pressure, cardiomyopathy, and cerebrovascular accidents are observed. From the nervous system - polyneuropathy, manifested by pain, paresthesia, decreased sensitivity of the peripheral parts of the extremities. The development of obesity, secondary diabetes mellitus, and thyroid pathologies is possible. Source: Main types of complications with pituitary adenomas. K. E. Makhkamov, M. M. Azizov. Bulletin of Emergency Medicine, 2015. p. 90-92.
Corticotropinoma
A pituitary adenoma that produces ACTH is an adenocorticotropic hormone, an excess of which develops Cushing's disease. Its symptoms:
- Cushingoid obesity - an increase in the volume of adipose tissue on the face, back, hips and buttocks, and abdomen;
- swelling and congestion of the face;
- striae - stretch marks of purple-violet color on the skin of the abdomen and thighs;
- skin atrophy, especially on the back of the hands, pustular diseases, fungal infections;
- osteoporosis accompanied by multiple compression fractures;
- arterial hypertension, cardiovascular failure;
- secondary diabetes mellitus.
Thyrotropinoma
A neoplasm that produces thyroid-stimulating hormone. Thyrotropinoma can be primary or secondary.
Primary thyrotropinoma has characteristic signs of thyrotoxicosis (excess thyroid secretion). Its symptoms:
- cardiopalmus;
- tremor - trembling throughout the body, shaking fingers;
- hyperhidrosis;
- nervousness;
- bad dream.
Secondary thyrotropinoma develops as a result of a long course of uncompensated hypothyroidism. It is characterized by:
- weakness, lethargy;
- body swelling and weight gain;
- lethargy, absent-mindedness, memory impairment;
- slow metabolism.
Prolactinoma
One of the most common gland tumors. It arises from cells that synthesize the hormone prolactin. The symptoms of this pituitary adenoma are different in women and men. Source: Aggressive pituitary adenomas (literature review and clinical observation). Kalinin P.L., Trunin Yu.Yu., Fomichev D.V., Chernov I.V., Ryzhova M.V. Tumors of the head and neck, 2021. p. 74-80.
Among women:
- decreased sexual desire up to frigidity;
- menstrual irregularities;
- discharge from the nipples outside the period of breastfeeding;
- infertility.
For men:
- gynecomastia – enlargement of the mammary glands;
- hypoplasia of secondary sexual characteristics;
- decreased libido, erectile dysfunction;
- infertility.
Symptoms
Manifestations of pituitary neoplasia depend on its type, functional activity, gender of the patient, and size of the microadenoma.
The most common signs for:
| Women | Men | Both sexes |
| Lengthening the cycle | erectile disfunction | Decreased libido |
| Lack of menstruation (amenorrhea) | Gynecomastia | Discharge from the mammary glands (more often in women) |
| Shortening of menstruation (up to 3 days) | Prostate dysfunction | Underdevelopment of reproductive organs |
| Metrorrhagia | Female pattern pubic hair | Infertility is a common symptom in diseases of the pituitary gland |
| Alternation of heavy and scanty discharge | Facial hair does not grow well, it is sparse and soft | Deterioration of intellectual abilities, decreased cognitive skills |
| Signs of osteoporosis | Wide hips, relatively narrow shoulders | Nervous excitability |
| Male pattern hair growth | Insomnia | |
| Skin problems | Excess weight | |
| Heart failure, hypertension | ||
| Progressive weakness | ||
| Diabetes |
Gonadotropinomas
Most often hormonally inactive, they can rarely produce active forms of follicle-stimulating or luteinizing hormones, causing ovarian hyperstimulation syndrome in women.
Neuro-ophthalmological signs
With endosuprasellar adenoma, partial loss of visual fields is observed while maintaining visual acuity. An increase in tumor size leads to gradual atrophy of the optic nerves and blindness.
A tumor growing to the sides causes impaired oculomotor function (ophthalmoplegia) and double vision (diplopia), and decreased visual acuity.
When an adenoma grows into the bottom of the sella turcica, patients note nasal congestion, simulating the clinical picture of sinusitis or nasal tumors.
If the tumor grows towards the hypothalamus, patients complain of sleep disturbances, uncontrolled appetite, unstable thermoregulation (fever, chills), emotional disturbances: unstable mood, tearfulness, irritability.
With a large adenoma and its multidirectional growth, the symptoms will overlap each other and be masked. The following neurological manifestations are possible:
- headache, dizziness;
- nausea, vomiting;
- speech and facial expression disorders;
- dysphagia is a swallowing disorder.
Treatment prognosis
Pituitary adenomas are benign formations, but with active growth they can cause many problems and even degenerate into a malignant process.
If the tumor is large (more than 2 cm), then there is a high risk of its recurrence in the next 5 years after surgical removal.
The nature of the adenoma is also of no small importance in predicting such formations. For example, with prolactinomas or somatotropinomas, a quarter of patients experience complete restoration of endocrine activity; with microcorticotropinomas, 85% of patients recover completely.
Average relapse rates are approximately 12%, and recovery ends in 65-67% of cases. But such forecasts are justified only if you turn to highly specialized specialists in a timely manner.
