Everyone knows that the surface of the brain should be covered with convolutions. Pictures of a normal brain are even in school textbooks. However, there are situations when there are significantly fewer convolutions than there should be, and they are smoothed out. It also happens that there are no convolutions at all. In such cases, the brain is “smooth”, this is its main external difference from normal. In fact, a smooth brain is a serious disorder that is incurable. Olga Pylaeva, a neurologist and epileptologist at the Institute of Child Neurology and Epilepsy named after A.I. St. Luke .
Brain malformations: polymicrogyria, agyria and pachygyria
Polymicrogyria, agyria and pachygyria are congenital malformations of the brain, also called brain malformations.
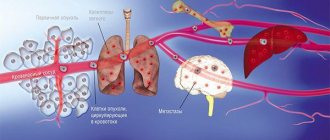
These anomalies arise as a result of a disrupted process of formation of the brain or its individual structures during the prenatal period, and represent abnormal changes in the structure of brain structures. There are no exact data on the prevalence of congenital brain defects, but polymicrogyria is considered the most common.
More details about each malformation:
Brain hygroma
Subdural hygroma of the brain (alternatively called hygromas) refers to the accumulation of fluid in the space of the same name. In many cases, it is considered an epiphenomenon of traumatic brain injury, called traumatic hygroma .
Subdural hygroma occurs in all age groups, but most often in older people. The vast majority of patients are asymptomatic. However some include:
- pain;
- mental status changes;
- nausea and vomiting;
- focal neurological disorders;
- seizures.
The pathogenesis of cerebral hygromas is not fully understood. The most common explanation is that the arachnoid layer is ruptured, creating a ball valve opening that allows cerebrospinal fluid to pass unilaterally into the subdural space. Although this does not necessarily truly describe the underlying mechanisms. There is an assumption that cerebral hygroma sometimes presents as noticeable effusions in which there is a separation of the layer of border cells of the dura mater with accumulation of fluid.
Epidural hygroma also occurs due to compression within the skull, which is accompanied by intracranial hematomas. As a consequence of late diagnosis and treatment - depressed fractures of the skull bones, brain injuries, etc. MRI helps to find the source of the problem in advance, which can also detect an arachnoid cyst.
Hygroma on the head usually occurs along the supratentorial convexities; in the posterior fossa is rare. Hygroma of the parietal region and other parts radiographically appears as a crescent-shaped accumulation of density/signal near the cerebrospinal fluid, which does not extend into the sulci and rarely has a significant mass effect.
Since frontal hygroma , for example, is often asymptomatic without radiological evidence, neurosurgical intervention is rarely required. In cases where mass effect is demonstrated by head CT , it can be removed this way. This is how in most cases it is recommended to remove a child’s hygroma .
The relationship between chronic hygroma and subdural hygroma is complex and not fully understood. Almost certainly, a significant number of collections diagnosed as chronic hematomas represent a subdural hygroma of the same right parietal region or another area.
We recommend a clinic for hygroma removal in Moscow
Provoking factors
The main reason for the development of polymicrogyria, pachygyria and agyria is the incorrect process of neuronal migration, which is caused by:
Polymicrogyria can be caused by cytomegalovirus infection, insufficient oxygen saturation of the placenta, and mutations occur in the genes COL18A1 (21q22.3), PAX6 (11p13), K1AA1279 (10q22.1), TUBB2B (6p25), EOMES (3p21.3-p21.2 ), RAB3GAP1 (2q21.3), SRPX2 (Xq21.33-q23).
Agyria can occur due to viral infections that penetrate the uterus or fetus during the first trimester, insufficient blood supply to the fetal brain in the first months of pregnancy. Among the genetic factors are mutations in the RELN gene (7q22), genes of the X chromosome, and 17 chromosomes.
In pachygyria, mutations occur in the LIS1 (17p13.3) and DCX (Xq22.3-q23) genes.
Causes
The main causes of lissencephaly are mutations in one of several genes. The main genes in which mutations cause lissencephaly are known under the names LIS1, DCX (doublecortin), RELN (reelin, localized on chromosome 7) and ARX (the gene is localized on the sex X chromosome, in this case, in addition to the smoothness of the grooves, MRI reveals a congenital absence corpus callosum, the main structure that facilitates the exchange of information between the two hemispheres). These defects are usually absent in the genes of the parents and first appear in the fetus during pregnancy (so-called “de novo mutations”). In this case, the parents can be completely healthy.
The occurrence of mutations in genes during pregnancy is a random event, which can be provoked by a number of factors, including various toxic influences and taking medications that are toxic to the fetus. Also, the cause of gene breakdown can be infections or poor circulation of the fetus at the beginning of pregnancy. However, it is impossible to predict that this will be the result. In most cases, the cause of the mutation remains unknown. In this case, subsequent children of the same parents will most likely be devoid of this mutation.
