Prevention and treatment of optic neuritis
Ophthalmologists call neuritis a degenerative process that develops in the trunk and in various parts of the nerve membranes of the eye and has an inflammatory etiology. The pathology is detected in an acute form against the background of a decrease in immune function with simultaneous general or local damage to neurons by pathogens of a bacterial or infectious nature. Among the symptoms common to various types of damage, experts name a decrease in visual acuity, a violation of the contrast of color perception, the appearance of characteristic elements in the form of scotomas, and pain. Treatment of optic neuritis is based on the use of anti-inflammatory, decongestant, antiviral, antibacterial, immunostimulating and desensitizing drugs.
Causes of optic neuritis
When listing the causes of optic neuritis, experts emphasize that the pathology in most cases occurs due to the presence of infection in the body. When listing what causes optic neuritis, experts name among the main causes:
- The presence of inflammatory lesions in the brain area, such as meningitis, arachnoiditis or encephalitis.
- Multiple sclerosis.
- Pathologies affecting the sinus area, such as tonsillitis, sinusitis, pharyngitis, tonsillitis or sinusitis.
- Dental diseases such as periodontitis or caries.
- Infection or mechanical damage to bone tissue located in the orbital area, such as phlegmon, periostitis and osteomyelitis.
- The development of infectious lesions of the body of a specific type, for example, diphtheria, typhus, ARVI, tuberculosis, neurosyphilis, gonorrhea.
- Autoimmune pathologies.
In addition to the listed causes of optic neuritis, in a significant number of cases the appearance of pathology is caused by inflammatory processes occurring in the eye area, for example, pathologies such as uveitis, iridocyclitis, choriodiditis.
Symptoms of optic neuritis
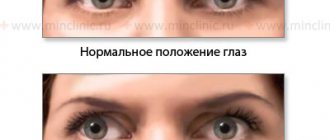
The diagnosis of optic neuritis is often made in patients who have rapid progression of the disease localized in the area of one eye. The severity of symptoms of optic neuritis depends on the form of pathology and the volume of tissue affected by the course of pathological changes. Depending on these factors, the patient may experience a wide range of symptoms, from deterioration of vision to the appearance of intraocular pain caused by increased pressure exerted by swelling to sudden loss of vision. Ophthalmologists distinguish characteristic signs of the disease for retrobulbal and intrabulbal varieties:
Among the features of the intrabulbal variety of the disease, experts include the dynamic development of symptoms that appear a few days after the lesion and last on average for 20-40 days. With this type, the patient may experience the appearance of spots localized in the central part of the image, loss of the ability to distinguish certain shades and visual acuity, up to the onset of blindness in the affected eye.
In contrast, signs of optic neuritis in the retrobulbal form are diagnosed less frequently and manifest themselves mainly in the form of a noticeable decrease in visual acuity or loss of vision. This type of disease has a longer course, the average duration of which is from 5 to 6 weeks. During this time, the patient may experience an increase in body temperature, a feeling of general weakness, migraines, a narrowing of vision in the peripheral vision area and the appearance of pain, the area of which is localized in the brow ridges.
Possible causes of eye pain and their symptoms
Discomfort and pain in the eyes are common. This symptom can be encountered after working for a long time at the monitor, reading in poor lighting, or when foreign particles enter. The pain can be sharp or aching, appear on the front or back of the eyeball, occur spontaneously or at a certain time of the day. With more serious pathologies, it will be accompanied by a decrease in visual acuity and can lead to its complete loss.
Foreign body entry
Pain in the eye area can also occur in healthy people. The membranes of the eyeball are very sensitive, and the entry of a foreign body into the conjunctiva causes its damage. This can be determined by characteristic features:
- severe pain in one or both eyes;
- profuse lacrimation;
- redness of the conjunctiva.
When a foreign body enters, profuse lacrimation usually begins. This is a reflex defense mechanism - it is necessary to flush out small particles that cannot be removed mechanically. In this case, it is recommended to rinse the eye with plenty of liquid, being careful not to irritate the mucous membrane.