Diagnosis of the disease
Patients with suspected pituitary adenoma complain to various doctors: a neurologist, ophthalmologist or endocrinologist.
At the initial appointment, the doctor will conduct a general examination, collect an anamnesis of life and illness, prescribe laboratory and instrumental tests: general blood and urine tests, blood biochemistry, ECG. A doctor of appropriate specialization will conduct an ophthalmoscopy, test visual acuity, neurological examination, and evaluate the existing symptoms.
In addition, the following studies are indicated for patients with pituitary adenoma:
- radiography of the skull;
- CT, MRI of the brain;
- Ultrasound of the thyroid gland, heart, liver, spleen;
- analysis of hormone levels in blood and saliva.
If surgical intervention is indicated, the patient must consult a neurosurgeon.
Diagnostics
To make a diagnosis, the doctor examines the medical history, examines the patient, and finds out complaints that are usually associated with hormonal disorders.
To identify pituitary microadenoma, the following is prescribed:
- MRI with contrast is the most informative diagnostic method;
- Craniography – x-ray of the skull in frontal and lateral projections. The examination is effective when the lesion grows;
- CT scan;
- determination of pituitary hormones in the blood. In case of deviation from the norm, the analysis is carried out two or three times.
An inactive microadenoma is most often discovered by chance during a physical examination or diagnosis of another pathology, since in most cases it is asymptomatic. The patient is consulted by an endocrinologist, neurologist, neurosurgeon, and mammologist.
Treatment of the disease
According to clinical guidelines, there are three main approaches to the treatment of pituitary adenoma:
- conservative (medicines);
- radiation therapy;
- neurosurgical.
The drug method is indicated for small prolactin-producing adenomas. Treatment is carried out with prolactin antagonist drugs.
Radiation therapy is carried out in various ways: gamma, proton, external beam radiation therapy, stereotactic radiosurgery.
For somatotropinomas and corticotropinomas, neurosurgical removal is used. Before surgery, hormonal therapy is often prescribed to reduce the effect of hormone hypersecretion, which sometimes leads to a reduction in the size of the tumor. Drug and radiation therapy are also prescribed after surgery according to indications.
Neurosurgical intervention is recommended for macroadenomas that have severe symptoms and a risk of complications - visual impairment, up to complete blindness, hemorrhage, brain cysts. Source: Pituitary adenomas: history, prevalence, clinical picture, diagnosis, treatment. V. P. Syty, A. A. Gonchar, Yu. V. Syty. Problems of health and ecology, 2010. p. 41-50.
Conservative treatment
Drug treatment is usually prescribed for small tumors and only after a thorough examination of the patient. If the tumor is deprived of the corresponding receptors, then conservative therapy will not produce results and the only option will be surgical or radiation removal of the tumor.
- Drug therapy is justified only if the neoplasia is small in size and there are no signs of visual disturbances. If the tumor is large, then it is performed before surgery to improve the patient's condition before surgery or after it as replacement therapy.
- Treatment for prolactin tumors that produce the hormone prolactin in large quantities is considered the most effective. Prescribing drugs from the group of dopaminomimetics (parlodel, cabergoline) has a good therapeutic effect and even allows you to do without surgery. Cabergoline is considered a new generation drug; it can not only reduce prolactin overproduction and tumor size, but also restore sexual function and sperm parameters in men with minimal side effects. Conservative treatment is possible in the absence of progressive visual impairment, and if it is carried out on a young woman planning a pregnancy, then taking medications will not be an obstacle.
In the case of somatotropic tumors, somatostatin analogues are used, in case of thyrotoxicosis, thyreostatics are prescribed, and in case of Itsenko-Cushing's disease, provoked by a pituitary adenoma, aminoglutethimide derivatives are effective. It is worth noting that in the last two cases, drug therapy cannot be permanent, but serves only as a preparatory stage for subsequent surgery.
Prognosis and rehabilitation
With timely diagnosis and proper treatment, pituitary adenoma has a generally favorable prognosis without undesirable consequences. Remission after removal of an adenoma occurs in 70-80% of cases, this figure is higher for microcorticotropins and lower for somatotropins and prolactin. The relapse rate is about 12%. Postoperative mortality is low - approximately 4%, decreasing to almost 0 for endosellar and endosuprasellar tumors. The risk of mortality is higher with a large adenoma, its penetration into the ventricular system, or tumor growth of blood vessels.
Rehabilitation, as a rule, does not take much time, since most pituitary adenomas are removed transnasally (through the nose) using endoscopic instruments. In the early postoperative period, the patient is prescribed painkillers, hemostatic agents, and antibiotic therapy. If there are no complications, after a few days the patient is discharged home and is under the supervision of a doctor (ENT, ophthalmologist, endocrinologist) in the clinic. No special rehabilitation measures are required.
Surgery
When surgically removing an adenoma, you can use one of two methods:
- Transcranial – involves performing craniotomy.
- Transsphenoidal - through the nasal cavity.
If microadenomas and macroadenomas are diagnosed, which do not have a serious effect on the surrounding tissues, surgery is performed transsphenoidally. If the tumor reaches a gigantic size (from 10 cm in diameter), only transcranial removal is recommended.