It happens less often that one or both parents initially have such a (very rare) gene breakdown. At the same time, it practically does not appear outwardly and becomes a “surprise” after the birth of a sick child. In these cases, the risk of having other children in the family with such a rare genetic disease is quite high.
"A little alive." What happens to the human brain and body after death? More details
Characteristic symptoms
The following symptoms are characteristic of polymicrogyria:
Pachygyria manifests itself before the age of 2 years. Its main features are:
Agyria manifests itself by 3-5 months of a child’s life, less often by 8-9 months; the main symptom of the pathology is expressed in the rapid lag of the child in physical and mental development.
The anomaly may also manifest itself with the following symptoms:
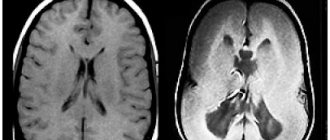
Cross-sectional photo of the brain and MRI of a child diagnosed with agyria
Establishing diagnosis
The following studies are used to diagnose brain malformations:
With polymicrogyria, the cerebral cortex is abnormally thin, and the subarachnoid spaces and ventricles of the brain are enlarged. Defeats
can be located on one or both sides, can be local or extensive. The cortex may appear abnormally thick due to the large number of small convolutions that coalesce to form thick, deep masses.
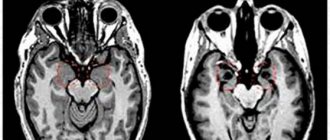
Pachygyria is determined by MRI results, which show thickening of the cerebral cortex, small gyri, and an underdeveloped Sylvian fissure.
In the prenatal period, it is possible to determine brain malformations using fetal ultrasound. If developmental abnormalities are suspected, they are referred for additional studies (MRI, genetic analysis of candidate genes).
Medicine is practically powerless
There are no effective methods for treating brain malformations in modern medicine. Therapy is aimed at relieving symptoms and maintaining the functioning of the body at an acceptable level.
For polymicrogyria and pachygyria, the following methods are recommended to alleviate the condition of patients:
For agyria, classical methods of therapy are considered ineffective: taking nootropic drugs, massage, physiotherapy.
Treatment with anticonvulsants and centrally acting muscle relaxants, which reduce tone in skeletal muscles, shows the greatest effectiveness.
Often epilepsy, which accompanies pathologies of brain development, turns out to be resistant to therapy, and then it is recommended to use a combination of two drugs.
Research is being conducted to treat these anomalies using stem cell transplantation and growth factor transplantation.
Treatment method
Any large brain tumor can be cured exclusively through surgery. Given the difficulty in identifying symptoms, it is advisable to go to the hospital if you have suspicions or prolonged headaches. Prolonged headaches, as well as generalized seizures, can indicate disturbances in the functioning of the brain. As the tumor size increases, intracranial pressure increases significantly. This may cause vomiting.
Treatment can be carried out exclusively by professional neurosurgeons after undergoing a full range of examinations. If severe symptoms appear, which appear due to active infiltration of tumor cells into surrounding structures or compression, urgent surgery is required.
Damage can be removed partially or completely. Tactics are selected individually, taking into account the location of the main vital centers in the brain. After completion of the surgical intervention, a rehabilitation period is required. At this time, nootropic drugs are used, as well as drugs aimed at restoring affected functions.
Depending on the location of the disease, rehabilitation procedures are prescribed separately. Among them are massage, physical therapy complex, taking pharmacological drugs and much more.
Prognosis and life expectancy
Patients with polymicrogyria who have mild forms of the pathology can survive into adulthood. In severe forms, death occurs at an early and young age due to pneumonia or seizures.
There is no single prognosis for patients with pachygyria. It can vary in each specific case and depends on the severity of the brain pathology and the intensity of the symptoms. But usually children with pachygyria live no longer than 20 years.
Underdevelopment of the brain in children with agyria is irreversible and the prognosis is unfavorable. Most patients do not survive beyond the age of 5 years. All patients have complete disability.
Due to depressed swallowing reflexes, tube feeding is often required. Death can occur due to diseases that occur against the background of the underlying pathology: intestinal paresis, cardiovascular failure, respiratory failure, atrophy of the respiratory muscles, hypostatic pneumonia.
Source
Treatment
This malformation does not have any effective treatment. All measures and procedures are reduced to palliative treatment, which allows maintaining the basic functions of the body.
Recently, attempts have been made to treat this disease using stem cell transplantation, or growth factors. But, as practice shows, in not a single case was it possible to achieve recovery, and such types of treatment only allow the situation to stabilize for a short time.
