Mnestic activity is the ability of the brain to record, remember any information, and reproduce it at the right time. The human brain has a well-developed ability to reproduce facts and events accurately.
But some people experience mental disorders. Why this happens and how to correct them will be discussed in the article.
Mnestic activity of man. Peculiarities
Mnestic activity is the work of the cerebral cortex aimed at the perception, systematization and sequential reproduction of information. Only humans have the ability to remember information that is not related to the direct perception of the world through the senses. However, it is feelings that are associated with attention.
The human brain constantly perceives and analyzes the incoming stream of signals. But as conscious beings, we can selectively fix our attention on the necessary areas of knowledge and remember abstract statements that do not have visual properties.
Processes of mnestic activity. Stages
The memorization process sequentially goes through several stages.
- Recognition of the material. It takes careful reading or listening to the material to leave some kind of trace in the brain.
- Then this trace must be fixed through volitional efforts.
- Systematization, when new knowledge is superimposed on existing knowledge in different brain structures and assimilated. At the same time, those blocks that do not correspond to previously learned material and marked as important, that knowledge is erased. This is necessary to ensure that internal “failures” do not occur in the playback system.
- Playback. The material that has been successfully integrated into the overall picture of the world built by the brain is securely stored in long-term memory.
It takes quite a lot of time to process new information. Few people have phenomenal mnestic abilities to quickly grasp and remember something forever. The brain also spends an incredible amount of energy.
The peculiarity of mnestic activity is that the perception mechanism is always at work. But for new neural connections to form, the body must have enough protein and neurotransmitters: dopamine, serotonin. In addition, you need at least 8 hours of sleep so that the brain is rested and can also successfully concentrate on systematizing what it has learned.
What are mnestic processes?
Human knowledge arises as a result of mnestic activity. Which has the goal of memorizing the relevant material in order to reproduce it later. Mnestic processes are those that occur in human memory and consist of the following stages:
- memorization is a process that ensures the retention of imprinted information; in the scientific sense it is divided into intentional and unintentional;
- preservation - during this process, the acquired information is transformed in different ways: by building associations, that is, assimilating the received material with what was already known and by interference, when the old material is improved due to its actualization;
- reproduction is a procedure that embodies and actualizes phases of existing experience (ideas, sensations, thoughts, feelings);
- recollection is a process that in theory is often not separated from the process of reproduction, but it should be noted that it is associated with an effort aimed at extracting images from long-term memory;
- recognition - fixation of an object of objective reality or phenomenon as previously familiar, establishment of associative connections between the observed and the preserved idea of it;
- forgetting - loss of the ability to reproduce, and sometimes even recognize, what was previously learned; Usually it affects something that is of little significance; can be partial or complete, and also vary in duration.
You may be interested in: Charles II: date of birth, biography, reign, date and causes of death
You may be interested in: The concept of holistic marketing, its types
The combination of “attentive-mnestic processes” is also often mentioned in the specialized literature. In these cases we are talking about the processes of attention and memory. As you know, they are very closely interconnected.
You will be interested: Dmitry Milyutin: date of birth, biography, military career, reform in the army
Types of memory. Short-term and long-term memory
Mnestic activity is a special brain activity that allows you to learn to keep large amounts of information in your head for a long time; operate with concepts.
Memory is divided by modality into motor, emotional, figurative, verbal-logical. There is also a division into voluntary and involuntary.
Based on storage duration, memory is divided into instantaneous, short-term and long-term, or indefinite. Information that enters short-term memory, with constant fixation of attention on this material and repeated repetition, passes into long-term memory.
Mechanisms of regulation and imprinting
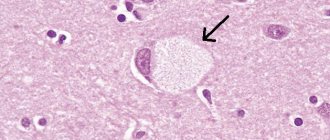
The recording of new information goes through three stages in time: initially, based on the work of the visual, auditory and tactile analyzers, an engram is formed, that is, a special trace in the iconic memory. At the next stage, the available data is sent to the higher authorities of the brain. In certain cortical structures and parts of the limbic system, the incoming material is analyzed and sorted.
