Treatment methods
How to treat inflammation of the brachial nerve? Treatment consists of pain control, nerve healing, and rehabilitation.
Some methods to reduce pain include steroids, narcotic medications , to stabilize the nerve membranes and control discomfort.
Proper rest and reduced physical activity are also recommended to relieve inflammation and pain.
It will take some time for complete recovery. Physical therapy and rehabilitation will be needed in some severe cases to restore arm movement , but worse outcomes can be avoided with timely diagnosis and treatment.
In extremely rare cases where symptoms worsen with conservative treatment, your doctor will recommend surgery to correct the problem. This is done only after unsuccessful therapy for two years.
The surgical procedure will involve correcting the damaged nerves so that they begin to function normally.
What does it represent?
Brachial neuritis is a condition of sudden pain in the shoulder and arm , accompanied by weakness or numbness.
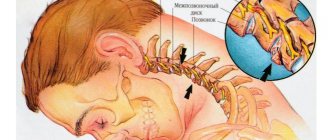
Caused by inflammation of the brachial plexus, formed by a combination of nerve roots emerging from the cervical spine into the neck.
Although the intense pain usually subsides within a few days, it is followed by some numbness and weakness in the arm and/or shoulder that may last for many months.
ICD-10 code
Neuritis in the ICD classification is not very precisely defined. In any diagnosis, it is important not just to collect a list of symptoms, but also to find out the exact cause of their origin.
In difficult cases, doctors use the coding M79.2 - neuralgia and neuritis not specified, neuritis NOS.
Etiology of inflammation in the shoulder joint
Neuritis is a general term that refers to diseases involving inflammation of a single nerve or group of nerves.
Brachial neuritis primarily affects the lower nerves of the brachial plexus, arm, and hand. This is caused by various conditions.
The reasons are as follows:
- Autoimmune disorders in which body tissues mistakenly attack the immune system. Sometimes these disorders can affect the nerves.
- The disorder may be the result of a mutation in a gene that affects skeletal development.
Symptoms of brachial plexus neuritis that begin in childhood are often the result of this genetic disorder. - The brachial plexus nerves pass through foramina in the cervical spine.
These endings can suffer trauma, such as falls, wounds or sports injuries. Another common sports injury, known as the "burner" or "sting", occurs primarily in football players. Direct blows direct the shoulder down and the neck in the opposite direction, stretching and compressing the nerves. - Tumors that develop in the neck or upper shoulder can compress the cervical nerves. They lead to intense pain, muscle weakness and numbness of the brachial nerve.
- Some babies are born with abnormalities of the humerus due to injury sustained during childbirth. Some experts think of it as damage to the nerves of the hand during childbirth. Such injuries usually disappear over time. Sometimes, there is a need for physical therapy.
- There is an extremely rare genetic form of the disease called hereditary neuralgic amyatrophy, which has a known cause of genetic inheritance and usually recurs on a regular basis.
Indirect causes of the disease:
- stress;
- diabetes;
- age-related disorders of the vascular system.
Causes of a pinched nerve in the shoulder
A pinched nerve can occur for several reasons, but it occurs when a nerve fiber is compressed by nearby tissue. As a result, the nerve bundle may become inflamed, leading to swelling. In most cases, the lesion affects the axillary, radial and median nerves. Among the most common factors that provoke the appearance of the disease are:
- degenerative-dystrophic diseases of the spinal column (in particular, osteochondrosis and arthrosis);
- complex diseases of the musculoskeletal system (for example, herniated discs);
- abnormalities in the functioning of the endocrine system (obesity). Excess weight puts increased pressure on muscles and nerves, which significantly increases the likelihood of illness;
- rheumatoid arthritis. The disease damages nerves over time, increasing the risk of pinching. The resulting bone spurs can lead to limited space for the nerves of the shoulder, which provokes the disease;
- various injuries (bruises, dislocations, fractures);
- prolonged walking on crutches;
- pathologies of the central nervous system;
- sedentary lifestyle;
- inflammation of the synovial bursa (bursitis);
- connective tissue dysplasia;
- excessive physical stress on the shoulder during sports;
- unsuccessful injections into the shoulder joint;
- infectious pathologies (for example, tuberculosis and syphilis);
- neoplasms in the shoulder and armpit area (both benign and malignant);
- damage to the acromial joint;
- increased and prolonged load on the shoulder joint;
- chronic lead poisoning;
- complications after surgical interventions (presence of adhesions or scars).