Transsphenoidal removal of an adenoma is allowed when the tumor is limited to the sella turcica or extends beyond it by no more than 2 cm. It is performed in a hospital setting after consultation with a neurosurgeon. The introduction of endoscopic equipment is performed under general anesthesia. A fiber optic endoscope is inserted into the anterior cranial fossa through the right nasal passage. Next, to free access to the area of the sella turcica, an incision is made into the wall of the sphenoid bone. The pituitary adenoma is excised and removed.
All surgical procedures are performed under an endoscope; an enlarged image of the current process is displayed on the monitor, making it possible for the neurosurgeon to have a wide overview of the surgical field. The operation lasts about two to three hours. On the first day after surgery, the patient can already be active, and on the 4th day he is completely discharged from the hospital in the absence of complications. In 95% of cases of such an operation, the pituitary adenoma is completely cured.
Transcranial surgery is performed in the most severe cases under general anesthesia by craniotomy. The high morbidity and risk of complications force neurosurgeons to take this step only when it is impossible to use the endoscopic method of removing an adenoma, for example, when the tumor grows inside the brain tissue.
Prevention
There is no specific prevention of pituitary adenoma, since the exact causes of tumor development are unknown. If suspicious symptoms appear, you should immediately consult a doctor. Timely diagnosis and treatment will help achieve the most favorable results and maintain the patient’s quality of life.
Sources:
- The main types of complications from pituitary adenomas. K. E. Makhkamov, M. M. Azizov. Bulletin of Emergency Medicine, 2015. p. 90-92
- Pituitary adenomas within hereditary syndromes. Mamedova E.O., Przhiyalkovskaya E.G., Pigarova E.A., Mokrysheva N.G., Dzeranova L.K., Tyulpakov A.N. Problems of endocrinology, 2014. p. 51-59
- Aggressive pituitary adenomas (literature review and clinical observation). Kalinin P.L.,
- Trunin Yu.Yu., Fomichev D.V., Chernov I.V., Ryzhova M.V. Tumors of the head and neck, 2021. p. 74-80
- Pituitary adenomas: history, prevalence, clinical picture, diagnosis, treatment. V. P. Syty, A. A. Gonchar, Yu. V. Syty. Problems of health and ecology, 2010. p. 41-50
Transnasal surgery to remove pituitary adenoma of the brain
This is a minimally invasive procedure that does not require a craniotomy and does not leave behind any cosmetic defects. It is most often performed under local anesthesia; the surgeon’s main instrument will be an endoscope. A neurosurgeon removes a brain tumor through the nose using an optical device. How is all this done?
- The patient is in a sitting or semi-sitting position during the procedure. A thin endoscope tube (no more than 4 mm in diameter), equipped with a video camera at the end, is carefully inserted into the nasal cavity.
- The real-time image of the lesion and adjacent structures will be transmitted to the intraoperative monitor. As the endoscopic probe advances, the surgeon performs a series of sequential manipulations to get to the part of the brain of interest.
- First, the nasal mucosa is separated to expose and open the anterior wall. The thin bony septum is then cut. Behind it is the desired element - the sella turcica. A small hole is made in the bottom of the sella turcica by separating a small fragment of the bone.
- Next, using microsurgical instruments placed in the channel of the endoscope tube, pathological tissues are gradually chipped off through the access created by the surgeon until the tumor is completely eliminated.
- At the final stage, the hole created in the bottom of the saddle is covered with a bone fragment, which is fixed with special glue. The nasal passages are thoroughly treated with antiseptics, but not tamponed.
The patient is activated in the early period – already on the first day after low-traumatic neurosurgery. About 3-4 days later, you will be discharged from the hospital; then you will need to undergo a special rehabilitation course (antibiotic therapy, physiotherapy, etc.). Despite undergoing surgery to excise a pituitary adenoma, some patients will be asked to additionally adhere to hormone replacement therapy.
The risks of intra- and postoperative complications during the endoscopic procedure are reduced to a minimum – 1%-2%. For comparison, negative reactions of various types after transcranial resection of AGGM occur in approximately 6-10 people. out of 100 operated patients.
After a transnasal session, most people experience difficulty in nasal breathing and discomfort in the nasopharynx for some time. The reason is the necessary intraoperative destruction of individual structures of the nose, resulting in painful symptoms. Discomfort in the nasopharyngeal area is usually not regarded as a complication if it does not intensify and does not last long (up to 1-1.5 months).
The final assessment of the effect of the operation is possible only after 6 months using MRI images and the results of hormonal tests. In general, with timely and correct diagnosis and surgical intervention, high-quality rehabilitation, the prognosis is favorable.
Forecast of the course of the pathology
Endocrinologists can give a favorable prognosis for microadenomas only with timely detection and treatment of small tumors. If the neoplasm does not manifest itself, then it does not affect the quality of life in any way. Refusal to treat hormonal imbalance or remove a tumor can lead to consequences that are difficult to eliminate.
Normalizing the production of hormones eliminates nervousness, improves metabolic processes, relieves infertility and decreased libido. Surgery for visual dysfunction almost completely restores vision.
Microadenoma is a tumor that is not dangerous in terms of possible lethal outcome. But its development can cause the most undesirable changes for a woman in appearance and mental health. Identification of even minor signs similar to the symptoms of an adenoma should prompt you to consult a doctor for a referral for a comprehensive examination.