It is known that the hippocampus acts as a kind of filter, classifying all this and discarding what is unnecessary, and the task of the temporal region is to establish relationships with areas where engrams are stored from other parts of the brain. At the last stage, all this is translated into a clear circuit of long-term memory.
Intellectual-mnestic activity
Memorization is closely related to intellectual activity. And by training the intellect, we thereby develop memory.
Mnestic activity is the ability to learn new things and adapt to a changing reality. If you work in one job for many years and fulfill standard requirements, your intelligence decreases. A person must constantly study something, be interested in new trends in science, and have a developing hobby.
Children under 5 years of age develop very quickly. Their consciousness does not differentiate the incoming flow of information into “bad” and “good”, “profitable” and “unprofitable”. They perceive absolutely everything.
For the development of mnestic activity in children, it is important to communicate with them in a playful way. It is the game that develops intelligence, not memorization.
Mnestic activity is development. As soon as a person stops training his intellect and establishing new connections between neurons, the aging mechanism of the brain and the whole organism is triggered.
Types of intellectual and mnestic disorders
The classification is based on dysmnesia, which includes:
- hypermnesia - the inability to distinguish main events from secondary ones with increased memorability;
- hypomnesia - weakening of memory in general;
- retrograde amnesia – loss of memories preceding the onset of the disease;
- fixation amnesia – shutdown of short-term memory;
- progressive amnesia - gradual erasure of memory.
The main symptom of these diseases is the degradation of the mental and mnestic abilities of the individual.
Korsakov's syndrome
In Korsakoff's syndrome, the ability to retain memories of the immediate past disappears, but long-term memory is not affected.
The patient fills gaps in memory with his own fantasies and fiction. The person turns out to be unadapted to the current situation: he cannot name the day, hour and location of his location, with whom he recently communicated and about what. Apathy, irritability, and fatigue are characteristic signs of patients with Korsakoff amnestic syndrome.
Most often, this syndrome affects elderly people, patients after a stroke, intoxication, head and brain injuries, and delirium. In the absence of organic damage to parts of the brain, restoration of short-term memory is possible.
Dementia syndrome
Dementia is a progressive dementia in which a general weakening of memory occurs, speech is distorted, motor functions are impaired, and self-control and adaptation skills are lost.
Depending on the area of damage to the brain, atrophic, vascular or mixed forms of dementia develop, of varying degrees of severity, in the form of total (complete disappearance of intelligence and personality) or lacunar (decreased intelligence with preservation of personality) dementia.
Atrophic dementias are diseases called “senile insanity” and are progressive and incurable. They end in personality disintegration (Alzheimer's disease), disability (Parkinson's disease) or personality changes (Pick's disease). The age of patients is from 50 to 65 years. Drug addiction and alcoholism can lower the age limit.
In patients with vascular dementia, against the background of fixation and progressive amnesia, lacunar dementia develops, accompanied by apathy, lethargy, unsteady gait, and urinary incontinence.
Psychoorganic syndrome
Psychoorganic syndrome means mental weakness, expressed in weakening of memory, loss of will and intelligence, and emotional instability. The disease can develop at any age, but predominates in the elderly, which is associated with atrophic changes in the brain.
There are four types of syndrome, all part of the same progressive process:
- asthenic is unstable behavior and an inadequate reaction to ordinary events and things that deplete the patient’s neuropsychic and physical strength, without reducing mental abilities;
- euphoric - complacent, fussy stupidity, with explosions of malice and anger, turning into a depressive-tearful state;
- with the explosive variant, the signs of the first two types are supplemented by weakening of will, memory impairment and craving for alcohol;
- in the case of the apathetic variant, there is a sharp decrease in memory and intelligence, lack of will and indifference to what is happening.
Patients with organic psychosyndrome are meteodependent, and the more stable this connection is, the less the degree of brain damage. There are also acute and chronic forms of encephalopathic syndrome.
Children of any age can suffer from this intellectual and mnestic disorder, which is associated with a violation of the formation and development of the child’s brain. A long period of speech development, impulsiveness, restlessness, inattention, overestimation of one’s abilities are signs of an emerging psychosyndrome.