Dry eye syndrome
Another cause of eye pain is a decrease in the secretion of the lacrimal glands. Normally, fluid is constantly formed and protects the mucous membrane from drying out. Dry eye syndrome is manifested by redness of the conjunctiva, a feeling of pain and stinging, discomfort and decreased visual acuity. This phenomenon can occur in any person, but several categories are at risk:
- office employees who spend working hours behind a monitor;
- aged people;
- those who work with welding machines;
- persons who live in hot climates, high dust or air pollution.
To treat dry eye syndrome, medications are prescribed that are analogues of natural tears. They have a similar chemical composition and are available in the form of eye drops. They can be used as needed throughout the day. Additionally, gymnastics will be useful.
Corneal erosion
The cornea is the outer layer of the eye's outer layer. It is a thin transparent film in which the primary refraction of rays occurs. It can be injured by irritation by mechanical or chemical means, as well as due to inflammatory processes. Other factors that can cause this symptom are improper eyelash growth and ill-fitting contact lenses.
Corneal erosion is a damaged area of the cornea. It can be identified by characteristic redness, severe pain in the eyes, lacrimation and photophobia. The healing rate of erosion depends on its depth and size. In most cases, it passes without consequences, but can also lead to loss of vision.
Barley
Barley (hordeolum) is an inflammation of the hair follicle of the eyelash, sometimes the sebaceous or meibomian glands. A painful lump appears on the eyelid, the skin turns red, and swelling may occur. The main cause of this disease is a pathogenic infection in combination with other factors (weakened immune defense, cold eyes). In most cases, the causative agent is staphylococcus.
A chalazion is a type of stye that is caused by inflammation of the meibomian gland duct. It is also called an internal or cold stye, as well as a meibomian cyst. The disease is characterized by a slow course (1-2 months), occurs with inflammation of the eye cartilage and the appearance of dense swelling. It may disappear on its own, but in some cases (if it is pressing on the eyeball) it is recommended to remove it during a simple operation.
Glaucoma
Glaucoma is increased intraocular pressure. It occurs when the circulation of fluid in the chambers of the eye is disrupted and its accumulation occurs. As a result, there is a risk of damage to the optic nerve, loss of elasticity of the membranes and gradual loss of vision. This disease is accompanied by pressing pain in the eye area and visual field defects. Over time, it can lead to complete blindness. An acute attack of glaucoma is a hard eyeball with a pupil that does not respond to light stimuli. There is also a headache that presses on the eyes.
Blepharitis
Blepharitis is inflammation of the eyelids. The process may be associated with mechanical damage to tissues, as well as with the action of fungal or bacterial microflora. Depending on the cause, there are several types of blepharitis:
- simple (aseptic, non-purulent);
- seborrheic - develops under the influence of a fungus, while the eyelid becomes covered with scales, crusts, and ulcers;
- staphylococcal - ulcerative blepharitis;
- demodicosis - its causative agent is a subcutaneous mite, the inflammation is accompanied by severe itching;
- allergic - most often occurs symmetrically (if the allergy is caused by eye drops or detergent, a one-sided reaction is possible);
- Rosacea-blepharitis (acne) - the skin of the eyelids becomes covered with a rash. filled with purulent contents.
With blepharitis, the skin of the eyelid is inflamed, swollen, and pain appears, radiating to the eye. In the acute form of the disease, it can occur in the form of barley or with the formation of subcutaneous cysts. In some patients, prolonged blepharitis can lead to decreased visual acuity. Treatment is prescribed individually, depending on the cause of inflammation.
Conjunctivitis
Conjunctivitis is an inflammation of the mucous membrane of the eye (conjunctiva). It can develop from fungal, viral, bacterial diseases or have a non-infectious origin. There are several main types of conjunctivitis:
- bacterial - most often caused by streptococcus aureus, accompanied by redness of the eyes, excessive flow of tears and photophobia, small hemorrhages appear on the mucous membrane;
- adenoviral - occurs with the release of pus and the formation of small follicles;
- hemorrhagic - in addition to eye pain, hemorrhages (bleedings) on the conjunctiva and on the eyelid become a symptom;
- fungal;
- allergic - may be accompanied by additional clinical signs and inflammation of varying severity.