Not long ago, neurosurgeon Vladimir Anatolyevich Zhuravlev gave an interview to the medical portal 103.by and answered questions about pituitary adenomas:
- What are the clinical manifestations?
- Is there prevention?
- What treatment is possible?
- Is it possible to conceive and give birth to a child with such a pathology?
The article is available on the portal 103.by, and we also publish it below on our website.
The pituitary gland is a small gland that is located in the head and controls a huge number of body functions. Nature reliably protected him from external influences, but remained powerless against internal changes. Blindness, infertility, sexual dysfunction, hair loss, unpleasant changes in appearance - these are not always the consequences of chronic diseases or negative influences from the outside. Similar problems are often caused by pituitary adenoma.
What it is? What are the first “bells”? How to diagnose the disease and how to treat it? These and other questions are answered by Vladimir Zhuravlev, Candidate of Medical Sciences, Associate Professor of the Department of Neurology and Neurosurgery of the BelMAPO, neurosurgeon of the highest medical category.
-What is the pituitary gland?
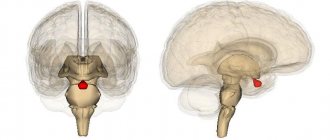
— The pituitary gland is the most amazing endocrine gland in our body. It resembles a bean in size and shape, about 15 mm. The pituitary gland is hidden in the most protected place of the head, in the center of the base of the skull, in an isolated bone bed - the sella turcica.
- What are its functions?
- This little “bean” secretes hormones that control all the endocrine glands of our body. His area of responsibility includes metabolism in the body, the formation of the skeleton and muscle mass, growth, and reproductive function. In addition, by controlling the adrenal glands, the pituitary gland ensures an adequate response of the body to all external influences - resistance to stress. In fact, the pituitary gland has much more functions and they all differ depending on the age and physiological periods of life. In childhood, the somatotropic function comes to the fore . From Latin this word is translated as “building the body.” This refers to growth, an increase in muscle mass and other integral changes in the body associated with this process.
During adolescence, hormonal changes occur, called puberty. Secondary sexual characteristics develop. During this period, gonadotropic hormones of the pituitary gland play a particularly important role, regulating the function of the child’s gonads. This is how body type, features of adipose tissue deposition, hair growth and many other features of our body are formed. This formation ends with the body’s ability to produce healthy germ cells or, in other words, the ability to procreate. In general, the gland has a lot of tasks. A failure in its functioning causes serious problems. Just imagine that the processor responsible for the operation of the entire computer system has broken down.
— By what signs can you understand that there are problems with the pituitary gland?
— The first “bells” can be seen by a pediatrician or therapist. During childhood, a child may stop growing. Stunting, especially against the background of the development of other problems - for example, obesity, arterial hypertension, which is not characteristic of age, etc. These symptoms may indicate a dysregulation of the endocrine system. In adulthood, this can manifest itself in changes in a person's physique and appearance, for example:
- facial features, fingers and hands, feet, and tongue become larger and larger. These manifestations are symptoms of acromegaly;
- the face becomes “moon-shaped”, arms and legs become very thin, and fat is redistributed to the body: to the stomach and chest. Symptoms are characteristic of Itsenko-Cushing's disease;
- dryness and thinning of the skin appear, bruising is very easy.
- blood pressure rises.
In people over 60 years of age, the clinical picture of pituitary tumors is less clear, and it becomes more difficult to suspect the disease.
As a rule, the average time from the appearance of the first symptoms of pituitary adenoma to diagnosis in adults takes: in women - about 1 year, in men - 6 years. The fact is that one of the first symptoms in young people is sexual dysfunction. For example, a woman’s menstrual cycle is disrupted. In such cases, as a rule, she does not delay and promptly seeks advice from a doctor. If a man’s libido decreases, then not everyone immediately goes to a specialist with complaints of decreased sexual function. In case of problems with conception, the woman is also most often examined first. Although the problem may be male infertility due to dysfunction of the pituitary gland.
— What is a pituitary adenoma?
Benign pituitary adenoma is a whole group of tumors, different in nature, symptoms, course of the disease and prognosis. Pituitary adenomas are the third most common among all intracranial tumors.
They can be divided into two groups:
- hormonally inactive (non-secreting hormones);
- hormonally active (producing excess amounts of pituitary hormones).
By size they are distinguished:
- microadenomas (up to 10 mm);
- macroadenomas (more than 10 mm).
The main types of hormonally active pituitary adenomas, depending on what hormone the adenoma produces, are as follows:
- prolactinomas - secreting the hormone prolactin;
- somatotropinomas - producing somatotropic hormone. The disease is called acromegaly;
- thyrotropinomas - secrete thyroid-stimulating hormone. It helps improve thyroid function. The name of the pathology is thyrotoxicosis;
- adenocorticotropinomas - produce adrenocorticotropic hormone, which stimulates the adrenal glands. Causes Cushing's disease.
There are also pituitary adenomas that provoke several hormones at once. The most common are hormonally inactive adenomas, which do not produce hormones, and prolactinomas, which produce the hormone prolactin. Their share is approximately 40%.