Congenital forms of dementia
Oligophrenia is a congenital dementia caused by hereditary, external factors or a combination of them. Today, about 300 hereditary diseases are the cause of mental retardation. Down's disease and microcephaly are a consequence of genetic pathology.
Oligophrenia has three stages:
- Moronism is a mild degree of mental and mental disability, in which the development of an adult corresponds to 12 years of age.
- Imbeciles remain for life at the level of a 3-7 year old child. Their speech is primitive, but understandable. The behavior is not aggressive.
- Idiocy is total dementia, in which a personality is not formed, the mental abilities correspond to a 3-year-old child, constant care and control of behavior are required.
Relationship between attention, intelligence and memory
The processes of mnestic activity are determined by the ability to voluntarily maintain attention on one object. Attention is a program that ensures that information that needs processing is retained in the field of consciousness. Weak control of attention is the key to the fact that it is difficult for a person to remember facts; even with good intelligence, he will not be able to achieve success in his profession.
Also with low intelligence. Even good attention, the ability to focus for a long time on one object will not help develop good memory if the intellect is poorly developed.
Memory research methods
As has been said, memory can be voluntary or involuntary; and by shelf life - short-term and long-term. To study the properties of involuntary memory, subjects were asked to do light work. And upon completion of its implementation, they were asked to tell about the main stages, about what was remembered most vividly.
Short-term memory is studied in more detail. The subjects are tested for the ability to remember objects of different modalities and for the duration of retention of this information. The amount of short-term memory is also important. Each subject has special properties. But research allows us to identify general patterns - why we remember some thoughts and facts well, and why we forget others.
The classic method for studying memory was invented by psychologist Hermann Ebbinghaus. To test memory, he suggested using syllables that were absolutely meaningless. The inability to make any associations or apply one’s intellectual abilities makes it possible to determine the pure amount of “technical memory”. That is, that reservoir in the brain where information is stored only for some urgent task.
The social significance and high prevalence of epilepsy contributed to the establishment of epileptology as an independent discipline. The chronic, progressive course of epilepsy is aggravated by the formation of mnestic-intellectual disorders, the negative impact of which on the social adaptation of patients is not inferior to the negative consequences of paroxysmal syndrome [7, 8].
Epilepsy is considered a highly disabling disease that causes stigmatization of patients in society. It is stigma that many consider an obstacle to improving the quality of life, which has a significant impact on personality, mood and behavior [3, 15, 16, 20].
The cognitive ability of patients with epilepsy is influenced by many factors, including the etiology of the disease, the type and frequency of seizures, the age of the patients at the time of their onset, as well as hereditary and psychosocial influences.
The final effect of antiepileptic therapy [21], since the peculiarity of treatment is the need for many years, sometimes lifelong use of antiepileptic drugs, which in 7-25% of cases lead to side effects and complications.
Recently, much attention has been paid to studying the influence of functional interhemispheric asymmetry on the nature of the ongoing process in patients with neurological and mental disorders - psychoses [4, 6, 18], various forms of deviant behavior [17, 22, 24-27] and with epilepsy itself [ 5, 9, 13]. Most authors come to the conclusion that lateralization is impaired in all of the listed types of pathology. To the above, we can add that interhemispheric asymmetry often determines the characteristics of the course of the disease and the effectiveness of therapy. Suffice it to say that among patients with schizophrenia and epilepsy, left-handed people are 2-3 times more likely than in the healthy population, and they mostly have severe forms of the disease [5, 23]. In addition, there is evidence that the processes of compensation and adaptation, as well as the course of the disease in right-handers and left-handers with damage to the ipsi- and contralateral hemispheres proceed differently [1, 19]. The effectiveness of therapy in epilepsy patients with right, left and mixed individual profiles of functional asymmetry also differs [13].
In this regard, the relevance of this study was determined by the high medical and social significance of the development of mnestic-intellectual disorders and the insufficient knowledge of the problem taking into account functional asymmetry.