In addition, given the poor prognosis and very high risk, treatment such as stem cell transplantation is almost never carried out due to the very unfavorable risk/benefit ratio.
Classic treatment regimens from neurologists, in which nootropic drugs, physiotherapy, and massage are prescribed, do not have an effect. The only treatment that really helps in any way is taking anticonvulsants and prescribing centrally acting muscle relaxants to reduce skeletal muscle tone.
None of the babies with this diagnosis were able to learn to walk in their short lives. Almost none of them can recognize their loved ones, despite the most intensive treatment.
Forecast
The prognosis for life is unfavorable. Most die in early childhood; a few live to 3-5 years of age, remaining deeply disabled. Death occurs from the development of intercurrent diseases (hypostatic pneumonia, atrophy of the respiratory muscles, intestinal paresis). Sometimes children require lifelong tube feeding due to suppressed swallowing reflexes. Due to the underdevelopment of other parts of the brain and many internal organs, the cause of death can also be acute respiratory and cardiovascular failure.
In conclusion, it should be noted that the only cure for this disease today is genetic consultation of parents at the pregnancy planning stage, and careful monitoring of their health by future parents.
Pachygyria brain symptoms
Terms microgyria
and
polymicrogyria
(PMG) describe pathological changes in the cerebral cortex, represented by many short, shallow gyri, forming a pathological pattern that can vary macroscopically. In some cases, when assessing the surface of the brain, the broad gyri are difficult to distinguish from areas of pachygyria, but the cortical ribbon has a typical polymicrogyric appearance with fusion of molecular layers (Friede, 1989, Harding and Sorr, 1997). Microgyria can be generalized, unilateral, multifocal and focal.
There are two main histological types of polymicrogyria (PMG), but transitional or mixed forms often occur. The most common unconditioned developmental disorder is microgyria with undivided layers (Ferrer, 1984, Harding and Sorr, 1997), in which there is a single wavy cell layer between the white matter and the molecular layer.
In classic four-layer microgyria, the first layer of small pyramidal cells, located below the molecular layer, is separated by a low cellular layer from a deep layer containing large pyramidal cells. The low cellular layer corresponds to normal layers IV and V, with which it merges at the boundaries of the microgyric cortex (Williams and Caviness, 1984, Evrard et al., 1989). This phenomenon allows us to suggest that post-migration disorders occur in the fifth or sixth month of pregnancy with secondary laminar necrosis developing as a result of circulatory failure and hypoxia. This interpretation is supported by the fact that classical PMG develops due to pathological events occurring after the middle of the current pregnancy, such as severe trauma, carbon monoxide toxicity or maternal asphyxia (Larroche, 1986, Barth, 2003b), and only in one of the monozygotic twins (Sugama and Kusano, 1994). Evrard et al. (1989) identified two peak periods for circulatory failure: between 20 and 24 weeks and during the last 10 weeks of gestation.
Insufficient blood flow may also be responsible for microgyria in fetal infections (Marques-Dias et al., 1984), which can cause vascular damage (Barkovich and Lindan, 1994) or circulatory failure, as well as porencephalic defects. However, individual PMGs can form shortly before the end of the migration processes and arise as a result of the death of the surface layers, damaging the glial conductors before the late migrating cells complete the migration process (Dvorak et al., 1978). In these cases, neurons arrested in the process of migration are identified under areas of microgyric cortex (Lyon and Beaugerie, 1988, Evrard et al., 1989). Several familial, probably genetically determined cases have been reported.
Isolated cases involving large deletions of the critical region of chromosome 22q11.2 have been described (Bingham et al., 1998, Worthington et al., 2000), with the suggestion that this may be a contributing factor in the occurrence of PMG. Other rare types of PMH have been identified in Zellweger syndrome (Raoul et al, 2003) and in other unusual syndromes such as Dellemann's syndrome (Moog et al., 2005, Pascual-Castroviejo et al., 2005).
Magnetic resonance imaging (MRI) in St. Petersburg
With MRI in St. Petersburg, we specifically look for abnormalities of the cerebral cortex in epilepsy and developmental delays. Disorders of cortical development can be an isolated developmental anomaly, or combined with other developmental disorders, such as regionalization disorders. Disorders of cortical development are determined by MRI of the brain and can be divided into:
Proliferation and differentiation disorders – microcephaly, megalencephaly
Migration disorders – agyria-pachygyria (lissencephaly), polymicrogyria, heterotopia
Disorders of the organization of the cortex - microdysgenesis
Megalencephaly is an enlargement of one or both hemispheres of the brain. With megalencephaly, MRI reveals an enlarged lateral ventricle on the corresponding side, the cortex is thickened and not divided into convolutions (agyria), and the white matter is not myelinated.