3. Neurosurgical treatment
Restoration of the damaged brachial plexus is carried out surgically - by the method of neurolysis
. This operation is most effective if performed within 6-8 months after the injury. If this period exceeds 18 months, the effectiveness of neurosurgical treatment is significantly reduced due to the developing Wallerian degeneration of nerve fibers.
If the diagnostic results reveal a neuroma, then it is excised during the operation. This is a microsurgical effect (endoneurolysis). If necessary, autograft
(nerve fibers taken from the lower leg, chest, etc.). The same technique, called “neurotization,” is used when the root is torn from the spinal cord trunk.
About our clinic Chistye Prudy metro station Medintercom page!
Damage to the radial nerve due to a fracture of the shoulder
Classification of mechanisms of injury to the brachial plexus.
Just as with injuries to other peripheral nerves, open and closed injuries to the trunks of the brachial plexus and their branches are distinguished.
In peacetime, cut, chopped and stab wounds of the trunks of the brachial plexus predominate. However, with the increase in crime, the number of gunshot wounds has increased. These are not only accidental shot wounds from a hunting rifle, but also wounds from bullets and fragments from explosions.
Gunshot wounds are characterized by severity and extensiveness, which is due to both high speed and the transfer of large kinetic energy of the wounding projectile to tissues. Iatrogenic damage to the trunks of the brachial plexus during erroneous surgical interventions.
The mechanism of closed injuries to the nerve trunks of the brachial plexus is mainly traction as a result of tearing, stretching with rupture of a different number of bundles. The traction mechanism of injury leads to damage to the nerve trunks over a large area, often the trunks are torn out of the intervertebral foramina, and the roots of the cervical thickening are torn off from the horns of the spinal cord.
A common cause of closed injuries to the trunk of the brachial plexus are road traffic accidents, among which the leading place is occupied by motorcycle trauma. In second place is a group of industrial and domestic injuries: falling from a height, getting a hand pulled into moving and rotating mechanisms, blows to the shoulder girdle from falling heavy objects. Often, traction injuries to the trunks of the brachial plexus rarely occur as an isolated injury, most often it is a consequence of polytrauma (78.3%).
Providing care and treatment of patients with multiple and combined injuries is associated with great difficulties associated with the severity of the general condition of the patients (mutual burden syndrome) and the difficulties of diagnosis.
Classification of conduction disorders of the nerve trunks of the brachial plexus.
1. Complete disruption of conductivity. 1.1. Clinical and neurological symptoms. 1.1.1.Flaccid paralysis of the corresponding muscles and their progressive atrophy 2-3 weeks after the injury. 1.1.2.Anesthesia, anhidrosis, lack of skin folding during a thermal test, an increase in skin temperature in the first 2-3 weeks followed by a persistent decrease in case of damage to the C8 and T1 spinal nerves or the lower trunk in the area of the median and ulnar nerves. With isolated injuries of the upper and middle trunks, anesthesia is not observed. 1.1.3. Pain on palpation of the area of the intervertebral foramina, possible presence of neuromas (especially with open injuries). 1.1.4. With high preganglionic levels of damage – Horner’s syndrome and the presence of traumatic meningoceles on myelograms or CT and MR tomograms; 1.1.5. Painlessness upon percussion along the projection of the nerves, absence of pain upon palpation of the muscles. 1.2. Electrophysiological signs: 1.2.1. Absence of muscle contraction and M-response when irritated by current of the brachial plexus trunks. 1.2.2. Complete reaction of degeneration of paralyzed muscles. 1.2.3. Absence of bends in the “intensity-duration” curve and a sharp increase in the threshold at durations of electric current pulses less than 10-5 ms. 1.2.4. Absence of electrical excitability of muscles (with concomitant damage to the great vessel and long periods that have passed since the injury). 1.2.5.Bioelectric silence or denervation potentials with electromyography. 1.2.6.Increasing skin resistance to alternating current over 1 MOhm, direct current over 15-17 MOhm. 1.2.7. Increase in skin temperature in the first 2-3 weeks after injury, followed by a persistent decrease by approximately 1.0-2.5 degrees Celsius.