The purpose of the study was to establish the pattern of formation of cognitive impairment in patients with epilepsy, taking into account the influence of the basic characteristics of the epileptic process and functional asymmetry.
Material and methods
We examined 132 patients (70 women and 62 men, aged 16 to 50 years; average age 27.8±8.9 years) who were treated in a specialized epileptology hospital at the Moscow Research Institute of Psychiatry. The main group consisted of 112 patients with cognitive disorders, the control group - 20 patients with epilepsy without cognitive disorders. The second control group included 20 healthy people, comparable in demographic indicators and level of education to the main group.
The work used clinical-psychopathological, psychometric, neurointroscopic, neurophysiological and statistical methods. When determining the form of the disease and the structure of the leading paroxysmal syndrome, the modern classification of epilepsy (New Delhi, 1981) and epileptic seizures (Kyoto, 1981) was used. To assess the profile of functional asymmetry, a set of techniques was used aimed at identifying preferences in the motor and sensory spheres [14]. Leading importance was attached to the motor sphere.
The level and structure of intelligence were assessed using the neurocognitive tests WAIS (Wechsler Adult Intelligence Scale) and the MMSE scale (Mini-Mental Test Examination). The NHS3 scale (National Hospital Seizure Severity Scale) was used to quantify neurological level disorders; Personality-psychopathology disorders were assessed using the Clinical Self-Esteem Scale (SCL-90) and the Munich Personality Test (MPT).
In accordance with the results of the clinical-psychopathological examination and cognitive tests, 3 subgroups of patients were identified in the main group according to the degree of intellectual impairment: subgroups of cognitive defect, borderline level and average level of intelligence.
In accordance with the ICD-10 criteria, these disorders corresponded to the headings: F-02.8 “Dementia”, F-06.7 “Mild cognitive impairment”. According to the division of dementia by severity [10], the subgroup of cognitive defect corresponded to moderate dementia, and the borderline subgroup corresponded to mild dementia. Let us dwell on these categories of disorders in more detail.
Dementia of moderate severity.
A cognitive defect consistent with dementia was observed in 17 (15.1%) patients. This subgroup includes patients with a general intelligence level below 69 points on the WAIS scale, with a pronounced mnestic-intellectual defect. Clinically, the cognitive defect was manifested by a significant decrease in memory (direct, indirect) and concentration, difficulties in generalization, switching, abstraction, and prediction. The pace of thought processes, counting operations and orienting-search reactions are also sharply slowed down, and for some patients they are inaccessible. Associative products are thorough, detailed, judgments are primitive, with a tendency to form super-valuable experiences. Criticism of their condition and behavior was sharply reduced; most patients in the group could not live without outside help. All of the above as a whole significantly complicated the perception of new material and comprehension, or made it impossible.
Mild dementia.
A borderline level of intellectual decline was detected in 37 (33.0%) patients. This subgroup includes patients with an intelligence level from 70 to 89 points on the WAIS scale, with a fairly pronounced mnestic-intellectual decline. What distinguished them from the patients of the previous subgroup was the possibility of independent living and self-care without restrictions. Clinically, the subgroup is represented by patients with decreased memory and attention functions, a slower pace of thought processes, but to a lesser extent than in the subgroup of cognitive defects. A decrease in the level of generalization and abstraction is characteristic. Thorough thinking, with difficulty switching. Most patients can develop simple new skills.
Mild cognitive impairment
was observed in 58 (51.78%) patients, with a general intelligence level from 90 to 109 points on the WAIS scale. The subgroup was characterized by a slight decrease in the cognitive sphere or its individual functions, which in most cases was detected only when using cognitive tests. Against the background of a slight slowdown in the pace of thinking and memory within normal limits, instability of attention was noted. Generalizations took place at the categorical level. The associative products are adequate, somewhat detailed, and emotionally charged. In the clinic, cerebrasthenic symptoms and emotional disturbances in the form of mood swings and dysphoric reactions came to the fore.
results
The cognitive sphere of patients with epilepsy is reduced with a high degree of reliability in comparison with the control group (Table 1).