According to the form of the course, acute and chronic conjunctivitis are distinguished. In the first case, it develops suddenly and begins with severe pain in the eye area. The acute stage lasts no more than a week. The chronic course is protracted, accompanied by discomfort, redness of the mucous membranes, and a feeling of the presence of a foreign body in the eye.
Keratitis
Keratitis is an inflammation of the cornea of the eye. The process can be of bacterial, fungal, viral origin, or develop due to injuries and mechanical damage to the shell. If the cornea is normally transparent and can transmit light rays, when it becomes inflamed, it becomes cloudy. The most dangerous is the protracted course of keratitis - it can lead to vascularization of the cornea, that is, the growth of blood vessels through it. This pathology is accompanied by a decrease in visual acuity. Keratitis causes acute pain in the front of the eye, photophobia, and lacrimation.
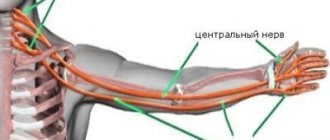
Pain in the eyes due to inflammation of the optic nerve
Inflammation of the optic nerve is a dangerous pathology that leads to rapid loss of vision. The process is accompanied by demyelination of nerve fibers, that is, destruction of the myelin sheath and loss of the nerve’s ability to conduct impulses. As a result, visual objects cannot be analyzed in the brain.
The causes of optic neuritis can be:
- inflammatory diseases of the meninges;
- acute intoxication;
- diseases of the inner membranes of the eye;
- systemic infectious diseases (influenza, tonsillitis, smallpox, malaria and others);
- systemic non-infectious diseases (hematopoietic pathologies, diabetes, gout and others);
- multiple sclerosis;
- injuries.
With optic neuritis, acute pressing pain appears in the eyes, the main focus of which is located behind the eyeball. The sensations intensify when pressing on it. There is also a narrowing of the field of view. Treatment takes place in a hospital and is aimed at eliminating the cause of neuritis and restoring nerve conduction. Its effectiveness depends on the timeliness of medical care.
Migraine
Migraine is an attack of headache. It begins abruptly and can last from several hours to several days. Painful sensations are often localized in the frontotemporal part of the head, but can spread to its entire surface. The exact cause of this phenomenon is unknown, but there is a relationship between migraine and traumatic brain injuries, nervous and endocrine disorders, and a genetic predisposition is also determined.
Classic migraine begins with additional symptoms (aura). Before the headache appears, discomfort also occurs in the eye area. Photophobia and deterioration of visual acuity may be observed.
How to treat optic neuritis
Depending on the area of localization of the disorder, ophthalmologists distinguish several types of the disease that arise as a result of local damage to the organ, leading to inflammatory processes, the development of which causes necrotization of damaged tissues. In order to determine a strategy for how to cure optic neuritis, the disease is diagnosed, based on the results of which the ophthalmologist hospitalizes the patient and prescribes a comprehensive treatment plan. Before treating optic neuritis, diagnostic procedures determine the etiology of the disease, depending on which the doctor can prescribe therapy using:
- anti-inflammatory medications;
- drugs that correct the functioning of the immune system;
- medicines from the group of antibiotics, with the exception of medicines from the group of aminoglycosides;
- corticosteroids;
- antiviral agents;
- drugs that regulate metabolism;
- antibacterial drugs;
- vitamin therapy using biologically active substances of group B;
- desensitizing drugs;
- medications intended to improve blood microcirculation;
- antispasmodics.
When it is established that the body is damaged by one of the types of infection, localized in the nasopharynx, respiratory organs or other structures, in addition to the course of treatment for optic neuritis prescribed by the doctor, the causes that caused the appearance of the background disease are eliminated.