— What are the clinical manifestations of pituitary adenoma?
— Unfortunately, pituitary adenomas do not have their own characteristic symptoms. Therefore, diagnosing them is quite difficult. Symptoms may include:
- headache;
- general weakness, decreased blood pressure;
- blurred vision, loss of visual fields, decreased acuity;
- changes in appearance not related to eating behavior.
The clinical picture of hormonally active pituitary tumors varies depending on the hypersecretion of a particular hormone. Prolactinomas are the most common hormonally active pituitary adenomas. They manifest themselves differently depending on the age and gender of the patient:
- women have menstrual irregularities and associated infertility;
- in men and women, libido and potency decrease, and infertility is noted;
- enlargement of the mammary glands, galactorrhea (spontaneous leakage of milk from the mammary glands without connection with the process of feeding the child).
- For what reasons does such a tumor occur?
— The question has not been fully studied. There is a theory that the problem is a “breakdown” of certain genes. Why this “breakdown” occurs is not completely known to scientists.
— Which doctor can diagnose an adenoma?
“Due to the variety of symptoms, a patient can contact doctors in a dozen specialties. The diagnostic sequence depends on the profile of the specialist to whom the patient turned. If the disease debuts in childhood, pediatricians will encounter the first complaints (short stature). The pituitary gland is an organ that regulates the function of the endocrine system. And therefore, it is most likely that an adult patient will first contact an endocrinologist. And menstrual dysfunction will lead a woman to a gynecologist.
Confirmation of the diagnosis is:
- MRI of the brain and pituitary gland;
- laboratory diagnostics (study of hormones of the pituitary gland and peripheral endocrine glands);
- consultation with an endocrinologist to determine the functional state of the endocrine system and hormonal activity of the adenoma;
- examination by an ophthalmologist (examination of visual acuity and fields).
Several doctors also take part in the treatment of pituitary adenomas:
- neurosurgeon;
- endocrinologist;
- ophthalmologist;
- and, possibly, doctors of other specialties, for example: gynecologists, oncologists, radiologists.
— What treatment is possible?
The following treatment methods are used:
- Surgical removal of the tumor.
At the moment, the most modern and effective is the transsphenoidal endoscopic method of tumor removal (removal is carried out through the nose).
- Radiation treatment.
Appointed when:
- the operation is impossible. For example, in the presence of absolute contraindications due to heart disease, kidney disease, etc.);
- the operation cannot be performed for technical reasons (the location of the tumor and its spread into the neurovascular structures will not allow the tumor to be completely removed);
- the previous operation was ineffective (there was no achievement of hormonal compensation after tumor removal).
Treatment options include so-called stereotactic methods, when radiation is applied directly to the tumor, with the most precise focusing, with minimal impact on surrounding tissue. In our country there are the following treatment methods:
- radiosurgery (when the entire radiation dose is delivered in one session);
- radiotherapy (when treatment is divided into several sessions). Radiosurgical treatment is carried out using a special device called a Gamma Knife.
3. Drug therapy.
Used for prolactinomas. This treatment method allows you to control up to 90% of all prolactinomas. There are medications used for other adenomas, but their prescription is carried out individually in each case by a council of several specialists.
Possible dangers and require treatment:
- hormonally active pituitary adenomas;
- pituitary adenomas, the size of which exceeds the size of the place from which they originate, that is, these tumors spread to adjacent parts of the brain. They begin to compress the optic nerves (they pass nearby). In this case, vision decreases, which can lead to blindness.
Hormonally inactive adenomas of small sizes (up to 10 mm), detected by chance, most often on MRI during examination for some other reason. They are called "chance finds." There is even a special term for them - incidentaloma. Such tumors, as a rule, do not grow during life, have no symptoms and only require dynamic monitoring. When deciding on the choice of treatment method for pituitary adenoma, a multidisciplinary approach is used (participation of doctors of various specialties). Prognosis for the treatment of pituitary adenoma must be given individually in each specific case.
— Is it possible to give birth to a child with prolactinoma?
- A very important point. The situation called “hyperprolactinemia” should not be confused with prolactinoma. With hyperprolactinemia, there is a lot of the hormone prolactin in the blood, but the cause of this is not a pituitary adenoma. As mentioned earlier, prolactinoma is a hormonally active pituitary adenoma that secretes an excess of the hormone prolactin. An endocrinologist can distinguish between these conditions. How to prescribe adequate treatment. The most informative way to detect tumors is MRI. But the prognosis for restoring fertility in such cases is different. The main symptom of prolactinoma is amenorrhea (lack of menstruation) and infertility. When treated with dopamine agonists, the tumor decreases in size and normal hormonal secretion is restored. Thus, in some cases, it is possible to restore fertility (the ability to become pregnant and give birth). But, unfortunately, this does not always happen, since the regulation of the activity of the endocrine glands is very complex.
— What happens if the pituitary adenoma is not treated?
— As I already said, some types of adenoma do not require treatment at all. In every fourth person on Earth, the pituitary gland has some kind of peculiarity inside it (cysts, seals, scars, zones of atrophy or hyperplasia, microadenomas without hormonal activity, etc.). But health is not always at risk in this case. It happens that a hormonally inactive adenoma is simply present, but does not have any effect on the body. In such cases, periodic monitoring is necessary.