The mnestic-intellectual functions of patients with moderate dementia are almost 2 times lower than in the control group of patients without cognitive disorders (63.0±6.7 and 112.7±4.6 points, respectively, t=–18.7; p=0.0000), and were formed to a greater extent due to verbal indicators: awareness, social orientation, counting, definitive thinking and memory.
The intellectual sphere of patients with mild dementia was significantly reduced, but to a lesser extent than in the group with moderate dementia (82.9±4.6 points, t=–16.2; p=0.0). The general level of intelligence of the borderline group, like the group of cognitive defects, was formed due to verbal functions: awareness, social orientation, abilities to understand idioms and generalization, and definitive thinking.
In patients with mild cognitive impairment, the intellectual domain was slightly reduced compared to controls (99.7±5.7 and 112.7±4.6 points, respectively). It was uniformly formed due to all verbal and non-verbal indicators, in contrast to the subgroups of cognitive defect and borderline level, where only verbal functions were manifested. Thus, patients with mild cognitive impairment were distinguished by the harmonious development of the intellectual sphere, despite its decline.
The data from Wechsler's cognitive technique were confirmed by the results of the MMSE test.
Analysis of the characteristics of the epileptic process influencing the appearance of cognitive disorder revealed the following factors to be of greatest importance.
1. Patients with moderate dementia were distinguished by the presence of diffuse slow-wave activity on the EEG with bilateral synchronous flashes, indicating dysfunction of the mid-brain structures, while the amplitude accent in the left temporal region led to a significant decrease in cognitive functions (p<0.05).
Patients with mild dementia were characterized by the presence of less pronounced diffuse slow-wave activity and the absence of bilateral synchronization, which, according to the results of cognitive tests, had a positive effect on their intellectual level. At the same time, the presence of focal epileptiform activity in the left frontotemporal region led to a statistically significant decrease in cognitive functions (p<0.01). Similar focal epileptiform activity, but with a focus in the right temporal region, correlated with mild cognitive impairment (p < 0.005).
2. The age of onset of seizures had a great influence on the cognitive sphere. In moderate dementia, the minimum values according to the Wechsler test were observed in patients with the onset of seizures before the age of 5 years (p <0.03). In mild dementia and mild cognitive impairment, the minimum Wechsler test score was observed in patients with the onset of seizures between the ages of 11 and 15 years (p=0.009 and p=0.0003, respectively).
3. The duration of the disease had an ambiguous effect on the cognitive sphere. In groups with cognitive impairment, as the age of onset of seizures increased (from 3.8 years for moderate dementia to 13.8 years for mild cognitive impairment), the duration of the disease decreased (from 21.9 to 13.3 years). At the same time, in the control group of patients without cognitive disorders at the latest age of onset of seizures (16.6 years), the duration of the disease corresponded to the group with dementia (Fig. 1).
Figure 1. Average values of the age of onset of seizures and duration of epilepsy in the study and control groups (years). This may be due to the characteristics of the premorbid level of intelligence and the degree of brain maturity at the time of the onset of the disease. It has been established that in patients with premorbidly high intelligence, a decrease in cognitive functions is detected to a lesser extent, later and is better compensated [2, 11].
Thus, when assessing the impact of the duration of the disease on the cognitive sphere, it is necessary to consider it in relation to the age of onset of seizures.
Among other factors of the epileptic process, the following had a significant impact on the cognitive sphere: high frequency of seizures (more than 1 per week), seizures with secondary generalization, and symptomatic form of epilepsy.
In accordance with the objectives of the study, the cognitive sphere of patients with epilepsy was studied taking into account functional asymmetry, in particular its motor component.
In the main group of patients with cognitive disorder, 14% of patients with left-sided motor asymmetry were identified. The first control group (patients with epilepsy without cognitive impairment) was entirely right-handed. The second control group (healthy) included 5% left-handed people.
Patients with epilepsy with left-sided motor asymmetry were distinguished by a heterogeneous structure in the genesis of handedness with compensatory and hereditary causes.