2. Deep conduction disturbance. 2.1. Clinical and neurological symptoms: 2.1.1. Paresis of the corresponding muscles (1-2 points) with their atrophy or severe malnutrition. 2.1.2. Hypoesthesia (1-2 points) with areas of hyperpathy, lack of discriminatory sensitivity and stereognosis. 2.1.3. Pain on palpation of the intervertebral foramina, possible presence of neuromas. 2.1.4. Pain on percussion along the projection of the nerves and pain on palpation of paretic muscles. 2.2.Electrophysiological signs can be the same as with complete disruption of conduction, or: 2.2.1.Partial reaction of degeneration of paretic muscles. 2.2.2. Presence of bends in the “intensity-duration” curve, but with a sharp increase in the threshold at durations of electric current pulses less than 50 ms. 2.2.3. Combination of denervation and “born” potentials during electromyography.
3.Partial conduction disturbance. 3.1. Clinical and neurological symptoms: 3.1.1. Strength of the corresponding muscles up to 3-4 points, their moderate hypotrophy. 3.1.2.Hypostisia 3-4 points, the appearance of discrimination of two points less than 40 mm in the autonomous zones of the median and ulnar nerves, the appearance of stereognosis (it should be remembered that all other nerves of the upper limb do not have autonomous zones of sensitivity, and therefore even their complete anatomical break is not accompanied by anesthesia in the areas of their innervation). 3.2. Electrophysiological signs: 3.2.1. Partial reaction of muscle degeneration. 3.2.2. Bends and approximations to the norm of the “intensity-duration” curve. 3.2.3. When the trunks of the brachial plexus are irritated by electric current, muscle contractions and an M-response are noted. 3.2.4. Decrease in amplitude and purity of action potentials during electromyography.
Classification of brachial plexus injuries by topographic level.
Intraspinal, radicular or preganglionic injury to the brachial plexus, C5-C8-T1 spinal nerves arise from the anterior and posterior horns of the spinal cord by two roots: dorsal, posterior, sensory and ventral, anterior, motor. Both roots approach each other and unite into one common trunk of the brachial plexus, emerging from the spine through the intervertebral foramen. Posteriorly laterally, slightly distal to the place where the key plexus unites into a common trunk, the posterior sensory root thickens in the form of a spinal or intervertebral ganglion, which is not related to the anterior motor root.
Clinically, along with other important aspects, the following are revealed:
- paralysis of the paravertebral muscles, which are innervated by the dorsal, posterior branches of the spinal nerves;
- paralysis of the muscles that control the scapula: serratus, rhomboid;
- conduction disorders of the spinal cord; Claude Bernard-Horner syndrome.
2. Trauma to the supraclavicular part of the brachial plexus - postganglionic damage to the brachial plexus after exiting the intervertebral foramen, where the C5-C6 spinal nerves are fixed by connective tissue membranes. The mechanism of injury is a blow to the shoulder girdle during a fall or a falling object from above with a sharp dilation of the angle between the neck and the shoulder girdle and the head moving backward and in the opposite direction.
More often, part of the brachial plexus is separated in the interscalene space, approximately at the level of formation of the upper trunk of the brachial plexus. Less commonly, the middle trunk of the brachial plexus is affected.
3. When the brachial plexus is damaged in the clavicular region, the secondary trunks are affected, which are crushed or can be crushed in the space between the clavicle and the first rib. The main mechanism of injury is a direct blow to the collarbone with its fracture and to the area of the shoulder girdle, shoulder, or a sharp lowering of the shoulder joint. Subclavian lesions cause damage to secondary trunks and their branches and nerves. The mechanism of injury differs in that bony injuries to the clavicle are often the direct cause of their injury.
Diagnostic methods
The inflamed ending is treated and diagnosed by a neurologist . The diagnosis is made after a lengthy review of the patient's medical history and physical examination. A detailed medical history was obtained, followed by clinical and neurological examination.
In some cases, treatment is not required. In other cases, treatment involves symptomatic management of the condition.
To diagnose the disease, the following studies are carried out:
- Blood analysis.
- Lumbar puncture: This is done to test the cerebrospinal fluid.
- EMG: Since the symptoms of this disease are similar to those of cervical radiculopathy, an electromyogram will help differentiate them.
It measures the speed and strength of transmitted signals. - Nerve biopsy: This is a common procedure to confirm the diagnosis.
A piece of the affected nerve is taken and sent to a pathologist for examination. - Radiological examinations of the inflamed nerve: Radiological examinations include MRI, CT and X-rays of the affected area.