Requires treatment:
- Hormonally active pituitary adenomas, which cause hormonal disorders and steadily progress. Therefore, the lack of timely treatment can lead to the development of severe, sometimes fatal complications. For example, with acromegaly, myocardial infarction or stroke may develop due to cardiac dysfunction.
- Hormonally inactive macroadenomas, which, when increasing in size, can compress the optic nerves, which can lead to the development of blindness. Unfortunately, such vision loss is irreversible. Compression of other parts of the brain can lead to displacement of the brain inside the skull and the development of hemorrhages or stroke.
By the way. There are tumors with extremely aggressive growth. They need to be treated quickly, using complete surgical removal combined with radiation if possible.
— What types of operations are used to remove pituitary adenomas?
— There are two types of surgical intervention possible:
- traditional craniotomy - craniotomy and tumor removal using an operating microscope. This method is used less and less, mainly when the tumor has spread and it is impossible to perform surgery through the nose;
- transsphenoidal endoscopic removal. A modern minimally invasive method in which the operation is performed through the nose. About 95% of pituitary adenomas are removed this way today. Today, this method in the world is the most effective, safe, reduces surgery time and facilitates subsequent recovery.
— Are the operations performed under general anesthesia?
- Without fail.
— Are there situations when operations are contraindicated?
— Yes, there are contraindications for operations. Among them:
- infectious diseases that are in the active phase. For example, influenza or ARVI also force doctors to postpone surgery;
- blood clotting disorder;
- uncompensated problems of the cardiovascular system and other internal organs that require correction.
— How long does it take to recover after surgery?
— On average it lasts a month. The patient remains in the hospital for about a week after the operation. Then he goes home, but visits an endocrinologist and neurologist. And also, if necessary, an ophthalmologist and other specialists. As a rule, after surgery, patients continue to lead their previous lifestyle. They return to work and usual activities.
— Is there a way to prevent pituitary adenoma?
— Regarding this problem, the best prevention is self-control. Do not neglect age-appropriate examinations. Regularly monitor your blood sugar levels, blood pressure, and monitor your body weight. Get medical checkups on time. If you feel unwell, do not delay, consult a doctor. Any problem can be solved faster and easier in the early stages.
Be healthy!
When should you see a doctor?
Pituitary adenoma is accompanied by endocrine disorders, which always cause negative symptoms. Be sure to make an appointment with your doctor if you experience weight loss or gain without changing your diet, blurred vision, changes in the appearance of the skin, headaches, or sexual dysfunction. You will be prescribed a series of tests, based on which a specialist will make an accurate diagnosis. The sooner you contact a medical clinic, the sooner you will receive a conclusion, the shorter and more effective the treatment will be.
First appointment with a therapist. Next, based on complaints and examination results, the specialist will write a referral to a specialized doctor. Women are examined by a gynecologist-endocrinologist, men by an andrologist. Consultations with doctors of other specializations may be required.
The MedCom clinic in Ryazan has everything necessary for the diagnosis and treatment of pituitary adenoma. Experienced doctors will conduct an emergency examination and develop the most effective and safe treatment regimen. Make an appointment by calling +7 (4912) 77–92–02 or using the online contact form. Do not delay your visit to the doctor - pituitary adenoma can be successfully treated in the early stages!
General symptoms of the disease
Advertising:
Each type of hormonal active adenoma manifests itself with specific symptoms, since during their development the production of a certain hormone is disrupted. But there are a number of general signs indicating the possible development of a pituitary adenoma, these are:
- Visual impairment
. It occurs due to compression of the optic nerves by a growing formation, which leads to disruptions in the transmission of signals from the analyzers to the cerebral cortex. In most cases, the pathology leads to loss of lateral visual fields. - Headache
. Cystic formation negatively affects the functioning of adjacent structures and leads to increased intracranial pressure. - Dizziness, weakness, fatigue
. These symptoms are associated with the effect of the tumor on nerve tissue.
Microadenomas are benign neoplasms, so there are usually no symptoms of intoxication, weight loss, or loss of appetite when they appear.
Rashes on the head of the male genital organ appear as a result of certain diseases or a number of external circumstances. Uncharacteristic changes in the skin require treatment, the plan of which may include medications and a number of medical procedures. Read more in the article: “rash on the head of the penis.”
Biological behavior and follow-up
There are functioning (3/4 of all adenomas) and non-functioning (1/4 of all adenomas) adenomas. Microadenoma, in the overwhelming majority, is a functioning tumor and, clinically, is manifested by signs of hormonal disorders and associated symptoms. Macroadenomas are more often non-functioning (but may also be hormone-producing), as a result of which they grow latently (clinically, without manifesting themselves in any way), and reach large sizes, discovered during an examination for focal and cerebral symptoms (visual disorders, increased ICP and etc.).
Nonfunctioning adenomas are usually present in patients with delayed puberty, short stature, or primary amenorrhea (in girls) [137].
The morphological structure of the tumor does not correlate with the type of hormone produced. However, prolactinomas and somatotropinomas are more often located in the lateral parts of the adenohypophysis, and adenomas secreting ACTH, TSH and FSH (LH) in the middle [2].