In 37.5% of patients with left-sided motor asymmetry, the following factors were identified in the anamnesis: pathology of childbirth with fetal extraction, complicated otolaryngological diseases, traumatic brain injury and infectious diseases of the brain with the formation of right-sided paresis. A nuclear magnetic resonance imaging scan of the brain in the left hemisphere showed organic changes of a cystic-atrophic nature in all of them. Due to these factors, patients were classified into the group with compensatory or pathological left-handedness.
The majority of patients (62.5%) were in the group of genetically fixed left-handedness due to hereditary conditions. Among the analyzed group of patients with epilepsy with left-sided manual preference, not a single case of sociocultural or environmental left-handedness was identified, which was a consequence of social upbringing, living conditions or imitation of relatives.
Patients with left-sided motor asymmetry had the greatest depth of cognitive impairment compared to right-handed patients. The proportion of dementia disorders among left-handed people reached 70%, among right-handed people - 45% (Fig. 2).
Figure 2. Distribution of cognitive disorders by severity, taking into account functional asymmetry.
The intellectual sphere of patients with epilepsy with a dominant left hand was characterized by a significant decrease due to a sharp deficit in nonverbal indicators (Table 2),
and also due to males (Table 3)
The level of intelligence of left-handed men was statistically significantly different from right-handed men (77.2 and 91.3 points, respectively, p = 0.006); among women, the differences did not reach a statistically significant level.
In the structure of the intelligence of patients with left-sided motor asymmetry, a deficit was found in both verbal (counting, p = 0.007; memory, p = 0.02; definitive thinking, p = 0.04) and non-verbal indicators (synthetic abilities, p = 0.01 ; hand-eye coordination, p=0.02; attention, p=0.02).
Analysis of factors in the formation of a cognitive defect, taking into account motor asymmetry, established the following patterns.
1. The early age of onset of seizures (before 5 years) and the duration of the disease (more than 20 years) in right-handed patients determined a significant decrease in cognitive functions, which was not confirmed in left-handed patients.
2. Focal epileptiform activity of the brain in the left temporal region led to a decrease in cognitive functions in right-handed patients and an increase in them in left-handed patients. A decrease in cognitive functions in patients with a dominant left hand was determined by the presence of diffuse slow-wave activity with the inclusion of bilateral synchronous discharges with an amplitude accent in the frontal region.
3. Taking barbiturates and clonazepam, as well as the factor of polytherapy with anticonvulsants, led to a significant decrease in cognitive functions in right-handed patients, in contrast to left-handed patients.
4. The prescription of antipsychotics led to a decrease in mnestic-intellectual functions in right-handed people, which was not confirmed in left-handed people.
Meanwhile, in women, the factor of left-handedness correlated with the duration of remission (p=0.0001, t=4.02). The average duration of remission in women with the dominant left hand was 3.93±5.15 years, with the right hand - 0.66±1.24 years. This allows us to consider left-sided motor asymmetry in women as a predictor of a prognostically favorable outcome of therapy in relation to paroxysmal syndrome.
Discussion
The study showed that a number of factors take part in the formation of mnestic-intellectual decline (defect). In this case, the defect can form both as a result of brain damage and epileptic activity itself, and as a result of the negative effect of antiepileptic therapy. Among the leading risk factors are the younger age of patients at the time of the onset of the disease, the high frequency of seizures (more than 1 per week) and their secondary generalization; Long-term neuroleptic therapy, especially clonazepam and barbituric drugs, significantly aggravates the development of cognitive defect. Studying the profile of lateral organization taking into account gender makes significant adjustments to the understanding of the formation and course of cognitive decline in epilepsy. The revealed influence of left-sided motor asymmetry on the formation of a pronounced intellectual defect is apparently due to a decrease in the right hemisphere functions of the brain, which manifests itself to a greater extent in men. It is likely that the left-sided profile of brain asymmetry is an unfavorable prognostic factor in relation to the cognitive sphere. At the same time, in women it contributes to the formation of remission of paroxysmal syndrome. It is obvious that work on studying the relationship between the asymmetry profile and various manifestations of epilepsy, including intelligence, should be continued.