MRI. T1-dependent coronal tomogram. Agiriya.
Heterotopias. During embryogenesis, neurons may not reach their destination in the cortex. Most migration disorders have a dominant X-linked origin. Anomalies can be local or diffuse. Diffuse heterotopias are localized periventricularly. Gray matter, according to MRI, accumulates only around the lateral ventricles, without affecting the areas around the third and fourth ventricles. In a quarter of cases, heterotopia is accompanied by anomalies of the corpus callosum and cerebellum.
If the neurons do not reach the cortex at all, lissencephaly occurs. If only some neurons do not reach it, then subcortical heterotopias appear, visible on MRI in the form of nodes or stripes (“double” cortex). Clinical symptoms are usually mild - slight developmental delay, pyramidal signs and, sometimes, dysarthria.
MRI. T1-dependent axial tomogram. “Double bark.”
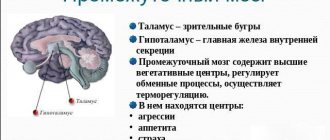
Focal (focal, nodular) heterotopias are also commonly called hamartomas. They occur as an independent anomaly or as a manifestation of tuberous sclerosis. On MRI, the signal from the nodes is typical of gray matter and they are typically not enhanced by gadolinium. This allows them to be distinguished from subependymal nodes in tuberous sclerosis. A special type of hamartoma is the hypothalamic hamartoma. It is located in the area of the gray tubercle, between the pituitary stalk and the papillary bodies. Hypothalamic hamartoma has an exophytic type of growth and reaches 12 mm. Clinically, it is asymptomatic or manifests itself in early maturation, acromegaly and a special type of partial epilepsy - convulsions in the form of obsessive laughter, as well as mental disorders. On T1-dependent MRI, hypothalamic hamartoma is isointense to white matter, on T2-dependent MRI it is slightly hyperintense. The formation is homogeneous and has a clear outline. The mass effect is expressed in the displacement of the pituitary funnel. Unlike astrocytoma of the same localization, hamartoma does not involve the optic chiasm. It is more difficult to distinguish a hamartoma from a meningioma, but the latter is enhanced by contrast. Ganglioglioma of the hypothalamus is rare. It contains cysts, sometimes microcalcifications (as seen on CT) and is enhanced with contrast in approximately half of the cases. Also rare are lipomas of the hypothalamus, which have a signal characteristic of adipose tissue.
Lissencephaly is a general term that refers to a disorder in the formation of sulci. Its extreme manifestation is the complete absence of convolutions - agyria. Gray matter is present, but it is not divided by fissures. Agyria can be local, usually this type is observed in the temporal lobe.
An abnormally small number of gyri due to incomplete sulci is called pachygyria. Usually, it is also local, the convolutions are wide and smoothed. The combination of areas of pachygyria and agyria is called lissencephaly type I. MRI reveals cortical thickening, vertical Sylvian fissures, and often straightened hippocampi . Clinical manifestations fit into various forms (Miller-Decker, Norman-Roberts syndromes, etc.), which appear in the first year of life. Type II is characterized by a violation of the structure of the cortex itself, which is penetrated by vessels and fibroglial bundles. This type is combined with hydrocephalus and incomplete myelination. A typical clinical manifestation is Walker–Warburg syndrome.
Polymicrogyria - multiple shallow gyri. Often combined with gray matter heterotopia and hemimegalencephaly. It is believed that the pathogenesis of polymicrogyria is associated with ischemic necrosis of the fifth layer of the cortex before the 20th week of embryogenesis. Some cases are associated with congenital cytomegalovirus infection.
In addition, polymicrogyria may be part of Aicardi syndrome, an X-related dominant pathology. It occurs in the form of spasms and chorioretinopathy. MRI often reveals cerebellar hypoplasia, agenesis or underdevelopment of the corpus callosum, cysts of the PCF and midline, and papillomas of the choroid plexus .
MRI. T1-dependent sagittal tomogram. Ecardi's syndrome.
MRI. T1-dependent coronal tomogram. Polymicrogyria.
Cortical microdysgenesis are responsible for some variants of extratemporal epilepsy and, apparently, for some mental pathologies. Only sometimes microdysgenesis produce changes at the macroscopic level, which are detected by MRI .
Cortical abnormalities are better seen in high fields than in open MRI. MRI of St. Petersburg makes it possible to study using MRI in different centers, but we advise looking for such complex pathologies only in specialized centers.
Leave feedback.
MRI in St. Petersburg USA