There are also some indirect signs associated with secondary endocrine changes. For example, a secondarily elevated level of GH leads to acromegaly (thickening of the skull bones, widening of the lower jaw on images), an increased level of ACTH leads to pathological compression fractures and “buffalo hump” back deformities [48].
Statistically, prolactinomas are most often found - 1/2 of endocrine active adenomas and 1/3 of all adenomas.
Among active adenomas, in descending order of frequency of occurrence, there are:
- prolactinomas (48%),
- somatotropinomas (10%),
- corticotropinomas (6%),
- thyroprolactinoma (1%),
- adenocarcinoma,
- mixed and non-secreting (35%) [175].
Large and nonfunctioning tumors can also disrupt hormonal balance. Hypopituitarism or moderately elevated prolactin, in both cases, is visible due to the so-called “crossing the stem” effect; Prolactin (unlike other pituitary hormones) is suppressed by a prolactin-inhibitory hormone (such as dopamine) and, if the pituitary infundibulum is compressed, can lead to elevated systemic prolactin levels due to interruption of normal inhibition of secretion [45].
Incidentaloma is an adenoma without any clinical manifestations; more often, these are non-functioning microadenomas (2-30% of adenomas), which attract attention, can be misinterpreted, and may not be justifiably subjected to unreasonable treatment.
An increased level of prolactin over 100-150 nm/ml is a sign of prolactinoma; with lower values of plasma prolactin, there is probably another reason: a tumor of the hypothalamus, drugs (phenothiazines), hypothyroidism and extraglandular hyperprolactinemia (liver, APUD system), physical activity, breastfeeding, nipple stimulation and recent sexual intercourse. ACTH may be ectopically produced in small cell lung cancer [193].
Malignant prolactinomas are extremely rare and cannot be determined either histologically or by imaging, but only retrospectively, starting from the presence of distant metastases [46]. Anaplastic adenoma and pituitary cancer are rare and develop mainly after long periods of relapse and repeated courses of complex treatment [193].
Morphology and localization
Pituitary adenomas, depending on their size, are divided into micro- (up to 1 cm) and macro-adenomas (more than 1 cm in diameter). Microadenoma is a lesion located entirely within the pituitary gland.
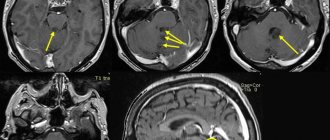
Direct signs of the presence of microadenoma:
- volumetric education,
- often hypointense on T1,
- T2 hyperintense or hypointense.
Indirect signs:
- funnel displacement,
- dredging,
- increase in the size of the pituitary gland,
- bulging of the superior contour of the pituitary gland.
In the absence of signs of microadenoma, its presence cannot be rejected without resorting to a study with dynamic contrast.
Using CT to diagnose microadenomas is not objective: bone artifacts and low tissue contrast. MRI is used exclusively. In cases with macroadenomas, CT is not replaceable for differential diagnosis.
Fig. 1549-1541
Microadenoma in the right half of the pituitary gland (arrowheads in Fig. 1549, 1550), which has relatively clear and even contours, is well differentiated by T2 (Fig. 1549) and a weakly hypointense MR signal by T1 (Fig. 1550). Bulging of the upper contour of the pituitary gland (arrow in Fig. 1551) is also a sign of pituitary microadenoma.
Fig.1552-1554
Also, signs of the presence of a microadenoma are a deepening of the bottom of the sella turcica (arrowhead in Fig. 1552), a clearly heterogeneous structure of the gland (arrows in Fig. 1552, 1553) and displacement of the funnel in the direction opposite to the microadenoma (arrow in Fig. 1554).
Assessing cavernous sinus invasion can be difficult. The most convenient way is to assess the extent of coverage of the cavernous part of the internal carotid artery. Less than 90 degrees makes sinus involvement very unlikely, while coverage greater than 270 degrees almost certainly indicates cavernous sinus involvement [45].
Invasion of the dural sinuses often leads to a direct release of the hormone from the functioning adenoma into the blood, which is manifested by an increase in the level of the hormone in the blood, for example, a convincing sign of prolactinoma of the pituitary gland invading the cavernous sinus is a prolactin level over 1000 ng/ml [2].
Invasion of adjacent structures occurs in 35% of cases and is not evidence of malignancy [48].
Fig. 1555-1557
Pituitary adenoma with invasion into the right cavernous sinus (arrow heads in Fig. 1555, 1556), which is well differentiated on contrast-enhanced MRI (arrowhead in Fig. 1557).
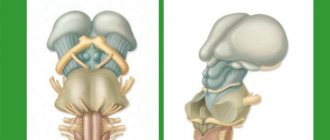
Macroadenoma is a large formation of the chiasmal-sellar region with an expansive type of growth and expansion of the sella turcica of the skull (the change is noticeable on the craniogram).
Extrasellar spread can occur in any direction, accordingly, indicated by the type of growth:
- suprasellar,
- antesellar,
- retrosellar,
- infrasellar,
- laterosellar.
It may spread in several directions at once.