Memory impairment. Causes
When a person during a study cannot remember 4 objects or words out of 10, researchers can note disturbances in mnestic activity. The causes of memory failures can be physiological or psychological.
Let's try to understand the cause-and-effect relationships that lead to a deterioration in the ability to perceive, analyze and remember information^
- Exhaustion of the nervous system due to stress or neurosis.
- Severe damage to the frontal lobes of the brain due to injury or stroke.
- Consequences of infectious diseases (meningitis, arachnoiditis) affecting the structure of the brain.
- Affective-emotional instability.
- Congenital brain abnormalities. Such as schizophrenia, childhood autism or dyslexia.
- Inability to regulate attention, lack of focused effort.
Functional memory disorders, which are based on prolonged neurosis or attention disorders, are treated with the help of a psychologist. But more serious disorders require long-term treatment. Moreover, late treatment often leads to the fact that it becomes impossible to eliminate the disorders.
Disturbances of mnestic processes
Pathology research is carried out, as a rule, in 3 areas:
- clinical;
- neurophysiological;
- psychological.
Memory pathologies in general can be depicted as two separate groups - quantitative (dysmnesia) and qualitative (paramnesia) disorders. The first include such as hypermnesia, amnesia, hypomnesia, and the qualitative ones include false memories, contamination, jamevu or pseudo-reminiscence.
The most famous memory disorder, often mentioned in films and books, is amnesia. It comes in different types; they are united by a common inability to reproduce previously acquired knowledge, experienced events, or remember new material.
Dyslexia due to memory impairment in children
Impaired memory of words and objects, difficulties with speech in early childhood may be associated with dyslexia. This is a special disorder of mnestic activity associated with a congenital anomaly in the region of the language center of the brain.
With this syndrome, the child experiences difficulty perceiving speech and dividing the flow of sounds into its component parts. Naturally, the development of memory and thinking in such children is slowed down. Studies of mnestic activity in children show that working with them, communicating, and pointing out errors of perception contribute to recovery from the syndrome.
It happens that the cause of difficulties in mastering writing is associated with visual-perceptual disorders.
Correction
Problems with memory have a negative impact on your studies and career. What can you do to improve your memory? There are several methods for correcting mnestic activity:
- If a person works with information, he needs to constantly get enough sleep.
- Take breaks during the learning process. The brain needs to rest and “reboot.”
- Organize material to make it easier to comprehend and remember. Build tables, pictures, diagrams.
- Use associations when learning.
- Remember more often the poems you taught at school.
To improve memory ability, it is recommended to take brain vitamins. These are Omega-3, glycine, all B vitamins.
If there are serious disturbances in the functioning of the cerebral cortex due to injury, more serious chemicals and treatment under medical supervision are required.
Classification according to the nature of mental activity
Individual characteristics of mnestic processes are characterized by what material is best absorbed: figurative, verbal, or both equally:
- Figurative memory. This is the ability to perceive and retain in memory certain visual images (ideas, pictures from life) and subsequently reproduce them; the type of memory is determined by a set of modality-specific sensations. This memory is plastic, can be long-term and appear unexpectedly. It is believed that its structure is made up of complex connections of neuronal units from different parts of the brain.
- Emotional memory. This type of memory is the result of fixations and new manifestations of emotional experiences; simply put, it is a memory for feelings. An impression that contains an emotional coloring is remembered instantly and without volitional effort, thus replenishing the structures of the human subconscious. This is a very stable mnestic type, the material of which can be reproduced completely involuntarily. Its biological basis presumably contains connections that combine subcortical neuronal links with links in different parts of the cerebral cortex.
- Semantic memory. This mnestic process correlates with the imprinting of verbal signs symbolizing what is happening in reality and internal experiences. Schematically, it represents series-connected linear links. If one of the links suffers, then this is fraught with a break in the entire chain, failure of the correct alternation of stored realities and erasing of certain fragments from memory.
Traditionally, the mnestic sphere is divided into 3 classic temporary types of memory:
- Iconic.
- Short-term (operative).
- Long-term (declarative).