Kinds
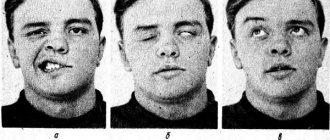
Depending on which part of the optic nerve has undergone inflammation, three types of neuritis are distinguished: neuritis (neurochorioretinitis), retrobulbar neuritis and opticochiasmatic arachnoiditis:
- Neuritis, or neurochorioretinitis. The inflammation is localized to the disc, or head, of the optic nerve, otherwise known as the blind spot. The optic disc does not have photoreceptors that sense light, but it is located on the fundus of the eye and is the site where the optic nerve exits the eyeball. The main symptoms of the disease are a sharp and rapid decline in vision and deterioration in color vision. After examination, hyperemia of the eye disc becomes obvious, in which the arteries in the center are narrowed, and the veins twist and dilate, blurred boundaries, vasodilation and a slight degree of prominence (protrusion) of the disc into the vitreous body. In advanced cases, there may be internal hemorrhages - in the disc or retina.
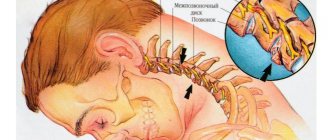
- Retrobulbar neuritis. The focus of inflammation in retrobulbar neuritis is on the orbit, outside the orbit in the cranial cavity. During the disease, patients feel constant pain, since the inflammation also affects the especially sensitive part of the orbit - the tendon ring, which is the beginning of almost all the muscles of the eyeball. It is characterized by a sharp decrease in vision and problems with color perception. It is within the framework of retrobulbar neuritis that the diagnosis of multiple sclerosis (MS) is often made. It is considered one of the earliest signs of MS, and also the most unstable - the disease can develop up to partial blindness, recover under the influence of therapy, but this cycle can be repeated several times.
- Optico-chiasmatic arachnoiditis. It occurs as a result of the transition of inflammation from the meninges to the nerve and chiasm. It is characterized by inflammation of the chiasm, the center of intersection of the visual fibers coming from the retina and the intracranial nerve located near the base of the brain. Optico-chiasmal arachnoiditis is characterized by mild hyperemia and mild swelling with narrowing of the visual fields. This is the most severe neuritis in terms of symptoms and clinical picture, which lasts for quite a long time.
In case of ordinary and retrobulbar neuritis, the examination is carried out by a neurologist and an ophthalmologist, and in case of opticochiasmatic arachnoiditis, treatment is carried out mainly in neurosurgical clinics under constant supervision. The doctor may also prescribe hospitalization.
Stages and degrees of optic neuritis
Ophthalmologists distinguish several types of pathology, differing from each other in the reason that caused the appearance of the disorder. In addition, experts distinguish such stages of optic neuritis as:
- Intrabulbal neuritis, a distinctive feature of which is a change in the shape of the optic nerve head and the spread of the inflammatory process not extending beyond the apple, is distinguished by the fact that it is most common in young patients.
- The combination of the previous type of lesion with degenerative changes occurring in the area of the nerve endings of the retina is observed quite rarely and is usually a consequence of an infectious or viral lesion.
- Retrobulbal neuritis is observed in a significant percentage of cases associated with multiple sclerosis. This type of pathology is characterized by the fact that in the initial stages it does not allow recording visual changes in the optic nerve disc, which is observed as the disease progresses at the stage of the nerve leaving the orbit.
Ophthalmologists emphasize the conventionality of distinguishing the degrees of optic neuritis, since due to various combinations of necrotization processes and inflammatory tendencies, the difference between the listed types of pathology can be conditional.
Methods for diagnosing optic nerve neuritis
Due to the strong similarity of symptoms of different types of disease, conducting competent, timely diagnosis is very important. Modern ophthalmology has the following methods:
- Clinical assessment of the patient’s eye condition - it involves an initial examination and collection of data about the patient’s life and illness. In this way, the possibility of the occurrence of infectious or another type of neuritis is established.
- Ophthalmoscopy is a way of examining the fundus of the eye using special instruments. It allows you to differentiate pathology and assess the condition of the retina, optic nerve head or blood vessels.
- MRI - using magnetic resonance imaging, tomographic images of the optic nerve are obtained, allowing one to draw a conclusion about its changes (thickening or dystrophy) and suspect the initial stage of multiple sclerosis.
It must be remembered that an effective diagnosis of inflammation of the optic nerve can only be carried out by an experienced specialist with a timely visit to the clinic.