Adenomas with a suprasellar growth pattern have a typical “dumbbell” or “8” appearance, which is explained by the tumor passing through the diaphragm of the sella turcica [48]. On MRI they are usually isointense to gray matter on T1 and hyperintense on T2 [72]. On CT, macroadenomas have a density of 30–40 HU [114].
Fig.1558-1560
Pituitary macroadenoma with a suprasellar type of growth (asterisk in Fig. 1558) in the form of a large formation above the sella turcica, compressing the chiasm and the third ventricle. Adenoma with a suprasellar type of growth (asterisk in Fig. 1559) and fouling of the siphons of the carotid arteries (arrowheads in Fig.). Macroadenoma with a retrosellar type of growth (arrowheads in Fig. 1560).
As it grows, it spreads to the sides, the tumor causes destruction of the bone structures of the sella turcica, and can also be complicated by liquorrhea.
If it reaches a large size, macroadenoma can even cause indirect compression of the foramina of Monroe and lead to occlusive hydrocephalus. Large lesions are often heterogeneous and vary in signal due to areas of cystic change, necrosis, and bleeding [115].
Fig.1561-1563
Macroadenoma with a laterosellar type of growth to the left from the area of the sella turcica (asterisk in Fig. 1561). Laterosellar spread to the right, and coverage of the cavernous segment of the right internal carotid artery (arrows in Fig. 1562). Destruction of the apex of the pyramid of the right temporal bone and the sphenoid bone, in the process of spreading of the pituitary adenoma, into the right middle cranial fossa (arrows in Fig. 1563).
Fig.1564-1566
Pituitary adenoma with growth into the sinus of the main bone (asterisk in Fig. 1564). Deepening of the bottom of the sella turcica due to bone atrophy and restructuring caused by the growth of adenoma (arrows in Fig. 1565). A giant macroadenoma with extensive distribution in several directions (arrowheads in Fig. 1566).
Bone destruction
In the process of expansive growth, macroadenoma leads to atrophic changes in the bone structures of the sella turcica, which at first looks like its expansion, and then like the absence of the back, inclined processes and the upper wall of the sphenoid sinus.
Fig. 1567-1569
Cystic adenoma
Cyst-shaped adenoma with expansion of the sella turcica (asterisk in Fig. 1567, 1568). The heterogeneous structure of the pituitary adenoma on CT is revealed due to the difference in density characteristics and, with contrast enhancement, objectively demonstrating the heterogeneity of the tumor (Fig. 1569).
Fig.1570-1572
A pituitary macroadenoma can be suspected by the expansion of the sella turcica during tumor growth (asterisk in Fig. 1570). CT gives a complete picture of the state of the bone structures of the base of the skull, which reflects a significant expansion of the pituitary fossa (asterisk in Fig. 1571), thinning of nearby bone structures (arrow in Fig. 1581) and disappearance of the dorsum sella (dotted line in Fig. 1571 and Fig. .1572).
Cystic degeneration occurs in 18% of cases, calcification is not typical [48].
Fig. 1573-1575
Cysts are found in the tumor stroma, which are limited areas with homogeneous liquid content, which is a reflection of dysmetabolic degenerative changes (arrows in Fig. 1573-1575).
Hemorrhagic adenoma
Macroadenomas are diagnosed as cysts containing blood, which is divided into phases depending on the specific gravity (separation of the contents into phases with different densities, in this case, plasma and formed elements - the effect of sedimentation). The presence of sedimentation effect is a specific sign of cystic degeneration [2].
Fig.1576-1578
Hemorrhage in the cavity of a cystic macroadenoma, with visualization of the level of sedimentation of formed elements and the liquid part of the plasma (arrows in Fig. 1576, 1577, 1579). Macroadenoma (asterisk in Fig. 1578) has a supra- and infrasellar distribution, compressing the chiasma and deepening the sella turcica (arrows in Fig. 1578, 1580, 1581), as well as laterosellar (arrowhead in Fig. 1578).
Fig. 1579-1581
Fig. 1582-1584
Hematoma in the left half of the adenoma (arrows in Fig. 1582, 1584), having an MRI signal in T1 (arrow head in Fig. 1583) and T2 (arrow in Fig. 1583).
There may be hemorrhage into the adenoma (apoplexy of the adenoma), reflecting convincing tumor invasion of the cavernous sinus, but this is not a hemorrhagic adenoma.
Features of the development of microadenoma
The pituitary gland is one of the endocrine glands. It is located at the base of the brain and is responsible for metabolic processes, human growth and physical development. Microadenoma is understood as hyperplasia (growth) of individual areas of the pituitary gland, which generally leads to an enlargement of the entire gland. The neoplasm most often occurs in women between 20 and 40 years of age, although it is also often diagnosed in children and adult men. Many doctors believe that its development in women is facilitated by hormonal changes associated with bearing a child and breastfeeding.
Microadenoma is a tumor no more than 1 cm in diameter.
Microadenomas are benign formations, but untreated disease can lead to a significant deterioration in quality of life.
It begins to grow most often in the anterior portion of the pituitary gland - the adenohypophysis. The formation of hormones itself does not produce hormones, but can lead to their excessive production or, conversely, to a decrease in secretion.
Advertising: